Journal of Emergency Medicine & Critical Care
Download PDF
Review Article
Hemodynamic Monitoring with the Clinic: Back to Basics
Pérez Nieto OR1, Guerrero Gutiérrez MA2*, MorgadoVillaseñor LA3, Fermín JL4, Zamarrón López EI5, Soriano Orozco R6, Sánchez Díaz JS7, Uribe Moya SE8, Diaz Martínez MA9, Deloya Tomas E10 and Escarraman Martinez D11
1Specialist in medical emergencies and critical care, General Hospital San Juan
del Rio, Mexico
2Resident of first year in critical care medicine, National Institute of Cancer,
Mexico
3Specialist in medical emergencies and critical care, IMSS Torreón Hospital,
Mexico
4Emergency Department, Adolfo Ruíz Cortines” IMSS Veracruz, Mexico
5Specialist in medical emergencies and critical care, Hospital Cemain Tampico,
Mexico
6Specialist in medical emergencies and critical care, IMSS UMAE T1, Mexico
7Veracruz. Specialist in medical emergencies and critical care, Mexico
8Department Emergency, Ángeles Lindavista Hospital, Mexico
9Department of Anesthesiology, General Hospital of Atizapan, Mexico
10General Hospital of San Juan del Río, Qro. Specialist in medical emergencies
and critical care, Mexico
11Department of Anesthesia. IMSS “La Raza”. Mexico City
*Address for Correspondence: Guerrero Gutiérrez MA, National Institute of Cancer, Resident of 1st year
in Critical care. Mexico City, E-mail: manuelguerreromd@gmail.com
Submission: 11 December 2019;
Accepted: 27 January 2020;
Published: 07 February 2020
Copyright: © 2020 Guerrero Gutiérrez MA. This is an open access article
distributed under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
Abstract
The state of shock is a frequent diagnosis in the critical areas,
prehospital, emergency, operating room and intensive care unit,
clinical hemodynamic monitoring is essential to make the diagnosis of
tissue hypoperfusion and its causes, in addition to guiding therapeutics,
the challenge It consists of performing adequate monitoring with the
tools available in our service, recent studies show that the data found
with the clinic have good reliability when compared to other types of
monitoring such as invasive and semi-invasive.
Keywords
Shock; Critical care; Hemodynamic monitoring; Clinical
Introduction
In any clinical scenario that involves facing a patient in a state
of shock, and regardless of the area in which they are (emergencies,
hospitalization, operating room or intensive care unit), early
recognition of an inadequate perfusion state will always be necessary
to start immediate treatment and achieve a reduction in morbidity
and mortality [1]. The objective will be to achieve adequate decisionmaking
as soon as possible and establish a therapeutic intervention
in order to restore normal hemodynamics and correct the cause that
led to the demand or significant loss of global perfusion, as this can
beneficially modify the course, prognosis and convalescence of the
disease.
Due to excessive abuse of invasive monitoring and abandonment
of the clinic, the aim of this article it’s to emphasize that the clinical
monitoring will always be within our reach, that is why in this review
we will observe that the clinical monitoring to the patient bedside.
Clinical evaluation and physical examination are the first steps
to individualize patients at risk of shock and timely detection of
manifestations of inadequate tissue perfusion, the clinical evolution of
the disease behaves in a multimodal manner and the sequential order
is not same in all patients, but in most cases, scientific knowledge
and experience return to the health personnel expert in identifying,
warning signs that may be useful clinical tools to demonstrate a state
of shock [2].
Hypotension is the sign attributed to the greatest importance in
most cases and is considered one of the main causes or manifestations
of shock, however, this can be found late in some circumstances and
the degree of hypotension does not necessarily correlate with the
degree of global perfusion of the patient [3].
Many common clinical alterations have been described as
indicators of inadequate global tissue perfusion, and some of them
reflect organic dysfunction, while others are related to the body’s
response to the significant stress to which it is subjected. As examples
to consider with sustainable evidence we have mottled and tortuous
skin, altered mental state (confusion, disorientation, seizures or
coma), and oliguria (urine production <20 ml/h or <400 to 600 ml/
day), data Named as clinical perfusion windows in shock, there are
also other signs that accompany inadequate tissue perfusion states,
these pillars not being in the strategy of identifying shock states, but rather related to the consequent or compensatory response of the
organism given the condition, such as tachycardia, dyspnea, increased
respiratory rate, jugular vein distension, and even peripheral edema
[4].
The so-called hemodynamic coherence refers to the balance
between the macrocirculatory and microcirculatory status, taking as
an initial pillar the resuscitation interventions aimed at correcting
the variables of the altered systemic hemodynamics, so that the
therapeutic used is effective in the correction of regional perfusion
and of the microcirculation ensuring the delivery of oxygen to the cells
of the vital organs so that they are able to maintain their functional
activities in what is reestablished from the cause of the shock [5].
Four mechanisms of loss of hemodynamic coherence have been
proposed, which, mostly described in patients with septic shock in
whom a failure in microcirculatory recruitment is observed despite
macrocirculatory resuscitation [5].
1) Heterogeneity: It is presented as a heterogeneous perfusion of
the microcirculation with clogged capillaries together with perfused
capillaries resulting in a heterogeneous oxygenation of the tissue cells.
2) Hemodilution: Dilution of blood in the circulation due to
aggressive resuscitation with liquids results in an increase in the
distance between erythrocytes and tissues
3) Vasoconstriction/tamponade: It is the stasis of the
microcirculatory flow of erythrocytes induced by circulatory failure
4) Tissue edema: Aggressive water resuscitation has the
consequences of reducing the diffusion of oxygen between the
transport cell (erythrocyte) and the receptor cell of the oxygen
molecule.
Macrocirculation is formed by the large, medium and small
caliber distribution vessels (arteries and veins) that carry blood from
the heart to the periphery and back to the pulmonary circulation,
and microcirculation refers to the microscopic vessels that carry the
oxygen and nutrients to the tissues and eliminate cellular debris.
The normalization of systemic hemodynamic variables in late
stages or in an inconsistent manner with the hemodynamic alteration
of the patient does not lead to improved perfusion of microcirculation
or oxygenation and instead can hinder it (eg excessive administration
of volume to a septic shock due to vasodilation), excessive
administration of vasopressor in systolic cardiac dysfunction).
The concept of a loss of hemodynamic coherence probably
explains the negative results in the 1990s, in which several
studies were conducted that aimed at normalization, or even
supranormalization of all the variables that influence oxygen delivery
systemic (cardiac output and arterial oxygen concentration) to coin
the term hemodynamic stability, or even take as a parameter of a good
resuscitation, without demonstrating significant benefit in morbidity
and mortality, therefore the importance of implementing a holistic
approach taking into account the clinical indices as a marker of global
tissue perfusion.
The future of hemodynamic monitoring aims to be continuous,
reliable, easy to interpret and that correlates adequately with the
physiological parameters, in addition to being complemented with
the metabolic results that together represent the real state of the
patient in a unit of time with the least possible injury and invasion
for the patient.
In the last decade, multiple systematized models have been
proposed as a guide in early recognition of a patient in the context
of inadequate tissue perfusion, as an example of a state of distributive
shock such as sepsis for which the SOFA score has been proposed
(qSOFA ) to identify those patients who are probably septic [] and at
risk of shock mainly outside the ICU, include systolic blood pressure
below 100 mmHg, respiratory rate above 22/min and altered mental
status, if two of Every three of these signs are present, sepsis should
be suspected. The qSOFA is a clear example of the simplification of
diagnostic criteria with emphasis on the clinic [6].
Blood pressure measurement monitoring (non-invasive):
Shock is defined as a state of effective tissue hypoperfusion,
not necessarily with arterial hypotension, commonly diagnosed
alternately by presenting lactate above normal values (> 2 to 4
mmol/L) [7].The pragmatic definition always included a Systolic Blood Pressure
(SBP) below 90 mmHg and a Diastolic Blood Pressure (DBP) below
40 mmHg, however, hypotension can be mostly evident only during
the most severe phases, since the mechanisms Homeostatic will try
to keep the average blood pressure at a normal level by increasing Systemic Vascular Resistance (SVR), this mechanism can be lost in
states of vasodilatation induced by sedatives or vasodilators, as well
as in vasoplegy, in this situation, the increase in SVR is useful to
maintain a minimum level of cardiac and cerebral perfusion, but it
can be detrimental to the perfusion of other organs, decreasing blood
flow and increasing oxygen debt [8].
Many patients with acute heart failure may develop signs of
peripheral disease and anaerobic metabolism without hypotension
[8]. On the contrary, the high Mean Blood Pressure (MAP) at the
expense of increased SVR can be detrimental, affecting systolic
ejection, worsening oxygen delivery, in the same way, patients
with acute bleeding will try to keep TAM within the normal value
by increasing the adrenergic tone that will recruit the unstressed
volume of the venous reservoir and increased arterial tone, however,
if the bleeding is not immediately controlled, this compensatory
mechanism becomes harmful and will lead to multiple organ failure
and death.
The state of shock should be suspected in the context of a known
patient with hypertension when there is a decrease in AST greater
than 20% to the figures of BP that the patient is accustomed, this
criterion comes from the assumption that under a certain MAP, the
Organ blood flow depends on pressure, while above that point blood
flow can be considered constant [9].
Hypotension is frequently associated with shock conditions, but
in many cases, shock can begin without a decrease in blood pressure,
and it can be a very late sign of shock. Therefore, hypotension may be
evident in the previous context or if blood loss is more than half of the
circulating volume [10].
MAP is considered the necessary pressure for perfusion of vital
organs, when MAP falls below the lower limit of self-regulation,
regional blood flow becomes linearly dependent on MAP. In some
pathological environments, and in specific vascular areas, MAP
underestimates the true perfusion pressure, due to marked increases
in venous pressure or extravascular pressure at the level of outflow.
There is no universal way or threshold of MAP to ensure that
blood flow is independent of blood pressure in vital organs. In fact,
the critical level of MAP probably differs between the organs and
depends on numerous factors, including age, history of hypertension,
neurovegetative state, so it should be emphasized in independent
organic perfusion pressures [11].
From the mere figure of blood pressure, hemodynamic condition
data can be obtained, systolic blood pressure is the one recorded when
the volume of ejection of the heart collides with the arterial walls,
therefore, a decrease in BP with a predominance of SBP will be mostly
caused by a decrease in systolic volume, (hypovolemic, cardiogenic
or obstructive shock), at least temporarily, the pulse pressure, which
is the difference between the SBP and the PAD, decreases in these
situations, also, the PAD represents mostly the vascular tone of the
arteries, therefore, a decrease in BP mostly dependent on ADT should
make us suspect a state of vasodilation (eg septic shock, anaphylactic,
neurogenic), so that in these circumstances a patient may have
hypotension without a significant decrease in pulse pressure.
Pulse pressure: Systolic blood pressure - Diastolic blood pressure
Pulse assesment: Palpating the patient’s pulse can give us quick information about
his hemodynamic state, when radial pulse is perceived, it can be
inferred that the patient has a PAS> 100 mmHg, when the brachial
pulse is perceived, it is inferred that a PAS> 80 mmHg is inferred
and when Only the carotid pulse is perceived, it is estimated that the
patient has at least 60 mmHg of PAS, when there is no radial pulse, we
should immediately look for the cause of the drop in blood pressure
and resolve it as soon as possible [12].
Pulse pressure:
Hemodynamic variable easily measured that is the result of the
subtraction of systolic blood pressure minus diastolic blood pressure
and whose normal value is around 40 mm Hg.Pulse pressure: Systolic blood pressure -Diastolic blood pressure (PP= SP-DP)
Systemic pulse pressure is approximately proportional to systolic
volume (assessing cardiac pump function, preload and afterload)
and inversely proportional to the distensibility of the arterial system,
especially the aorta. It is a simple way of assessing ventricular
elastance and arterial instability, shaping the arterial ventricle
coupling. The arterial system performs the function of cushioning the
volume ejected by the left ventricle. If the pulse pressure is extremely
low, that is: less than 25 mmHg or less, the cause may be low systolic
volume such as hypovolemia, cardiogenic shock or obstructive shock,
it may also be caused by congestive heart failure or stricture of the
aortic valve In the case of a hypotensive patient with a state of shock,
maintaining a normal pulse pressure suggests that the most likely
cause is vasodilation [13].
Heart rate assesment (HR):
All cardiac myocytes in the embryonic heart have pacemaker
properties. Some myocytes synthesize large amounts of contractile
proteins to become “functional” myocardium, others retain the
ability of pacemakers and generate electrical impulses. The Sinoatrial
Node (SA) in humans is about 8 mm long and 2 mm thick. It is
found in the groove where the superior vena cava joins the right
atrium. The autonomic nervous system controls various aspects of
cardiac function, including the frequency with which the heart beats,
however, cardiac function does not require all intact nerve pathways
since a completely denervated heart (a heart transplant recipient) can
adapt well to stressful situations.The pacemaker trigger frequency is usually controlled by the
activity of both divisions of the autonomic nervous system. The
increase in sympathetic nerve activity, through the release of nor
epinephrine and adrenaline, increases the heart rate mainly by
increasing the slope of the pacemaker’s potential, this mechanism of
increasing the heart rate works during physical exertion, anxiety and
certain diseases, such as febrile infectious diseases. On the contrary,
the increase in vagal activity, through the release of acetylcholine,
decreases the heart rate by hyperpolarizing the pacemaker’s cell
membrane and reducing the slope of the SA node potential.
Cardiac Output (CO) depends on Heart Rate (HR) and Stroke
Volume (SV); the increase in heart rate being the most important
mechanism to increase cardiac output quickly.
Cardiac output =Heart rate × stroke volume.
Tachycardia, defined as a heart rate> 100 beats/min regularly
occurs in situations of increased metabolic oxygen demand with the
need for an increase in cardiac output or in conditions associated with
decreased systolic volume with intact myocardium (eg hypovolemic
shock or obstructive) due to the decrease in preload (volume decrease)
and also in situations of impaired systolic heart function. Since
tachycardia reduces the diastolic time during which ventricular filling
occurs, systolic volume may decrease at high heart rates, this has its
highest expression in unstable or symptomatic tachyarrhythmias
(example: supra ventricular tachycardia with low cardiac output data
); This, however, only becomes clinically significant in patients with
myocardial relaxation disorders that cause decreased diastolic filling.
Tachycardia also occurs in situations of increased sympathetic tone,
that is, pain, anxiety and combative response.
Sinus tachycardia is always an undesirable sign, and its cause
must always be determined. An initial CF> 105/min and a sustained
HR> 90 to 95 beats/min in patients with shock status are associated
with an increased risk of death [14].
The higher the HR, the more severe the situation, the HR decreases
with age, so an HR> 110/min in an elderly patient is a very worrying
sign. The clinical context and disorders of the other vital signs are
important to assess the implications of a tachycardia.
Tachycardia in combination with hypotension (SBP<110 or
MAP<75 mmHg) and a high respiratory rate (> 20/min) should
make us think about performing interventions on the patient [15]. It
should be emphasized that, in almost all circumstances, one should
treat the underlying cause (if possible) of the tachycardia and not the
tachycardia itself, this is very routine in daily practice with adding a
beta-blocker to the indications however You run the risk of increasing
the chance of an acute adverse cardiac event. However, in patients
with diastolic dysfunction, reducing HR can improve diastolic filling,
therefore, increase systolic volume and improve macrohemodynamic
variables such as an increase in BP, in refractory septic shock this
possibility can be considered with beta-blocker. intravenous with HR
goal close to 90/min.
In an episode of HR> 150/min (SVT) without underlying
extracardiac cause it should be considered to use intravenous vagal
or anti-arrhythmic maneuvers, in case the SVT is accompanied by
symptoms (hypotension, chest pain, dyspnea, neurological alteration,
etc.) it should alert to take an immediate action to reduce the HR that
corresponds to a synchronized electrical cardioversion and possibly
the use of anti-arrhythmic drugs in case of not obtaining a good
therapeutic response.
At the other end we have bradycardia. Sinus bradycardia is
defined as a heart rate of less than 60 beats/min. Patients with sinus
bradycardia usually have a frequency between 45 and 59 beats/min,
but rarely can be as slow as 30 beats/min. Sinus bradycardia is often
benign and does not necessarily indicate sinus node dysfunction.
In the context of the critical patient, sinus bradycardia is most
often due to a pharmacological reaction (eg sedatives), but it can
occur in patients with intrinsic disease of the conductive tissues
of the heart. Bradycardia can also present before, hypothermia,
hypothyroidism and elevated intracranial pressure. The medications
most commonly involved include beta blockers, calcium antagonists,
dexmedetomidine, Propofol, clonidine and digoxin.
Dexmedetomidine, an alpha-2 receptor agonist, decreases the
production and response to catecholamines and leads to bradycardia
due to these sympatholytic effects. Proprofol induces bradycardia
by blocking calcium and potassium channels in heart cells. While
Propofol and dexmedetomidine alone have a relatively low incidence
of bradycardia when used in combination with other AV nodal block
medications, the risk of bradycardia increases [15].
Bradycardia <50 beats/minute accompanied by symptoms
(hypotension, dyspnea, neurological disturbance, chest pain, etc.)
indicates that we should start an immediate treatment, the use of
atropine is recommended in this situation, if it is not resolved, a
chronotropic can be used positive as dopamine in infusion and
consider the use of a pacemaker.
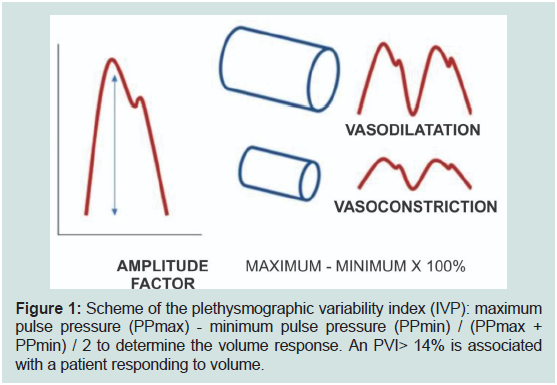
Assesment of the plethysmographic curve:
One of the hemodynamic assessment tools available from the
pre-hospital environment, to the emergency room and other critical
areas is the plethysmographic wave analysis observed with the pulse
oximeter. The plethysmographic pulse wave figure is illustrated as
a mirror image of the pulsatile vessel light intensity wave, whose
variations in wave size are due to changes in local blood volume and
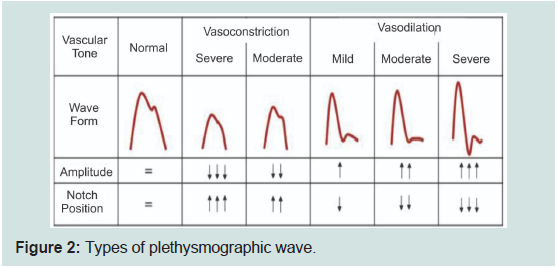
vascular resistance [16].The shape of the plethysmographic pulse curve can provide
information on the current state of peripheral vascular resistance and
the heartbeat volume. The amplitude of the plethysmographic wave
is related to the vascular state of the peripheral arteries as follows:
the larger the amplitude of the wave, this will be associated with a
mild, moderate or severe vasodilation, on the contrary, the smaller
this amplitude will be related to peripheral arterial vasoconstriction.
Likewise, the position of the notch of the dicrota wave in relation to
the level of amplitude of the maximum systolic peak does not offer
certain information: if the position of the notch is above 50% of
the amplitude, the tendency will be vasoconstriction, instead If the
position of the notch of the dicrota wave is below 50% of the amplitude
of the plethysmographic wave, the tendency will be peripheral arterial
vasodilation. Clinically we can infer that a patient who presents
hypotension accompanied by a plethysmographic vasodilation
pattern, the type of causal shock will be distributive (vasodilated), in
case, on the contrary, it is associated with a vasoconstriction pattern,
it is inferred that the type of Shock will be one that affects systolic volume (hypovolemic, cardiogenic, obstructive) (Figure 1 and 2) [17].
Figure 1: Scheme of the plethysmographic variability index (IVP): maximum
pulse pressure (PPmax) - minimum pulse pressure (PPmin) / (PPmax +
PPmin) / 2 to determine the volume response. An PVI> 14% is associated
with a patient responding to volume.
Shock Index and Modified shock index:
The Shock Index (SI) is a rapidly obtained parameter that indicates
severity and tendency in the patient, which is the result of dividing
the heart rate between systolic blood pressure, due to its simplicity
and applicability have been the subject of study by different authors,
so that if it is elevated, it can be assumed that there is a decrease in
systolic volume or a decrease in systemic vascular resistance [18].The normal range of the shock index for healthy adults is 0.5 to
0.7. In non-pregnant patients, the shock index is useful for detecting
shock at early stages, even more than conventional vital signs,
especially in patients with trauma shock or sepsis of non-specific
origin.
The Modified Shock Index (MSI) is a variant determined by heart
rate and Mean Blood Pressure (MAP), a reported cut (<0.7 and>
1.3) as a better predictor of mortality than the conventional shock
index. A study that analyzed more than 9000 patients who went to
the emergency room concluded that the MSI was significantly better
than clinical parameters such as HR, SBP, DBP and SI only to predict
mortality. The MSI has been highly associated with mortality is above
1.8 [19].
Anything that increases HR or decreases BP will modify SI, so
the clinical picture must be taken into account. Among the factors
that can modify the SI and the MSI are the presence of pain and
anxiety, which can cause tachycardia and thereby increase the values
of the indices, or the measurement of blood pressure with manual
or automatic systems. It is known that taking blood pressure with
automatic systems increases blood pressure and thereby decreases the
values of these indices [20].
Perfusion windows:
Since 1961 it is stated that it may be better to recognize the state
of shock than to define it, so we must direct the intentional search
for this pathological state through the clinical windows, which give
us a wide and accurate picture of the patient taking tissue perfusion
ineffective [21].Mental status:
Changes in mental state occur early in the course of circulatory
failure. Recent developments in scoring systems have revealed
that changes and fluctuations in mental state and/or attention,
the presence of disorganized thinking and an altered level of
consciousness are related to an abnormal brain function, which may
be caused by alterations in cerebral oxygen supply and/or decrease in
microcirculatory perfusion at that level [22].We will set the stage for a state of shock with decreased cardiac
output, both low cardiac output and low blood pressure contribute
to changes in perfusion and brain function [23]. In the so-called
distributive shock, cardiac output is preserved, but the Loss of
self-regulatory mechanisms due to the activation of Nitric Oxide
Synthetase (iNOS) may result in abnormalities of micro circulatory
perfusion leading to the loss of adequate perfusion and function [24].
In case of septic shock, the inflammatory response to the infection
itself leads to changes in mental status [25], nowadays it is generally
known as encephalopathy associated with sepsis, where changes in
metabolism can cause an abnormal disorder. Mental status in these
patients similar to delirium status.
Like many clinical signs described in the field of circulatory
insufficiency, a change in mental status is neither sensitive nor
specific. However, a patient who has a sudden change (hours) in brain
function should be carefully examined for possible circulatory failure,
while an abnormal mental state in a patient with clear circulatory failure may be a warning sign that a patient It is reaching the limits of
compensatory mechanisms [26].
Temperature:
The skin is the main organ in thermoregulation and has no selfregulating
mechanisms; A decrease in skin perfusion results in a
decrease in local temperature. Understanding that cold and moist skin
has long been seen as an important symptom of impaired circulation
of different origins [27], therefore, cold skin, even in patients with
sepsis, is an early sign of circulatory failure [28]. Few studies have
demonstrated abnormal hemodynamic profiles in patients with cold
skin to the touch, most of them corresponding to cardiogenic shock.A mixed cohort review showed that cold skin patients were
associated with lower cardiac output (GC), mixed mixed venous
oxygen saturation and higher lactate levels. A sweaty skin and cold to
the touch can correlate with elevated lactate levels, high veno-arterial
difference of CO2 (DvaCO2) high and low SvcO2.
The difference of the central temperature at the feet (Tc-toe) has
been a proposed strategy such as the difference between the central
temperature measured in tympanic membrane and the temperature
in the ventral surface of the big toe that has been used as a measure of
vasoconstriction peripheral as a result of a shock state, however it has
the disadvantage of being affected by hypothermia and the ambient
temperature.
The temperature gradient between the tip of the finger and the
forearm (Tskin-diff) has also been used as a marker of peripheral
vasoconstriction peripheral Tskin-diff is the difference between the
temperatures on the index finger and on the radial side of the forearm,
which It has the advantage of not being affected by the environment
because the change in external temperature affects both the fingertip
and the forearm alike.
Skin:
The skin is the first organ to sacrifice blood flow before a state of
circulatory shock, so it will give visible manifestations quickly and
with an adequate correlation with other clinical and biochemical
parameters of tissue hypoperfusion at other levels. A pale or mottled
skin recognized early indicates strong suspicion of inadequate tissue
perfusion. In current reviews (Coudroy col) [29]; It was found that
almost a third of the patients admitted to the ICU had mottled skin,
while this was present in almost 50% of patients with septic shock
since their admission to the emergency area.Spotted skin is defined as “irregular skin coloration” and is the
result of heterogeneous vasoconstriction of the small peripheral
vessels, skin spots usually manifest around the knees and may extend
to other peripheral circulation sites such as fingers and ears Initially
When mottled skin is observed over a large area, it is a sign that the
patient is in danger of death, patients with a higher speckled score
are more likely to die even on the first day of admission, therefore
it should be considered an emergency Medical regardless of blood
pressure, it is important to mention that mottling is not modified
with pressure on the skin on physical examination [30].
There is a direct relationship in the mottle score with the amount
of serum lactate, the latter being a faithful marker of lethality in the
absence of other possible causes of hyperlactatemia such as previous liver disease, drug exposure and inborn errors of metabolism. Oufella
et al. they found a direct relationship between mottled and lactate
with a p = 0.0001 [31].
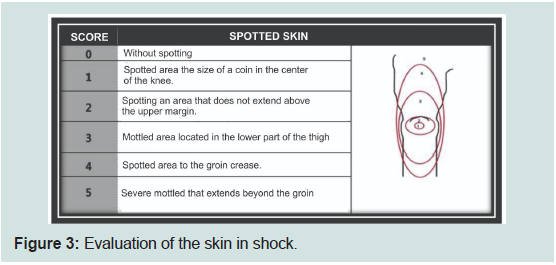
There are several mechanisms involved associated with mottled
skin: a poor distribution of blood flow, loss of vascular self-regulation
and an increase in metabolites of nitric oxide synthetase. The
mottled index proposes six degrees associated with gravity, (0 to 5)
and depends on the extent of the mottled skin up the knee. Higher
spotting index score (score of 4 to 5) is associated with high mortality
in patients with septic shock. Spotted skin prolonged for more than
6 h was associated with higher mortality in the ICU regardless of
scoring systems severity (Figure 3) [32].
Capillary filling time:
The capillary filling time measures the amount of time necessary
for the skin to return to its initial color after applying pressure for
a few seconds on a soft tissue (usually finger or knee area), initially
used as a diagnosis and monitoring of patients Pediatric patients with
hypovolemic shock because it provides important information on
skin perfusion and microcirculatory status and is an attractive and
easy-to-use tool for doctors in the initial detection of critical patients
[33]..It is recommended to perform it by applying firm pressure for
15 s, long enough to remove blood from the nail bed. It has been
shown that capillary filling time is related to more objective perfusion
measurements, even than temperature gradients. Capillary filling
under normal conditions lasts less than 2 s, values greater than 2.5
to 5 s are associated with higher mortality, especially if they persist
steadily and have a direct association with elevated serum lactate,
elevated DvaCO2 and decreased SvcO2.
The evaluation of capillary filling measured by applying firm
pressure to the ventral surface of the right index finger, for 10 s, the
time for the return of normal skin color was considered abnormal > 3 s corresponding to a lactate value ≥ 2.0 mmol/L, both as tissue
hypoperfusion data [4,34]. To date, the best evidence with statistical
significance emphasizes the time of capillary filling with better utility
in the evaluation of patients with circulatory insufficiency [35].
Uresis:
One of the main functions of the kidney, is to filter the blood
and eliminate waste and excess fluids, an early sign of an impaired
renal perfusion is the decrease in urine production, in a standardized
way oliguria is taken as a uresis <400 at 500 ml/day or <0.5 to 1 ml/
kg/h. Renal injury can occur due to decreased cardiac output, but
also due to direct inflammation in the nephron, which is the case
of sepsis, even a worsening of the renal lesion has been described in
patients with sepsis and septic shock to which it is applied increased
contribution of crystalloid or colloid volume of hydroxyethyl-starch
type, which suggests that the renal lesion in pro-inflammatory states
is not volume dependent, but of inflammation to the nephron per se.Studies of patients with early septic shock and post-operated
cardiac surgery have shown to have significantly lower urine output
despite a similar macro-hemodynamics [36]. The reason for this
dissociation is multifactorial, since many factors are related to the
decrease in renal function in sepsis. However, tubular injury is
unlikely to be a concomitant factor; the term acute tubular necrosis
should be avoided to address renal dysfunction in acute circulatory
insufficiency, especially if it is associated with a systemic inflammatory
response [37].
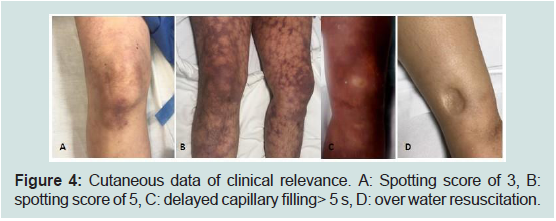
The presence of a decrease in urine production with a threshold
of 0.5 ml/kg/h represents a specific and sensitive parameter to
diagnose and treat acute circulatory insufficiency due to the risk of
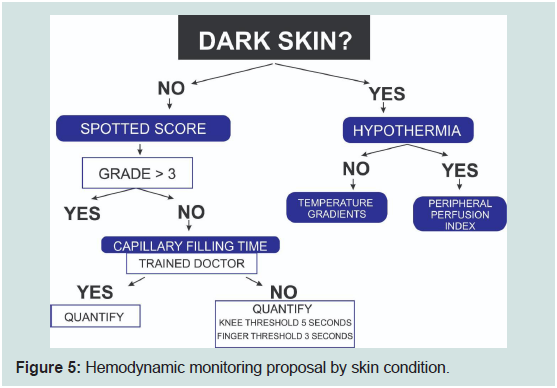
renal insufficiency and associated mortality (Figure 4 and 5).
Figure 4: Cutaneous data of clinical relevance. A: Spotting score of 3, B:
spotting score of 5, C: delayed capillary filling> 5 s, D: over water resuscitation.
Discussion
Clinical hemodynamic monitoring at the patient’s bedside is a useful tool, free of charge, highly reproducible and with evidence that
supports its efficacy compared to other minimally invasive or invasive
methods. Hassanin has described the applicability of clinical perfusion
indices: delayed capillary filling, mottling score and its relationship
with the patient’s prognosis, which provide the same information
as other methods such as central venous oxygen saturation or venoarterial
difference of CO2, without the need to perform a puncture
and laboratory analysis.
The ANDROMEDA randomized controlled study presented a
holistic vision based on pathophysiology and physiology with goalguided
therapy, observing that a CRT> 3 s corresponds to a lactate
value ≥ 2.0 mmol/L, these data corresponding to effective tissue
hypoperfusion , the manuscript concludes that there is no added
benefit when measuring lactate compared to the CRT measurement,
generating a better use of resources due to cost reduction, it is even
associated with prevention of over-resuscitation and evidencing
decrease in mortality at 28 days when goal-guided therapy is
performed.
The use of capillary filling time, mottle score and other clinical
features such as tissue perfusion indices require a significant context,
using it as a universal detection tool in each patient could have
limited value in some cases (skin patients obscure, patients without
lower extremities, patients with previous neurological alteration,
etc.), however of the available studies, the clinic is present in all cases,
it should not be forgotten that the worst hemodynamic monitoring
is the one that “is not done” and having the premise that “less is
more”, however, it is prudent to consider whether the patient requires
another type of more advanced evaluation in the clinical course of
his pathology in case of not obtaining good results with the initial
therapy.
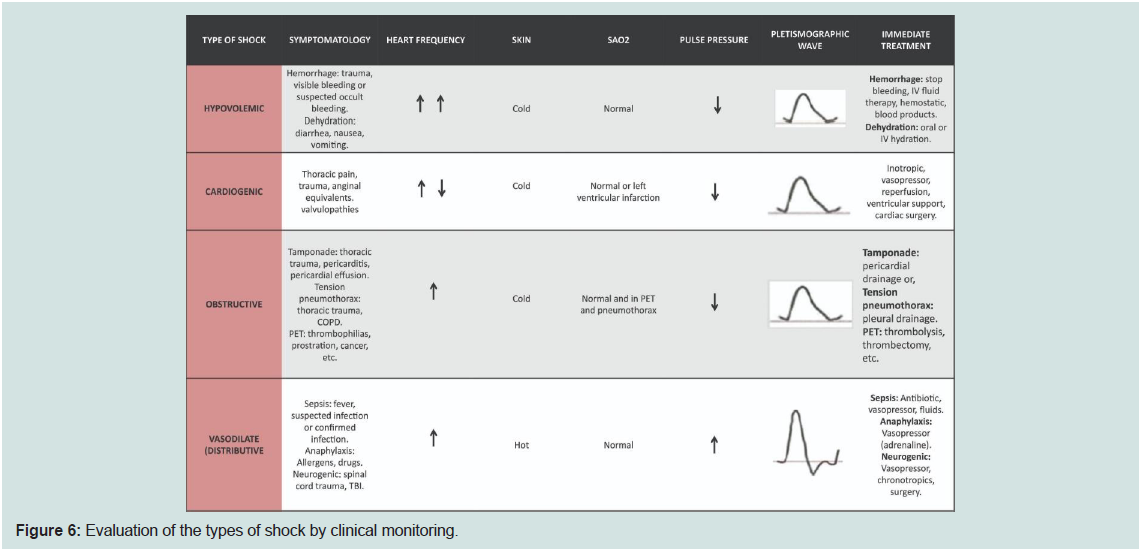
Conclusion
The clinic is a useful tool, highly reproducible and with good
correlation with other markers of tissue perfusion, it is recommended
to use it for early diagnosis of the states of shock and tissue
hypoperfusion, as well as monitoring the therapeutic response to
the patient’s bedside, we summarize the main clinical scenarios in
Figure 6, with this you can evaluate your patients through clinical
monitoring.