Journal of Emergency Medicine & Critical Care
Download PDF
Review Article
Characteristics of the Contemporary Intensivist: A Qualitative Study
Dennis D1*, Knott C2, Khanna R3 and van Heerden PV4
1Department of Intensive Care and Physiotherapy Department, Sir Charles
Gairdner Hospital, Perth, Western Australia; Curtin University, Faculty
of Health Sciences, Perth, Western Australia
2Department of Intensive Care, Bendigo Health, Bendigo, Victoria, Australia;
Monash Rural Health Bendigo, Monash University, Victoria, Australia; Rural
Clinical School, University of Melbourne, Victoria, Australia; Department of
Intensive Care, Austin Health, Heidelberg, Victoria, Australia
3Phoenix Australia, Department of Psychiatry, University of Melbourne,
Melbourne, Victoria, Australia; Division of
Mental Health, Austin Health, Heidelberg, Victoria, Australia
4Department of Anesthesiology, Critical Care and Pain Medicine, Hadassah
Medical Center and Faculty of Medicine, Hebrew University of Jerusalem,
Israel
*Address for Correspondence:
Dennis D, Intensive Care Unit, Sir Charles Gairdner Hospital, Perth,
Australia; Senior Lecturer, Curtin University, Perth, Australia; E-mail:
Diane.Dennis@health.wa.gov.au
Submission: 10 June 2022
Accepted: 16 July 2022
Published: 23 July 2022
Copyright: © 2022 Dennis D, et al. This is an open access article
distributed under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
Abstract
Background: Intensive care professionals work together within a
high-acuity high-stress environment and develop unique clinical and
human skill sets within the specialty. The manner in which medical
leadership acts, responds, and is understood by those around them
is an important component of optimising healthcare. The aim of this
study was to explore, qualify and define the self-perceived attributes
of senior doctors working in intensive care (Intensivists), and construct
‘Intensivist personas’ that might provide useful insight for the entire
healthcare team.
Methods: Using a prospective qualitative design, this study
involved face-to-face interviews with 19 Intensivists who each had
more than four year’s clinical experience. Participants were asked
their perceptions of the typical personality traits of a ‘flourishing’
Intensivist; and how they felt they were viewed by others outside their
specialty. Interviews were audio recorded, transcribed and attributes
were coded using a thematic framework analysis of each transcript
using NVivo software. Personas that might represent the contemporary
Intensivist were then constructed based on the themes that emerged.
Results: More than 700 pages of coded data were extracted from
the transcripts. Six personas were built according to how Intensivists
saw themselves: the Fixer; the Retriever; the Diplomat; the Negotiator;
the Pragmatist; and the Duck. An additional three personas were
created relating to how they perceived they were viewed by others’:
the Superhero; the Naysayer; and the Dictator.
Conclusion: This study describes the self-perceived personality
traits of modern-day Intensivists and in doing so, adds to the scarce
qualitative literature available. Understanding these attributes is
important for all who work in intensive care, including nurses who are
an integral part of healthcare service delivery.
Keywords
Intensive care medicine; Doctors; Thematic framework
analysis; Personality traits; Interview
Background
The practice of medicine goes back to ancient times and was
historically a broad-based science. In modern medicine, there is
increasing specialisation of practice in line with the massive expansion
of knowledge, and the advanced skill set required to deal with new
technology. As a result, our human understanding of ‘what it is to
be a doctor in the 21st Century (Common Era) is rapidly evolving,
with over 1.5 million new medical-related studies indexed annually
on search engines such as Pubmed [1].
Intensive care is a field of medicine devoted to managing complex
life-threatening illness. It has its origins in the mid-nineteenth century
Crimean War, when Florence Nightingale tended to those soldiers
worst injured in an area geographically closest to her nursing station.
These patients were closely monitored and attended to quickly in the
event of clinical deterioration [2]. This ‘collective’ model of acute
care (cohorting the sickest patients to where most of the resources
are) was further established in the 1950s in response to the global
poliomyelitis epidemic. Medical centres throughout the world
established respiratory ‘intensive care units’ (ICUs) to monitor and manage patients requiring positive and negative pressure ventilation.
Anaesthetists were frequently involved in the development of these
services as they were seen to be the experts in airway intubation
[2], ventilation and resuscitation. In the years that followed, these
respiratory or ‘general’ ICUs devolved into the distinct sub-specialties
seen today in some countries, based on the nature and case-mix of
the hospital. For example, separate ICUs for surgical, burns, cardiac,
paediatric and neonatal patients.
As the discipline of Intensive Care matured, specialist doctors from
other, often diverse, backgrounds also sub-specialised in intensive
care medicine. Part of this involved the establishment, development
and maturation of professional societies which defined the role of the
‘Intensivist’, including the core competencies and training required.
In Australia and Aotearoa New Zealand, the ‘newness’ of intensive
care medicine as a speciality is reflected by the fact that the Australian
and New Zealand Intensive Care Society (ANZICS) first met in 1975
[3], formalising training of Intensivists in 1976 with a specialist
College becoming operational in December 2010 [4,5].
The key service elements of a modern general ICU are centred on
the delivery of a number of highly invasive supportive therapies such
as mechanical ventilation; renal replacement therapy; extracorporeal
membrane oxygenation and monitoring [6], which are implemented
through the coordination of a broad interprofessional team of
doctors, nurses, allied health professionals and others. Modern-day
Intensivists are correspondingly directly responsible for patients
under their care in a relatively closed clinical system, with input
from other specialties as required [4], the so-called “closed” model
of intensive care.
Although present-day doctors represent a similar cohort in
terms of the entrance criteria for medical school, and receive broadly similar pre-licensure training, there is an abundance of literature
dating back to the 1960s suggesting that personality stereotypes
exist for some medical specialties [7,8]. Anaesthesia, for example,
has been reported to attract people who are more self-sufficient and
extroverted compared to doctors in general practice [9]; Psychiatrists
have been characterised as possessing greater frustration tolerance,
emotional maturity and stability than seen in other fields [10];
Surgeons have been found to be more tough-minded, resolute and
unempathic compared to both anaesthetists and doctors in general
practice [11]. These data are important, as the synergy of personality
type with working environments has been shown to be significantly
related to workplace resilience [12].
A persona describes a particular type of character that a person
seems to have, often different from the real or private character that
person has [13]. It is a fictional individual whose characteristics
may be derived as a composite of a number of different real people
[14]. As the field of intensive care medicine is relatively new, there
is little published data related to the self-perceived personality traits
of doctors working in the domain. Creating a shared understanding
of these frames would be useful to all who work within the intensive
care healthcare service delivery. Based on the personal reflections of
a sample of Intensivists, the aim of this study was to explore, qualify
and define the attributes of doctors working in intensive care in order
to construct the persona or personas of the contemporary Intensivist.
Methods
Research design and setting:
This study used a prospective qualitative design to explore the
research question of what characteristics define the attributes of
doctors working in intensive care. To answer this, the primary
objectives were to1. Interview a group of experienced Intensivists
2. Analyse their responses and construct a persona or
personas of the ‘typical’ Intensivist.
A once-off face-to-face interview was conducted on-site at each
participant’s respective hospital during non-clinical time in a quiet
location adjacent to the ICU. Ethical approval was granted by Sir
Charles Gairdner Hospital HREC (Lead site: RGS0794); the Austin
Hospital/HREC/18/OTHER/14); Hadassah University Hospital
(0313-18HMO). All participants provided informed written consent
prior to participating in the study.
An example of the specific interview questions relating to
Intensivists’ perception of the characteristics of the modern-day
Intensivist was:
“Can you describe what you think are the attributes and typical
personality traits of a ‘flourishing’ Intensivist?”
and “How do you think those professionals outside of intensive
care view the stereotype of the contemporary Intensivist?”
Participants:
Intensivists from two countries (Australia and Israel) who had
worked in the ICU specialty for more than four years were considered
for inclusion in the study cohort. They were approached in-person by the site investigator and provided informed written consent prior to
participating.Data collection:
Data collection was undertaken by three researchers (Intensivists
[CK and PVvH], and non-Intensivist [DD]) who all had experience
in qualitative research methods. Interview data was audio-recorded
and transcribed. Transcripts were edited by participants for accuracy,
and then returned to one investigator (DD) who entered them into
the dataset as de-identifiable data. Data saturation was reached
after approximately 60% of the population of Intensivists had been
interviewed at the first site (in Israel), suggesting that approximately
15-18 participants would provide thematic sufficiency.Data analysis:
NVivo software (Version 12, 2018 software; QRS Pty Ltd.,
Victoria, Australia) was used to undertake a thematic framework
analysis. Codes were initially generated by two investigators (DD and
RK) who reviewed two random transcripts independently. One of
these researchers (RK) had not undertaken any interviews and was
not an Intensivist, which ensured the reflexivity of the analysis. The
final code-book was built with the consensus of all investigators who
subsequently coded all manuscripts. Personas were created from the
themes and subthemes that emerged from coding; literal quotations
were selected to support these constructs.Results
During 2018, 19 hour-long interviews were carried out at an
Israeli institution (n=6) and two Australian institutions (n= 6 and 7
respectively), with one Australian Intensivist declining to participate.
Six personas were constructed around the self-perceived attributes
that defined the Intensivist.
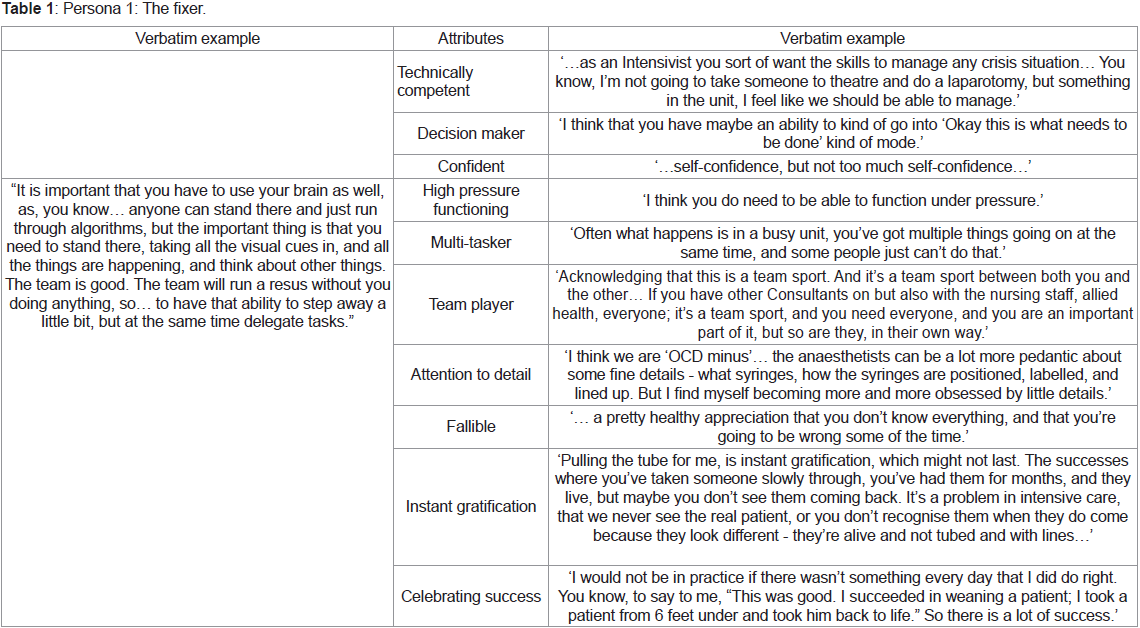
The Fixer (Table 1): Described as one who applied technical competence
to make patients better; someone confident who worked well
under pressure.
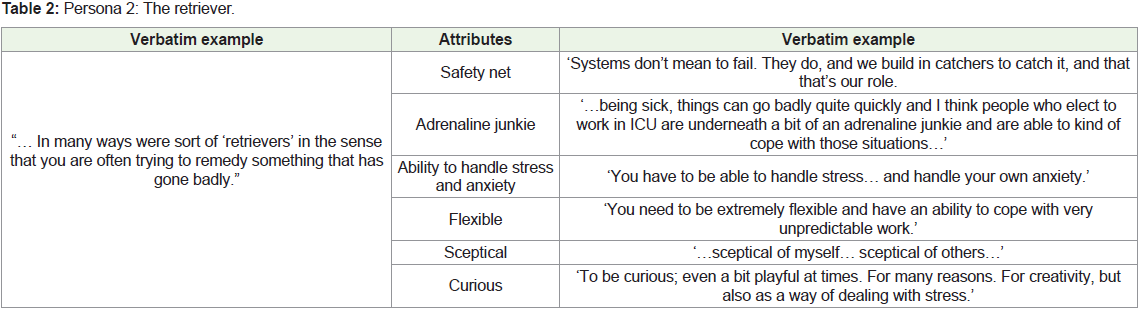
The Retriever (Table 2) : Described as one who was able to take
the sickest of patients and restore them to better health.
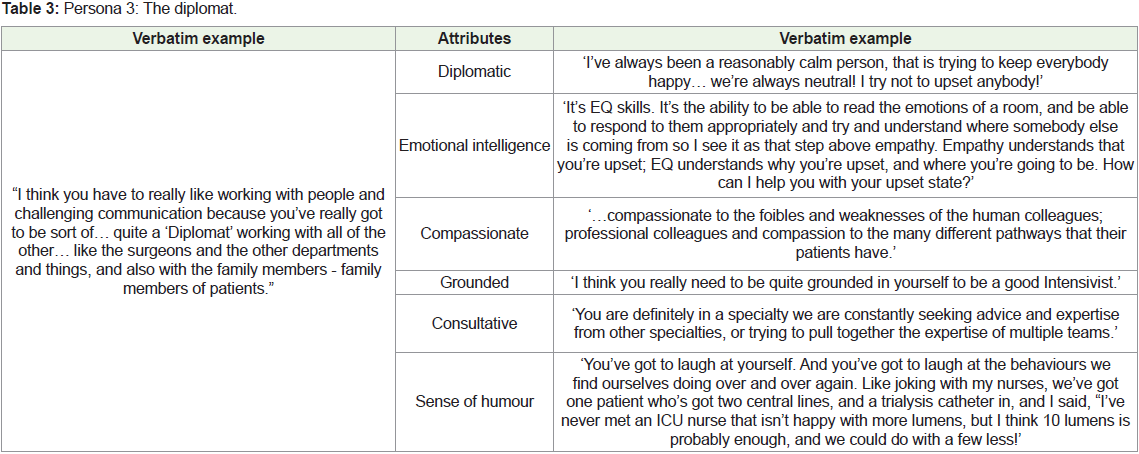
The Diplomat (Table 3): Described as one who was able to navigate
interpersonal relationships successfully in order to facilitate best
patient care.
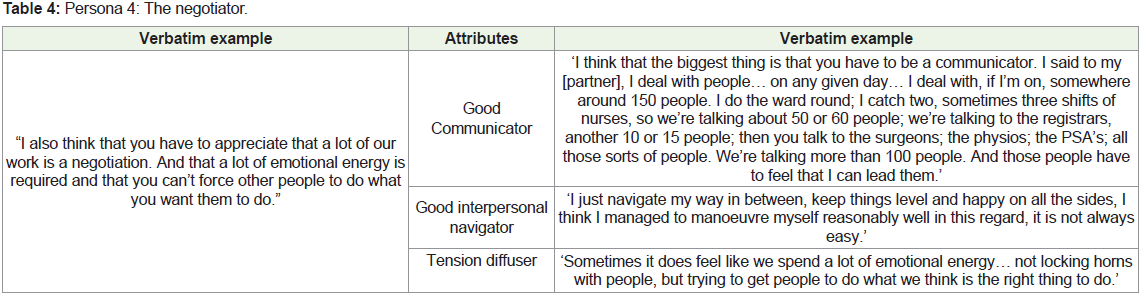
The Negotiator (Table 4): Described as one who was a steadfast
patient advocate in order to facilitate best patient care.
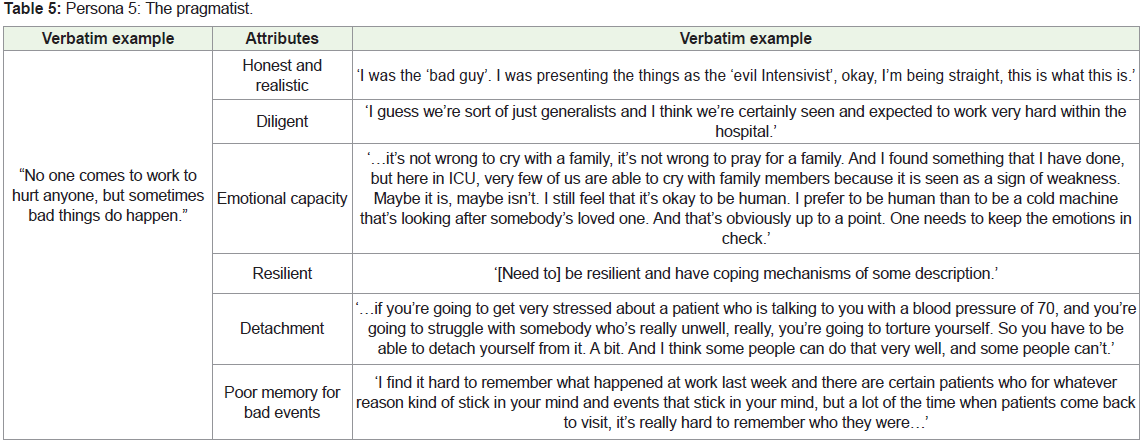
The Pragmatist (Table 5): Described as one who was realistic and
practical in the face of difficult conversations and uncertainty.
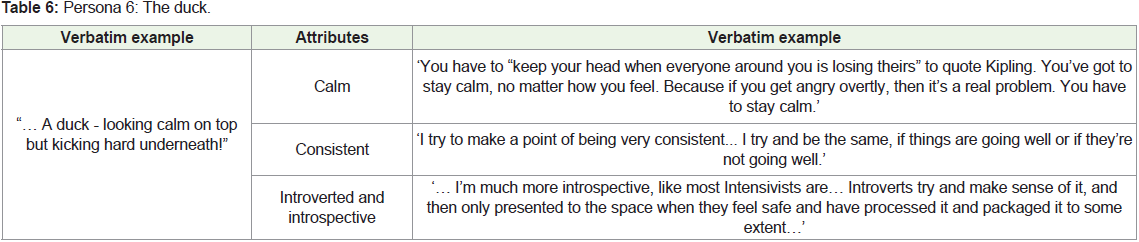
The Duck (Table 6): Described as one who appeared consistently
calm in a crisis whilst perhaps figuratively paddling furiously beneath
the water to achieve a good outcome.
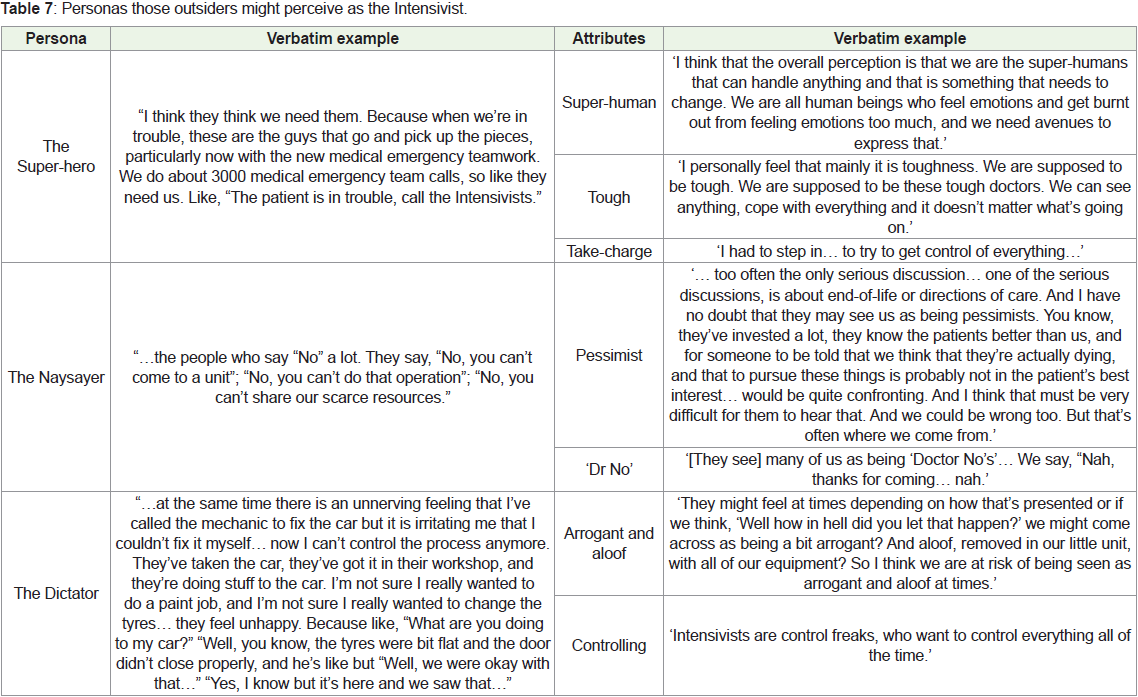
A further 3 personas were constructed around reported attributes
which the Intensivists considered were the external perception
of that outside of the Intensive Care Medicine specialty (Table 7). These were the Super-hero; the Naysayer; and the Dictator.
Discussion
Perceptions of self (Tables 1-6):
When asked to describe the attributes and typical personality
traits of a ‘flourishing’ Intensivist, one respondent began by saying,
“I think it takes all sorts” and this statement summarises the data
that emerged. We built nine personas from the attributes that
Intensivists’ identified, either within themselves or in their intensive
care colleagues. Six of these were constructed according to how
they viewed themselves; three were assembled in line with how they
imagined their specialty projected themselves outside of intensive
care.Intensive care doctors deal in high levels of patient illness acuity,
and each persona perhaps reflects a unique facet of their daily life,
including the responsibility of directing the provision of care. Intensivists are often leading a team as the last in a long line of defence
trying to enhance survival and recovery for a patient. Working with
their team, they may bring people back from the certainty of death
to the possibility of survival (the Retriever persona). We can conjure
up visions of care and consultation outside of the ICU, such as their
attendance at Medical Emergency Team calls, their involvement
in the triage of patients’ enroute from places external to hospital
emergency departments; or from within the hospital, like operating
theatres. Being both curious and sceptical of other’s decision making
fits the uncertainty of being faced with an unknown patient in an
unfamiliar non-ICU environment. It also allows for the avoidance of
cognitive biases in one’s own decision-making which is needed in
order to function as this last line of defence [15]. Being adaptable and
flexible in response to unexpected circumstances, in fact thriving in
that atmosphere, like an ‘adrenaline junkie’, were key components of
this persona.
Perhaps more optimistically, Intensivists also possess the
expertise and technological arsenal to lead new solutions in the high
acuity environment (the Fixer persona) to enhance patient survival
or improve prognosis. This persona comprised sound clinical
competence, strong technical skills with confidence and ability to
undertake multiple tasks and make quick decisions under high levels
of pressure.
Acknowledgment that the Intensivist does not function in
isolation was a key attribute of the Fixer, whereby teamwork, and the
ability to share in the celebration of success, were qualities identified.
The Intensivists recognized that they bring others along with
them on the patient’s journey, sometimes willingly (the Diplomat
persona) and sometimes under duress (the Negotiator persona).
The features of the Diplomat included an ability to ‘read the room’
in difficult circumstances and remain grounded and compassionate.
The Diplomat is happy to seek the advice of others, and able to
laugh at their own idiosyncrasies. The most distinctive attribute
of the Negotiator is the skill of communicating, and the ability to
navigate and overcome interpersonal conflict and diffuse tension.
This extended from interactions with co-workers in the ICU to
interactions with patients, and family, and the other specialties with
whom they worked.
Respondents commonly acknowledged that no matter how much
quality care they provide, patients can still unpredictably live or die
without rationalisation. The Pragmatist persona comprised those
attributes of honesty, diligence and realism, which aligned with an
ability to have a degree of detachment from emotional involvement
and a poor memory for bad events.
Finally, at their best, Intensivists bestow both their care and
training of others in a calm and consistent manner (the Duck). This
persona represented more the manner in which they approached
their craft rather than the craft itself. The analogy was that during
crises, the Intensivist delivered coordinated care effortlessly as they
glided across the water, and yet beneath the water, they were actually
furiously paddling away. There is perhaps a piece of the Duck persona
in each of the other personas.
Projected perceptions of others (Table 7):
At face value, the projected perceptions of others looking in at
the specialty were somewhat at odds to the perceptions Intensivists
had of themselves. On closer examination however, each of the three
external personas could be seen as being equal and opposite to the
other six self-perceived constructs, albeit viewed in somewhat of
a negative light. For example, the ‘Super-hero’ Intensivist is seen
to swoop in when a patient or colleague is in peril to save the day
with super-human knowledge, calmness and strength of character
that belies authority. These features might be equally represented as
positive attributes in the characterisations of the Retriever and the
Duck - although the weight of responsibility that the Super-hero
persona conjures up perhaps matches the burden of the unreasonable
expectations placed upon them by others.Likewise, characteristics of the Pragmatist in taking a realistic
negative appraisal of the long-term outlook of patient care, and
relaying these views honestly with a level of personal detachment and
resilience, might be interpreted as reflecting a Naysayer persona - the
interpretation of what is pessimistic versus what is realistic defining the difference between the perspectives. The wide-angle lens of the Fixer
affords a longitudinal view and broad oversight and understanding
that might be viewed as arrogance in the ‘Dictator’ persona. Likewise,
the emotional intelligence and skill in communicating, seen in the
Diplomat and Negotiator respectively, might be represented in the
Dictator with negative connotation as being aloof and controlling.
It remains unclear as to whether these described perceptions
were derived from the responses Intensivists encountered in their
present-day practice, or whether they were anecdotally derived from
their years-in-training. No data was collected from people outside of
the specialty to support or refute the perceptions held, including the
nurses they worked with, as this was beyond the scope of the study.
With emerging literature related to the high rate of burnout
within the intensive care domain [16-18], our findings have
important implications in terms of the selection of, and entry into,
the specialty by medical trainees. Before choosing the intensive care
pathway, junior doctors should reflect deeply around their personal
attributes as to whether they fit some of the personae described.
Equally as important, during the selection of their trainees, training
programmes should screen applicants for attributes accordingly. It
should be acknowledged that some of these attributes, though not
directly teachable, can nonetheless be deliberately cultivated so may
have relevance even for current trainees/Intensivists. By having
awareness of the cultural traits in senior Intensivists, it may also be
desirable to select trainees differently for the creation of different or
diverse future personae for Intensivists who continue to adapt to the
ever-evolving sociotechnical field of intensive care medicine.
A strength of this study was that it sampled doctors from 3 sites
in 2 countries who had been working in the field of Intensive care
for a substantial length of time. Although some of those interviewed
serviced rural areas as ‘retrievalists’, a limitation was that the study
cohort was predominantly from urban adult intensive care centres
within well-developed healthcare service delivery teams. We
acknowledge that other personas and attributes may have surfaced
from a sample that included both rural and paediatric Intensivists.
There were also no interviews of people external to the specialty to
substantiate the perceptions had by those outside the discipline as to
the personas of the Intensivists, and this is both a limitation and a
path for further study.
Conclusion
This study adds to the relatively scarce qualitative literature on
the personality traits of doctors in modern-day medicine, providing
specific self-reported insight into the intensive care specialty. Nine
personas were constructed, and no one of these stood alone as
the ultimate definitive identity; neither was one specific persona necessarily mutually exclusive of another. The contemporary view of
the Intensivist is perhaps better represented as a combination of all
of the nine described. The perception of others working in the field
related to these personas is a future direction of this work.
References
3. Australian and New Zealand Intensive Care Society (ANZICS) (2021) Our History Camberwell, Victoria.