Journal of Emergency Medicine & Critical Care
Download PDF
Review Article
Thinking about Inking; Medical Alert Tattoos and Practical Implications of Their Use for Providers and Patients
Brito AMP1-3*
1University College Cork, National University of Ireland School of Medicine.
Brookfield Health Sciences Complex, College Rd, Cork, T12 AK54, Ireland
2Queen’s Medical Center, 1301 Punchbowl Street, Honolulu HI 96813
3Oregon Health and Science University, 3181 Sam Jackson Rd, Portland OR
97239
Address for Correspondence:
Brito AMP, Queen’s Medical Center, 1301 Punchbowl Street,
Honolulu HI 96813; E-mail: a.brito.26@gmail.com
Submission: 20 September 2022
Accepted: 10 October 2022
Published: 13 October 2022
Copyright: © 2022 Brito AMP. This is an open access article distributed
under the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original work
is properly cited.
Abstract
Objective: Medical alert tattoos (MATs) are under-recognized and
under-studied. The information contained in tattoos may be useful
for guiding patient management in emergent presentations such as
trauma and critical illness when the patient is unable to communicate.
However, use of MATs is fraught with medico-legal complexity as well
as reliability and safety concerns. This study aims to examine patterns
of use and develop recommendations for patients and providers.
Methods: An online survey was created for health care providers,
patients and tattoo artists regarding incidence, background
motivation, content of tattoos as well as providers’ experience with
and recommendations for their use. A literature review was performed
to examine the available evidence presented in previously published
case reports as well as historical, clinical, and ethical reviews.
Results: Allergies and chronic medical conditions were commonly
seen. Of the providers who had encountered a MAT 39% reported
that it had influenced patient management. Literature review showed
wide heterogeneity in the use of MATs by patients and providers.
Conclusion: Whether or not MATs are a good idea, patients
are using them to communicate medical information. Health care
providers should be aware of their use and the complex issues around
interpreting the information they contain.
Keywords
Tattoos; Health information; Advance directives; Emergency
care; Medical alert
Introduction
Tattooing: Tattooing is a popular format for body modification
that involves the deposition of pigments into the skin to create
permanent markings. Contemporary studies indicate that in the USA
and Europe 1/5 to ¼ of the population has at least one tattoo [1,2].
However, tattooing is far from a new concept. The earliest known
tattoo is about 5200 years old [3], and in ancient Egypt tattooing
was relatively common practice [4]. In the context of contemporary
western society, tattooing was popularized in Britain and America
during military campaigns with the prevalence of tattoos reaching as
high as 65% in members of the US Navy in World War II [5-8].
Tattoos in Medicine: Tattoos have been used in a variety of ways
in medicine. The presence of inked dots and lines over the lower back
and spine in a late Neolithic mummy in a pattern corresponding to
acupuncture sites has been theorized to indicate a possible therapeutic
intent of the tattoos themselves3, and in some parts of contemporary
West Africa tattoos are placed on the forehead to treat epilepsy or
hands and feet to treat peripheral neuropathy [9].
Tattoos may be used to cover scars or recreate the appearance of
normal anatomic structures such as nipple tattoos after mastectomy
or corneal iris tattoos in leucomata [10-14]. They may mark the site of
a colonoscopic biopsy allowing localization during surgical resection or the site of radiation therapy to ensure consistent localization
[15,16]. Ongoing studies are evaluating color changing tattoos as
continuous monitors of blood glucose for diabetics which may
facilitate recognition of hypoglycemic events [17].
Tattoos as a media for medical information have been in use
for more than half of the last century. Large scale blood type tattoo
programs were used in Germany in World War II for service
members, and US civilian programs during the cold war resulted in
thousands of adults and children receiving blood type tattoos [18].
In the military context medical and identifying tattoos with enlisted
person’s name, blood type, religion and other information are usually
placed on the flank [19]. These are sometimes referred to as “meat
tags” as part of their intent is to increase the chance of remains being
identified and sent home in the case of death in combat, as the torso is
frequently the largest portion of the body left intact after high energy
trauma.
The use of medical alert tattoos raises questions of safety,
accuracy, social concerns, and ethical/medico legal concerns. While
there are several case reports, small survey studies and popular media
articles there is need for a broader systematic approach to studying
these tattoos and the implications of their use for both patients and
medical professionals.
Methods
Review of case reports: A search was performed using the
PubMed database with search terms “medical alert tattoo”, “medical
tattoo”, “Do Not Resuscitate (DNR) tattoo”, “tattoo” and results
filtered for relevance. 14 studies were identified with specific case
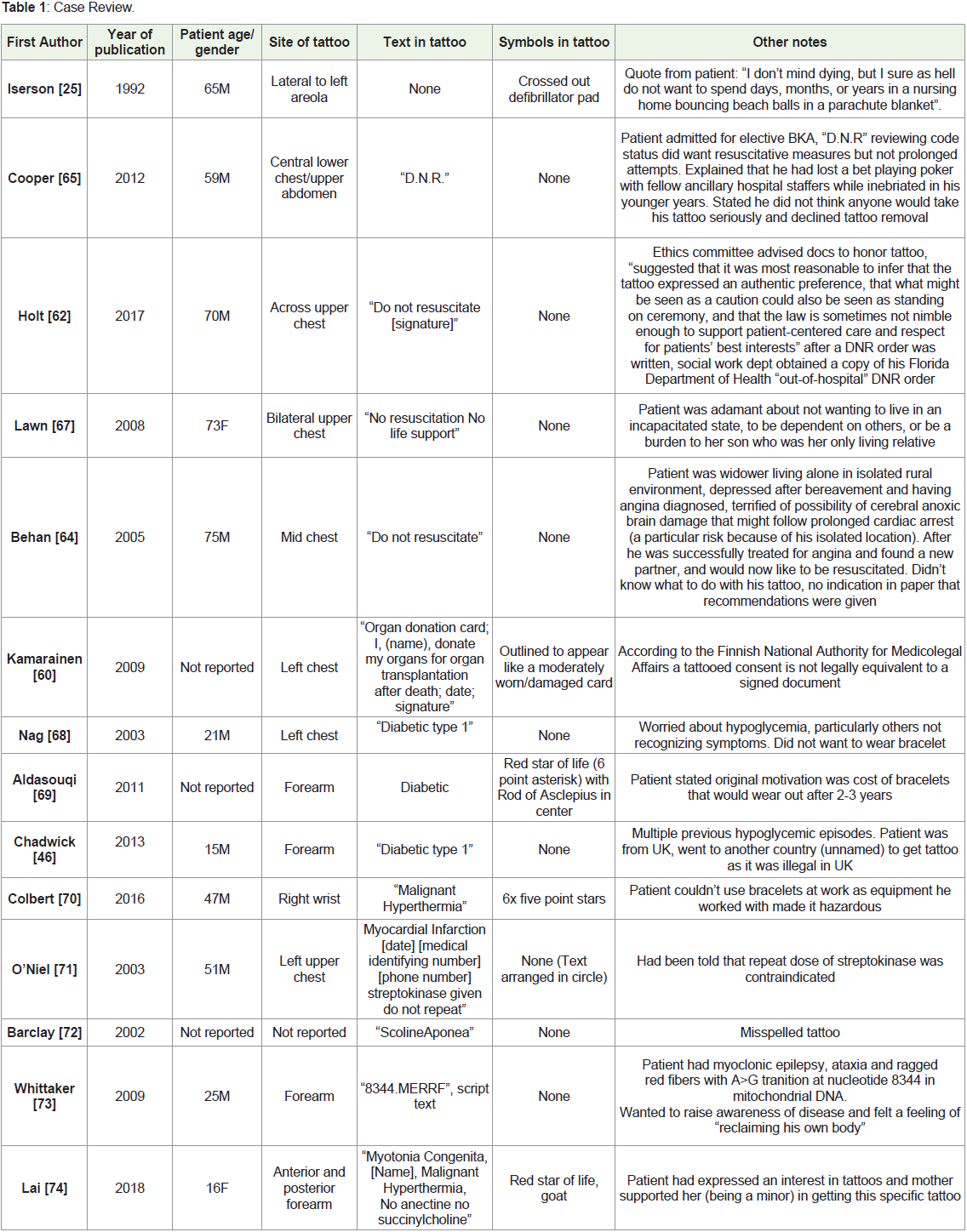
reports. The results are summarized in Table 1. Popular media articles
were not used for case review.
Survey: A survey was created with questions targeted to tattoo
artists, health care professionals, and patients with chronic medical
conditions with and without medical alert tattoos. Surveys were
designed to obtain maximal demographic and content information
as well as examine motivations and applications of these tattoos.
The tattoo artist survey focused on incidence of medical alert tattoos, content, and technical aspects of tattooing and tattoo aging.
The health care professional survey focused on experiences with
medical alert tattoos in practice as well as recommendations for use.
The patient survey focused on demographic information, medical
history as it pertains to tattoo content, text and symbol content of
tattoos, tattoo placement, motivations and attitudes about tattoos
as well as receptiveness to recommendations. The study and surveys
were reviewed and approved by the ethics board of the University
College Cork. The survey link was made available on a social media
site (Facebook) created for the purpose of this study with study
aims, safety and ethical information available. This was distributed
through a combination of sharing on other social media sites such
as tattoo artist interest groups, various medical groups, and health
care associated sites as well as through email between 2014 and
2019. There were zero responses from these methods for the tattoo
artist arm so surveys were printed and brought in person to tattoo
shops at various locations in the United States of America, Canada,
and Ireland. This allowed additional conversation about answers to
survey questions as well as various technical explanations of tattoo
techniques and limitations. Only two artists refused to complete the
survey when approached in person. The overall response rate was not
available as it was not possible to accurately quantify total reach given
the methods of distribution.
Results
Surveys: Survey respondents numbered 10 for tattoo artists, 14
for patients with medical alert tattoos, 20 for patients with chronic
health conditions but no medical alert tattoo, and 54 for health care
professionals.
Tattoo artists: 90% of tattoo artists surveyed had done a medical
alert tattoo. Artists surveyed had a range of 5-30 years’ experience
with a mean of 12 years. The number of tattoos done ranged from 0-50
with a mean of 10 and median 9. In terms of technical considerations
for tattooing, tattoo artists uniformly advocated simple text relative
to any form of cursive or fancy font as having greater longevity. Most
artists felt that the size of lettering to have good long-term legibility
would be around 1 inch or 2.5 cm although this would vary based on
experience and technique (for example, single needle vs multi needle).
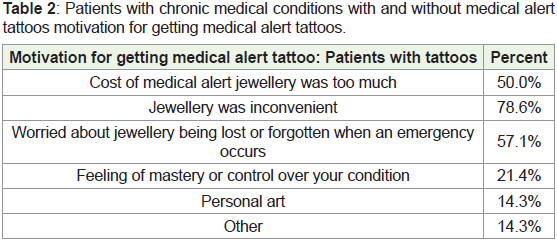
Patients with medical alert tattoos: 50% of patients with medical
alert tattoos surveyed were between the ages of 26-35. Almost all had
gotten their medical tattoo within the 5 years prior to responding to
the survey. 93% had previously used other media such as jewelry or
cards to keep their medical information on their person. Motivations
for getting a medical alert are summarized in the first portion of
Table 2. These patients had a range of 1-12 tattoos in total with 40%
having only one tattoo (the medical alert tattoo). Of those patients
with multiple tattoos, 22% had their medical alert tattoo placed near
other tattoos. 93% said that they would have considered following recommendations on content, design and placement for medical
alert tattoos provided by health care professionals if they had been
available at the time they got their tattoo.
Table 2: Patients with chronic medical conditions with and without medical alert
tattoos motivation for getting medical alert tattoos.
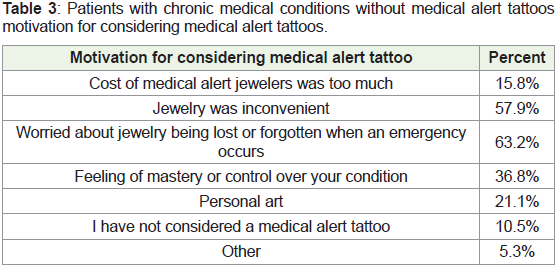
Patients with chronic health conditions without medical alert tattoos: 50% of patients in this category were between the ages of 36-
50. 90% have considered getting a medical alert tattoo. Motivations
for considering this option are listed in the second portion of Table 3.
90% would consider following recommendations for content, design
and placement if such recommendations were available from health
care professionals.
Table 3: Patients with chronic medical conditions without medical alert tattoos
motivation for considering medical alert tattoos.
Health Care Professionals: 85% of health care professionals
surveyed were either paramedics/EMTs or physicians, the remaining
15% identified as nurses, NPs, PAs or other. All respondents were
involved in direct patient care. 33% had seen a patient with a medical
alert tattoo and of those 39% reported that their treatment of a patient
had at some point been influenced by the information in the tattoo. All
of these instances were in emergent situations. 83% of those surveyed
would support a patient considering a medical alert tattoo and 89%
would consider providing recommendations based on health care
professional guidance to patients considering a medical alert tattoo.
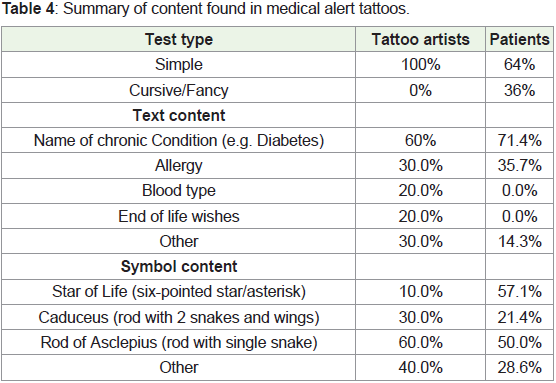
Content: Content of tattoos is summarized in Table 4. Text
content included in the “other” category generally referred to medical
history that did not fit into general chronic medical conditions
(for example, history of splenectomy, prior administration of
streptokinase). Symbols included in the “other” category ranged
widely and notably included blue circles and I>^v, (both of which
are representative of diabetes) as well as cartoon characters, 5 pointed
stars, syringes, skull and crossbones.
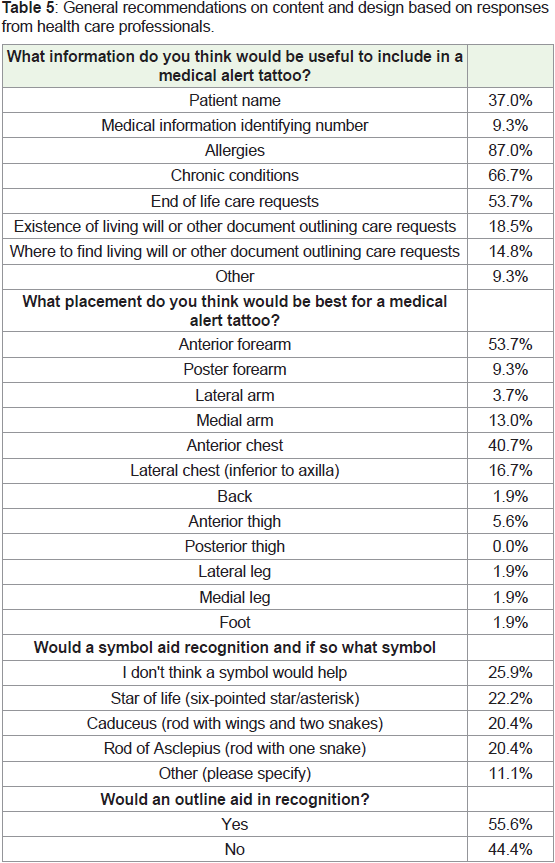
Recommendations: Health care providers were asked about their
recommendations for content and placement to make medical alert
tattoos more recognizable and useful to the patient. Responses are
summarized in Table 5.
Discussion
Incidence/Prevalence: The incidence and prevalence of medical
alert tattoos is very difficult to estimate. The usual creators of medical
alert tattoos, tattoo artists, are theoretically a good source of data
but this proved very difficult to obtain. Prevalence estimates are also
difficult as there is likely response bias, particularly with social media.
However, when searching popular media articles and image search
engines it is clear that tattoos are being used by many patients to
convey medical information. Given their widespread use by patients
it is important that health care professionals are aware of this practice
and be trained in their recognition and interpretation in situations
where a patient cannot communicate their medical information.
Content: In terms of tattoo subject matter, both tattoo artists and
patients reported chronic medical conditions as the most common
content. Allergy was the next most common, followed by other (which
included splenectomy and previous administration of streptokinase),
blood type, and end of life wishes. The information health care
professionals thought would be most useful to include were allergies
(87%) and chronic conditions (67%). Just over half (54%) thought end of life care requests would be useful. Surprisingly, a minority (37%)
thought a patient’s name would be helpful information and only 9%
felt a medical information identifying number would be helpful. In
the case of ID numbers, these apply only to the system in which they
are assigned and are not linked to the patient universally. Although
memberships to services like Medic Alert and various applications
connect an ID or a phone to a chart [20], going through the process to
access the information takes time. Clear, easily accessible information
can make medical alert tattoos valuable in emergent situations where
time constraints make it difficult to go searching for a patient’s
medical information.
Tattooing as a means of recording vaccination status was
proposed in 1959 but before recently was not popular [21], possibly
because of the high numbers of recommended vaccines in western
countries where tattoos are popular. Vaccination status was not seen
in medical alert tattoos in this survey; however, it closed before the
first COVID-19 vaccine became available. Currently internet searches
reveal that many people are getting virus and vaccine themed tattoos
both as a general topic and to indicate vaccination status. There
are examples of vaccination cards and even QR codes linked to the
European “Green Pass” which allows access to public sites/events if
the patient’s vaccination status is verified through this government
regulated system [22].
Text: All tattoo artists surveyed had only put simple text in
medical alert tattoos. However, 36% of patients reported using cursive
or fancy text in their tattoo. Using complex text can impair legibility,
particularly long term as ink bleeds within the skin and may blur
irregular edges of fancy text. Tattoo artists universally recommended
simple text to optimize long term legibility. Size is also a factor in long
term legibility. Artists were asked about the minimum size of text
they felt confident would be legible over a long period of time. Larger
was better with most people recommending approximately 1 inch
or 2.5cm, although several artists noted that this would depend on
technique. Namely, single needle technique (not used by all artists)
with careful ink deposition would allow smaller text to remain legible
for longer. So in addition to a clear font an experienced licensed tattoo
artist is important to guiding the minimum size of font to ensure long
term legibility if a small tattoo is desired.
Symbology: Symbols are widely used to quickly visually identify
information such as hazards, directions, and categories. 74% of
health care professionals surveyed felt that they would be more likely
to recognize a medical alert tattoo if a medical symbol was included.
Symbols can have varied meanings when used in tattoos [23].
Within the context of medical alert tattoos there is wide variation in
symbol use but the caduceus, rod of Asclepius, and star of life are
seen most frequently. These examples are associated with medicine
and para medicine. While these associations are an important aspect
of a symbol aiding in recognition, the symbol’s popularity is also
an important part of its usefulness in this context. One example of
the difference between accurate association and recognizability is
the blue circle. This symbol is accepted to be a symbol of diabetes
by many patients with diabetes as well as diabetes associations
[24], but is not widely recognized outside of these communities. Of
the health care professionals surveyed in this study, only 9% had
previously heard of a blue circle representing diabetes. Similarly
I>^v (‘I’m greater than my highs and lows’) is a popular symbol for
diabetes within these patient communities but would be unlikely to be recognized as medical information in an emergency. Symbols not
traditionally associated with medicine may be chosen by patients for
artistic or personal reasons, but may be less likely to be recognized
by emergency medical providers. Surveyed medical professionals
were split between which of three common medical symbols was
most recognizable. This may be influenced by type of medical care
practiced; pre hospital symbols tend to use the star of life, where the
caduceus and rod of Asclepius are seen more often in hospitals and
private clinics. Providers might more easily recognize the symbols
they see more often in their environment.
The interpretation of symbols alone can also be very problematic.
The medical symbols discussed can also be seen in tattoos on
people without intent of reference to their health. Caduceus, Rod of
Asclepius and Star of Life tattoos are commonly found on health care
professionals and even symbols specific for a particular condition can
be found on patients without the referenced condition. For example,
a parent may have a blue circle for a child with diabetes, or a person
may have a colored ribbon for a family member with cancer. One
case report above gives an example of a DNR tattoo containing only
a crossed out image of an old model of defibrillator pad, which may
not be recognizable as such to current providers [25]. While they can
aid in recognition, a symbol alone is not sufficient to reliably convey
medical information and assumptions should not be made about the
patient’s health status if they are found to have a symbol associated
with a medical condition.
Safety Issues: Tattoos and the process of tattooing are not
without risk. Transmission of viruses such as Hepatitis C and HIV by
tattooing is well established [23,26]. Although the risk of infectious
disease transmission is low with licensed professional tattoo shops,
particularly compared to those obtained in prison or by any nonprofessional
tattooists where needles may be shared [23], the risk of
any kind of infection is still an important factor to consider.
Under the US Food and Drug Administration tattoo inks fall
under the Federal Food, Drug, and Cosmetic Act [27]. The FDA has
never approved any ink for injection into the skin (although India
ink IS FDA approved for endoscopic submucosal injection) [28], and
many pigments used in tattoo inks are not even approved for external
skin contact [27]. While recommendations on sterility of tattoo inks
are provided by the Council of Europe [29], this regulatory body
does not have legal power to enforce these recommendations. One
study in Denmark found 10% of unopened stock bottles and 17% of
previously used stock bottles were contaminated with pathogenic and
non-pathogenic bacteria [30]. An FDA safety update in May 2019
also identified several available inks as contaminated with multiple
microorganisms [31].
Because of the artificial coloration in tattooing, benign or
malignant skin changes may be harder to identify [32], and the ink
itself may actually predispose to pathologic processes. Surveys of tattoo
ink contents have revealed Group 1 (carcinogenic to humans) and
Group 2B (possibly carcinogenic to humans) compounds which may
be present in the ink or produced with UV or laser exposure [29,33].
While multiple cases of skin cancers associated with tattoos have been
reported in the literature [33,34], a causative relationship is difficult
to establish and at this time occurrence of melanoma on tattoos is
considered coincidental [33]. However, inflammatory reactions have
been clearly linked to tattoo ink exposure and it is logical that cellular
changes associated with chemical exposure may directly or indirectly lead to malignant degeneration [35]. Additionally, tattoos may make
interpreting diagnostic studies for lymphatic spread of malignancy
more difficult; in some cases extra cutaneous pigment migration
may lead to false positive nodal spread of malignancy on PET [36] or
sentinel lymph node biopsies using dyes [37,38].
Exposure to tattoo ink can also trigger initial or recurrent
manifestations of underlying inflammatory conditions such as
sarcoidosis, various dermatosis, uveitis or severe allergic reactions that
may require surgical removal of the pigment [32,39-43]. While red
and black inks are most commonly associated with adverse reactions
it’s difficult to say whether the incidence is relatively higher than
other inks as relative frequency of use of different colors is unknown
but black and red appear most common anecdotally [41]. One of the
most common conditions depicted on medical alert tattoos, diabetes,
may lead to complications of healing a tattoo if blood glucose is not
well controlled [39].
Temporary medical alert tattoos are commercially available and
often targeted to children [44]. These commercial tattoos are usually
FDA approved with low incidence of adverse reactions, whereas
homemade temporary tattoos such as those made from henna may
be associated with severe allergic and other reactions [45]. Safety data
for use of tattoo ink in children is not available. Tattoos may become
distorted and illegible with growth, making them impractical for
children and adolescents. There are also legal age cutoffs for tattooing
in many countries and states [46], related both to lack of safety data
and the ethical issues with inflicting pain without clear benefit on
those under the age of consent.
Social Issues: Despite the increasing prevalence of tattoos in
western society, there is still a recognized stigma associated with them
in many groups. Historical and contemporary literature has frequently
shown a link between tattoos and antisocial behaviors [47-51].
While there does seem to be a link with early age body modification
and risk taking behavior, older adult studies may have significant
selection bias as they frequently draw their data from criminal or
mental health facilities [23,47,52]. In fact, a recent European survey
showed that people with body modifications including tattoos and
piercings reported higher self-esteem and fewer symptoms of social
impairment and sleep disorders than their non-modified control
group [53]. A study from the same year reported that 16% of tattooed
people surveyed regretted at least 1 tattoo, but the rates of regret were
significantly higher in those who were first tattooed before age 21 [54].
Another study from 2012 looked at motivations for wanting tattoos
removed and most common reasons were professional (for example
rules at work about visible tattoos or applying for a different type of
job) or personal (most commonly a change in relationship status with
a partner named or depicted in a tattoo) [55]. Regrets about tattoos
are very rare in military personnel [23]. In the case of a medical alert
tattoos, comments by our respondents did not express regret. In fact,
in both this study and a prior smaller study on diabetics with medical
alert tattoos patients felt encouraged or supported by family and or
medical providers with only one example of a negative experience in
the smaller study [56].
Motivations: A study by Kluger et al asked 5 diabetic patients
about their motivation for getting medical alert tattoos [56]. One
reported metal allergy and the rest inconvenience of jewelry. The
current study also found that inconvenience and cost of jewelry was
also a large contributor to the decision to get a medical alert tattoo, but also found that personal art and a feeling of mastery over the chronic
condition were important motivators for many people. Considering
that these non-medical reasons are sometimes motivators for getting
medical alert tattoos it is understandable why some patients may not
be receptive to recommendations from health care professionals on
their use. However, the majority of patients seem to be motivated
by practical reasons and based on this study would be receptive to
guidance.
Accuracy: In the case studies above there are several examples
of errors including simple and identifiable spelling errors as well as
inaccuracy of the content to the patients’ current clinical situation.
Arguably the biggest problem with the information contained in
medical alert tattoos is that it is self-reported. As any clinical provider
will attest, patient self-reports of their medical history are not
infallible. In one study 7% of service members self-reported incorrect
blood types or Rh factors on a screening form for a walking blood
bank [57]. In the blood type tattooing program during the cold war,
the incidence of incorrect tattoos was estimated to be as high as 10%
[18]. The consequences of transfusion with incorrectly cross-matched
blood may be fatal. The more recent issue of restrictions on people
refusing COVID-19 vaccination could conceivably serve as motivation
for incorrectly reporting vaccination status through a tattoo. In cases
where it is possible to confirm information in medical alert tattoos
this should be done, but when that is not possible weighing risks and
benefits of acting on this information can be helpful. For example,
acting on an incorrect DNR tattoo can have fatal consequences,
whereas acting on an allergy tattoo has minimal risk.
DNR tattoos: Under US federal law “an advance directive is
defined as: A written instruction such as a living will or durable power
of attorney for health care, recognized under state law […] relating
to the provision of health care when the individual is incapacitated.”
[58]. Depending on state regulations a tattoo may or may not qualify
under this definition. In the UK, the requirement for a valid advance
directive is that it is in writing, specifies the patients exact wishes and
is signed by the patient and a witness [59]. In Finland, according to
the National Authority for Medico legal Affairs, a tattooed consent is
not legally equivalent to a signed document [60].
A recent article in the Oregon Law Review examined this topic
in the context of US law [61]. Two states, Florida and Oregon,
require advance directive or Physician Orders for Life Sustaining
Treatment (POLST) documents to be printed on specific color paper
which more explicitly invalidates tattoos. Some states do recognize
advance directive proxies in the form of cards or jewelry, and the
author suggests that tattoos could theoretically be used as proxies
if approved by a given state. This would be particularly useful in
states like Oregon where copies of patients’ POLSTs are available
online and indication of their existence for a given identified patient
could be enough to quickly confirm the patients’ wishes and guide
management accordingly.
In the absence of clear and specific verbiage in many state laws
on this subject, interpretation can be aided by hospital specific ethics
consultation. To quote the committee in Holt et al’s case study [62],
“what might be seen as a caution could also be seen as standing on
ceremony, and […] the law is sometimes not nimble enough to
support patient-centered care and respect for patients’ best interests”.
To best interpret the information presented in DNR tattoos, providers
must be aware of their local laws and apply them to each individual clinical circumstance with the patients’ best interests at the core of
their intent.
Opinion articles have suggested that DNR tattoos should never
be considered equivalent of an advance directive [63]. This article also
brings up the same issue with an example of a piece of jewelry that
simply stated “DNR”. In this case the patient presented with need for
a laparotomy which was done, and when recovered the patient told
providers the DNR referred only to not wanting a prolonged ICU stay.
Of the case reports reviewed on DNR tattoos, only 3 of 5 represented
confirmed accurate information about the patient’s end of life wishes.
One did in fact inform provider decision making in the absence of
next of kin, and after the patient was made officially DNR but before
they expired their paper DNR document was found confirming the
information in the tattoo [62]. One of the two that did not represent
accurate information was in an elderly male who had previously been
DNR but whose health had improved and he changed his legal status
[64]. The argument was that tattoos can’t be valid because they are not
changeable, which is inaccurate; Tattoos can be changed in multiple
ways. Complete removal or elaborate cover up of a tattoo particularly
one in black ink is time consuming and expensive. However, adding
a line crossing words out can be done quickly and often without an
appointment. As such simple changes to a tattoo can in some cases be
easier than changing a legal document. In this case report it is unclear
if any guidance on changing the tattoo was given. In situations like
this it is valuable for providers to be aware of options for removing or
changing tattoos as patients’ medical information changes.
Another example of an inaccurate tattoo is a patient who had the
letters “DNR” tattooed on his chest because he lost a bet during a
poker game [65]. There are also a few other general media articles
on people who have DNR tattoos that are meant for style rather than
actually conveying medical information. This further supports that
providers need to be wary of the accuracy of these tattoos. In general
when people get these tattoos for reasons other than conveying end
of life wishes they tend to be relatively simple, small, and very rarely
say anything other than the letters DNR. However, there are examples
of small simple DNR tattoos being accurate expressions of patient
wishes and there are probably examples of complicated tattoos being
inaccurate. With any expression of patient wishes there is a duty to
confirm them if possible and if only limited information is available,
if a provider acts in good faith with the information available there
is ethical and legal precedent for taking DNR tattoos into account
which can be further guided by consultation with the hospital ethics
committee.
Validity can be considered similarly with any nonstandard
advance directives- a declaration of wishes is only useful when it
can be confidently applied to the clinical situation the patient is in.
Arguably one can compare the contents of tattoos to the patient in
a moment of lucidity saying exactly what is written in the tattoo.
For example, if a patient woke and said “DNR”, it would not be
appropriate to assume that means they want no interventions. The
UK Mental Capacity Act states that a provider should not incur
liability for providing treatment in the patient’s best interests if they
do not know or are not satisfied that a valid and applicable advance
decision exists [59]. One must be satisfied that the statement is
clear enough to be valid and applicable to the situation, which very
often requires further thoughtful investigation even in the case of
a patient presenting with an advance directive document. If able to effectively communicate, these patients will often agree to advanced
interventions if their counseled that their condition is likely reversible
and they have a reasonable chance of recovery. The non-standard
formats of living wills and other documents and the difficulties in
interpreting and applying what is written has contributed to moving
towards more standard advanced directives and proxies as discussed
above. Regardless of the format, communication of wishes is only
as useful as the content and the applicability of that content to the
clinical situation.
Similarly to standardizing paper and electronic advance
directives, standardizing medical alert tattoos may also be useful. This
could aid in recognition, improve clarity of messages conveyed and
as discussed above potentially allow for legal recognition as a proxy
to a full advance directive [61]. One article suggested creating flash
that can be copyrighted by the American Academy of Hospice and
palliative medicine reading as follows: “Consider do not resuscitate:
I concur to the guided and educated decision of my medical team for
medical futility in my present clinical scenario.” [66]. While it seems
this did not come to fruition, the idea of providers partnering with
national associations with the guidance of ethical and legal teams is a
useful one. Further collaboration on this issue is needed.
Limitations of this study
The population of patients with medical alert tattoos is a difficult
one to study. Determining prevalence is difficult as these tattoos are
usually done without involvement of the medical system. Incidence
is even more difficult to determine as the population controlling the
incidence (tattoo artists) exist outside the culture of medical research.
Outreach through social media as done in this study and prior
smaller studies is problematic in that there is notable response bias
[56]; patients with medical alert tattoos likely have more interest in
completing a survey on something that relates directly to them, and patients with chronic medical conditions without medical alert tattoos
may be more likely to respond if they are already considering getting
one. The technology of tattooing itself is also quite old. While it’s still
being done many questions were encountered in the process of this
study about newer technologies to store medical information such as
microchips. However, similar problems come up where information
may be out of date, inaccurate, not recognized or not compatible
with locally available technology. Most importantly, the data on this
subject overall is not strong enough to definitively say medical alert
tattoos can improve outcomes for patients with chronic medical
conditions. That kind of certainty with all the possible confounders
would likely require a randomized control trial which is not a
practical option. We have tried to collect data from patients, artists
and medical professionals to guide recommendations. Although we
were not able to obtain large sample sizes, to the author’s knowledge
this remains the largest study on this topic to date.
Conclusions and Recommendations
The results of our survey support that many medical professionals
believe that medical alert tattoos can be an appropriate media for
conveying medical information. It is important to note that the
appropriateness varies on a case-by-case basis driven by the patient’s
medical history and motivations as well as the clinical setting. Based
on the current lack of structured guidance on this subject coupled
with the already wide use of medical alert tattoos, whether or not
medical alert tattoos are a good idea or not is somewhat of a moot
point as it is clear patients are going to get them regardless of the
presence or absence of guidance. However, as most patients report
that they would be receptive and that there seems to be room for
optimizing their usefulness, formal recommendations are warranted.
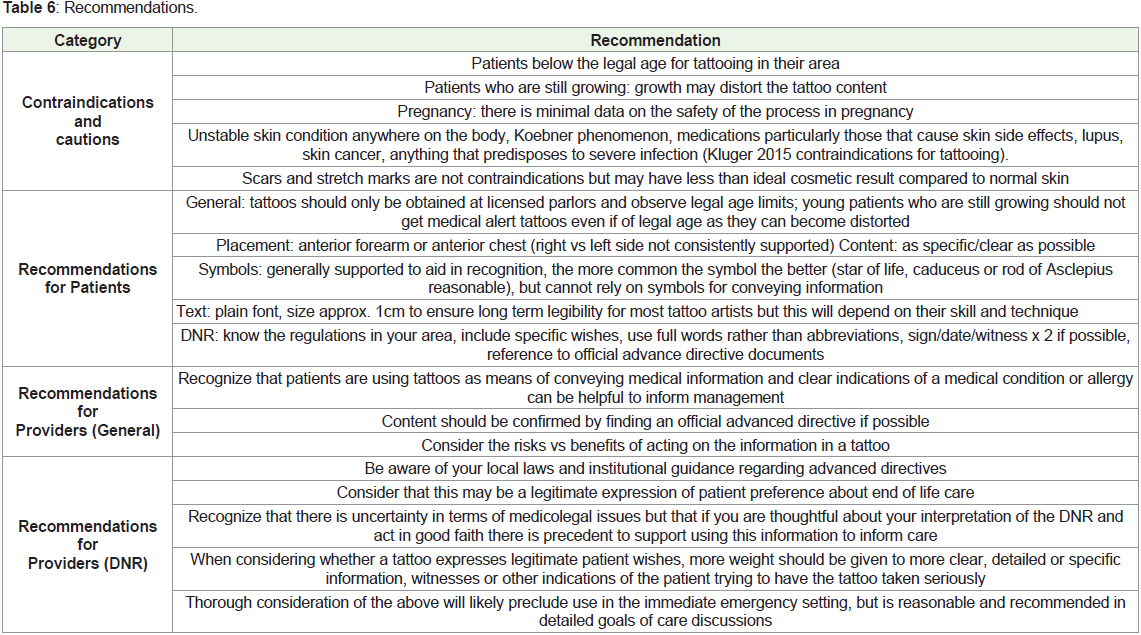
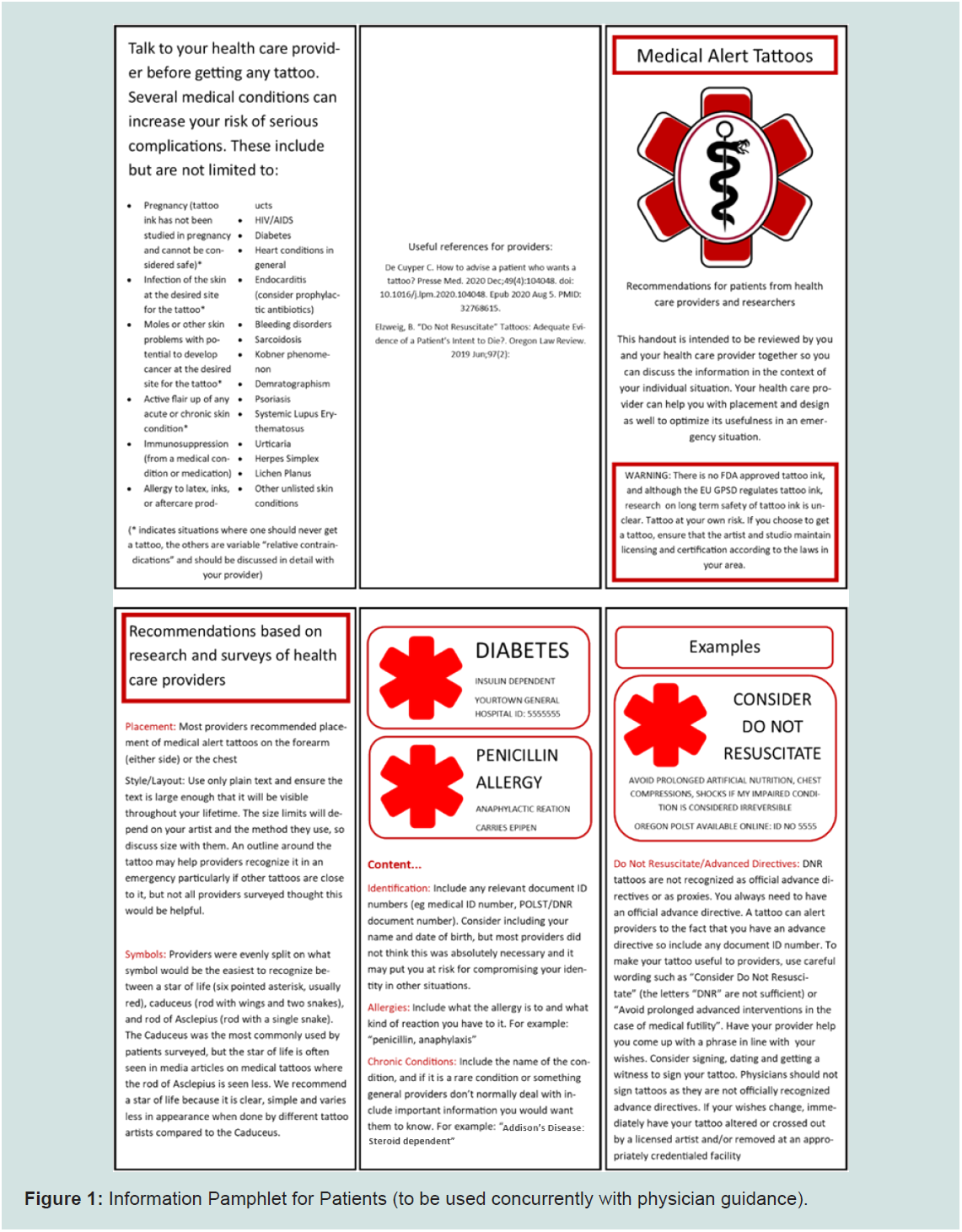
As such the following recommendations are proposed for patients
and health care providers (Table 6 and Figure 1).
Acknowledgements
The author would like to thank Dr Gemma Kelleher for her
support of this project through the design and ethical approval
process, and Dr Laszlo Kiraly during the editing and submission
process.