Journal of Emergency Medicine & Critical Care
Download PDF
Research Article
Pediatric Mortality andPreventable Death at a Mature Trauma Center
Nicole Fox1*, Stacey Staman2, Anna Goldenberg3 and Rahul Kumar John Porter4
- 1Department of Surgery, Cooper Medical School of Rowan University, New Jersey
- 2Pediatric Trauma Program Manager, Cooper Medical School of Rowan University, New Jersey
- 3Department of Surgery, Cooper Medical School of Rowan University, New Jersey
- 4Director of the Center for Trauma Services, Cooper Medical School of Rowan University, New Jersey
Address for Correspondence: Nicole Fox, Department of Surgery, Cooper University Hospital, 1-Cooper Plaza Camden, New Jersey, USA, Tel: (856) 342-3341;Fax: (856) 342-2817; E-mail: fox-nicole@cooperhealth.edu
Citation: Fox N, Staman PVS, Goldenberg A, Porter J. Pediatric Mortality and Preventable Death at a Mature Trauma Center. J Emerg Med Critical Care 2018;4(1): 4.
Journal of Emergency Medicine & Critical Care | ISSN: 2469-4045 | Volume: 4, Issue: 1
Submission: 18 April, 2018| Accepted: 17 May, 2018 | Published: 28 May, 2018
Submission: 18 April, 2018| Accepted: 17 May, 2018 | Published: 28 May, 2018
Copyright: © 2018 Fox N. et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objectives: It is critical to review pediatric mortality and identify preventable/potentially preventable death (PD). We sought to characterize mortality in pediatric trauma patients at our center and identify causes of PD.
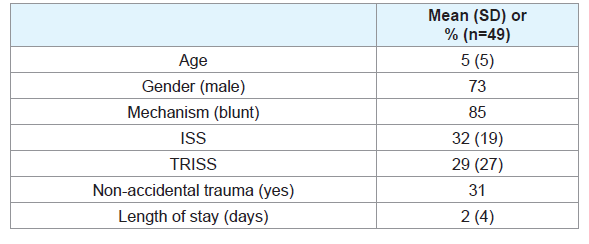
Methods: A retrospective review of pediatric (<14) trauma deaths (2006-2016) at our American College of Surgeons verified level 1 adult/ level 2 pediatric trauma center was conducted. Patients that died from burns, drowning or hanging were excluded. Demographics, clinical characteristics, and autopsy data were collected. Injury severity (ISS) and trauma & injury severity (TRISS) scores were calculated for each patient. Injuries were classified as non-survivable if they involved an ISS of 75. Death after non-survivable injury was considered nonpreventable. A multi-disciplinary panel reviewed all mortalities and rendered decisions regarding preventability and causes of PD.
Results: 49 of 3,065 patients died over the study period (MR=1.6%). Patients that died were primarily male (73%) with severe injuries (ISS 32 (19)) caused by a blunt (85%) mechanism. Fifteen deaths (31%) were the result of non-accidental trauma (NAT). Seven patients had an ISS of 75 indicating non-survivable injuries. After calculating TRISS on the remaining 42 patients, 12 patients had a >50% probability of survival. 25% of patients with a TRISS >50% were determined to be PD’s for an overall preventable death rate (PDR) of 6%. Failure to control hemorrhage (67%) and failure to secure an airway (33%) were the causes of PD.
Conclusion: We identified a PDR of 6% at our institution and found that a TRISS >50% correlates significantly with PD.
Introduction
Traumatic injuries (both accidental and intentional) are the leading cause of death and disability in adolescents and young children. Over 10 million children annually require hospital care for the evaluation and treatment of traumatic injuries and the cost of pediatric trauma is estimated to be approximately $14 billion in lifetime medical spending [1]. In light of its overall physical, emotional and financial impact, pediatric injury is considered a major public health problem in the United States [2].
A significant amount of research has focused on improving survival in pediatric trauma patients. In 1984, Ramenofsky and colleagues evaluated 100 consecutive pediatric trauma deaths. They concluded that the majority of errors leading to death in potentially salvageable patients occurred in the field, illustrating a need for pre-hospital education [3]. There is a paucity of literature, however, evaluating causes of in-hospital pediatric trauma mortality and reasons for preventable death (PD). In 1999, Esposito et al critically reviewed 77 in-hospital pediatric trauma deaths and concluded that 16% were preventable or potentially preventable. The primary causes of PD identified were a “lack of recognition and ability to treat straightforward problems with airway, breathing and circulation.” The patients in this study were treated in a variety of settings across the state of Montana and the authors noted that the study period “predates trauma system development and was selected to allow for a post-system comparison in subsequent years” [4]. In 2009, Diamond et al showed a significant decline in the pediatric PD rate in Ontario over a 20 year period after the development of a trauma system (21% vs. 7%). The leading cause of PD over the study period was uncontrolled hemorrhage, primarily from abdominal injuries [5].
Our primary study objective was to critically review and characterize in-hospital pediatric mortality within a mature (adult and pediatric) trauma center. In addition, we sought to identify and determine the primary causes of PD in this setting.
Materials and Methods
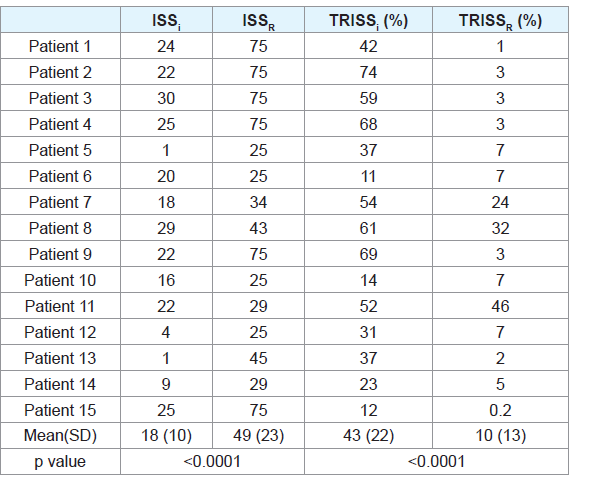
A retrospective review of all pediatric (<14) trauma deaths from 2006-2016 at our American College of Surgeons verified level 1 adult/level 2 pediatric trauma center was conducted. This study was reviewed by the institutional review board (IRB) and deemed exempt from ongoing IRB oversight due to the minimal risk to the study population as they were deceased. Patients were excluded if they died from burns, drowning or hanging. The primary study objective was to characterize in-hospital pediatric trauma mortality. The hospital charts of deceased patients (n=49) were reviewed and demographic and clinical characteristics were abstracted. Patient characteristics including age, sex and mechanism of injury were assessed along with clinical variables. Injury severity (ISS) and trauma & injury severity (TRISS) scores were calculated for each patient. Autopsy reports (if available) were used to re-calculate ISS and TRISS when additional injuries were discovered at the time of autopsy.
The primary study endpoint was PD. Injuries were classified as non-survivable if they involved an ISS of 75. Death after non-survivable injury was considered non-preventable. All other injuries were considered to be survivable. Death after survivable injury was considered preventable/potentially preventable and subject to further review. PD was defined in this study as “death which could be avoided if optimal care was delivered”. To be deemed preventable a trauma death must meet three criteria: the injuries produced by trauma and its sequelae must be survivable, the care which has been delivered must be suboptimal when compared with standards and the identified errors in the delivery of care have directly or indirectly contributed to patient outcome.
All pediatric trauma deaths were reviewed by the trauma medical director and presented at monthly morbidity and mortality conference. Deaths were then critically reviewed a second time by a multi-disciplinary panel which ultimately rendered decisions regarding preventability and causes of PD using the criteria outlined above. Within the study period (2006-2016), our trauma center was reviewed twice by the American College of Surgeons. Members of the trauma verification team provided a third level of review for two years of the study, 2014 and 2016. The verification team reviewed all pediatric deaths as part of the review process to become a verified level 2 pediatric trauma center.
The PDR was defined as the total number of preventable deaths divided by the total number of deaths over the study period. Data were reported as percentages or means (SDs). Categorical variables were analyzed using the χ2 or Fischer’s exact test while continuous variables were evaluated with Student’s t test. A p≤0.05 was considered statistically significant.
Results
3,065 patients were admitted over the study period and 49 died (mortality rate=1.6%). Patients that died were primarily male (73%) with severe injuries (ISS 32 (19)) caused by a blunt (85%) mechanism. Fifteen deaths (31%) were the result of non-accidental trauma (NAT). Characteristics of study patients are presented in Table 1. Autopsy reports were available in 27 (55%) of cases. Based on autopsy findings, 15 of 27 (55%) patients required revision of both ISS and TRISS, resulting in a significant increase in ISS and decrease in TRISS (Table 2).
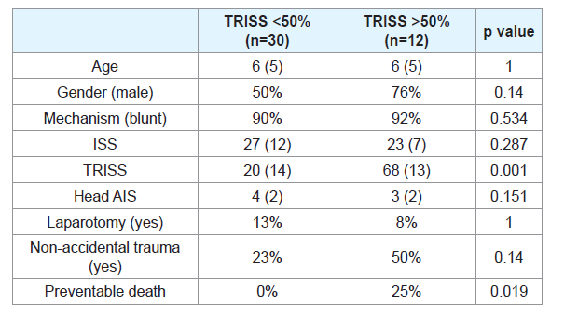
Seven patients had an ISS of 75 indicating non-survivable injuries. After calculating TRISS on the remaining 42 patients, 12 patients had a >50% probability of survival and 30 patients had a <50% probability of survival. There were no differences in age, gender, mechanism, ISS, head abbreviated injury scale (AIS) or rate of NAT between the two groups. All of the preventable deaths (n=3) occurred in patients with TRISS >50% (Table 3).
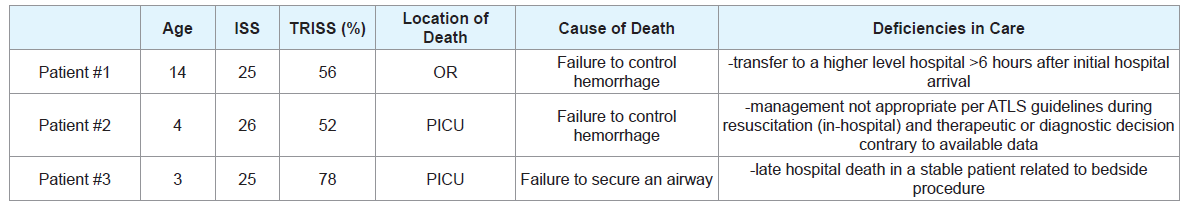
After multi-disciplinary review, three deaths were classified as preventable resulting in a PDR of 6%. The cause of death in two cases was failure to control hemorrhage and subsequent exsanguination. The cause of death in the third case was failure to secure an airway leading to respiratory arrest followed by cardiac arrest. Two of the PDs occurred in the pediatric intensive care unit (PICU) and one occurred in the operating room (OR). Table 4 provides a summary of the PDs.
Discussion
Our data indicates that the overall mortality rate for pediatric trauma patients admitted to a mature (adult and pediatric) trauma center is low at 1.6% and the majority (57%) of patients that die have severe traumatic brain injuries (head AIS >4). The most important findings of the current report are that the PDR for pediatric trauma patients was 6%. Furthermore, a TRISS >50% correlates significantly with PD. Autopsy reports, when available, assist in the accurate calculation of ISS and TRISS and may clarify the actual cause of death in some cases.
Overall mortality rate is not an adequate reflection of pediatric trauma center performance and/or quality of care as the overall mortality rates in children are generally low. Several studies have attempted to determine which types of centers provide the best care to injured children (pediatric trauma centers v. adult trauma centers v. mixed trauma centers), however these studies use overall in-hospital mortality rates as a basis for comparison [5-9]. We believe that the PDR is a more appropriate area of focus as it quantifies the number of patients who died as a result of deficiencies in care. In-hospital PD has not been well characterized in pediatric trauma patients and a baseline PDR has not been established for comparative purposes between centers. Our process of identifying PD included individual case review of all pediatric deaths in trauma M&M conference as well as a subsequent secondary review by a multi-disciplinary panel that included the adult and pediatric trauma medical directors. As stated previously, a third level of review was performed by site reviewers from the ACS of 2014 and 2016 deaths.
Through this intensive review process, three PD’s were identified over the study period. Two deaths were a result of uncontrolled hemorrhage. One of these patients was transferred to our facility after initial presentation to a non-trauma center. She was a restrained backseat passenger in a motor vehicle collision with a Glasgow Coma Score of 15 at the scene complaining of abdominal pain. At the initial hospital she was taken to the operating room (OR) for the management of spleen and liver injuries. Surgeons were unable to control hemorrhage and she was transferred directly from the OR at the initial facility to the OR at our trauma center. The total time from her accident to transfer to a trauma center was seven hours. On arrival to the trauma center she was acidotic, hypothermic, coagulopathic and expired in the OR. From the operative notes, these appeared to be survivable injuries with a failure to control hemorrhage and subsequent exsanguination. The second patient was ejected from a motor vehicle and sustained traumatic liver lacerations with active extravasation, a right renal laceration with adrenal hematoma and left lung lacerations. The patient was taken to interventional radiology for angioembolization of the liver and admitted to the pediatric ICU (PICU). Approximately 7 hours after admission, the patient had a drop in hemoglobin to 6, became hypotensive and bradycardic, progressed to PEA arrest and expired in the PICU. On review, this was considered a potentially PD related to ongoing, unrecognized hemorrhage.
The third PD was classified as failure to secure an airway in a patient initially admitted after being “found down” at home and unresponsive with injuries concerning for non-accidental trauma. He had a traumatic subdural hemorrhage, required craniectomy and was admitted to the PICU. On day 19 of his hospital stay he became bradycardic and desaturated and the determination was made that his tracheostomy was occluded. A bedside tracheostomy change was attempted however the patient progressed to cardiac arrest during this procedure and expired. On review, this was considered a PD related to inability to secure an airway.
The PDs identified in this study represent opportunities for trauma performance improvement (PI). According to the American College of Surgeons Committee on Trauma, an effective PI process requires monitoring clinical processes, outcomes and systems issues and identifying sentinel events. The process must also result in the development of corrective actions for these events to prevent future recurrence [10]. In the case of the patient initially brought to a nontrauma center, extensive education and outreach was conducted with pre-hospital providers as well as surrounding hospitals (non-trauma centers) to emphasize the importance of bringing the “right patient to the right place the first time”. To mitigate systems issues and decrease delays, a transfer center was subsequently established at our hospital to ensure maximum efficiency for patient transfers. In addition our institution committed to becoming verified as a pediatric trauma center.
The in-hospital PD from exsanguination required individual provider education and remediation by the trauma medical director. In the case of the PD from a failure to establish an airway, a multidisciplinary group established an emergent airway protocol for the institution that clearly outlined the escalation pathway for assistance in difficult airway cases. All trauma providers were oriented to the protocol and adherence to the protocol is prospectively monitored.
The use of autopsy reports to calculate accurate ISS and TRISS was an important part of this retrospective review. In 1981, West JG advocated the use of autopsy reports as an inexpensive and valuable method to evaluate trauma care [11]. Ramenofsky ML et al. also used available autopsy reports to determine survivability in pediatric trauma patients [3]. In our review, there were several patients that died shortly after presentation without the benefit of CT scans to identify injuries. These patients had erroneously low ISS and high TRISS. Exhaustive attempts were made to collect autopsy reports from the office of the medical examiner and all available reports were reviewed by the trauma medical director and incorporated into the secondary review process. The trauma registry was updated to reflect the re-calculated ISS.
TRISS was also calculated specifically to determine whether or not higher TRISS were associated with PD. In 1991, Kaufmann CR et al. evaluated the validity of applying TRISS to injured children. They determined that despite the physiologic differences between adults and children, TRISS was applicable to children and a valuable tool to evaluate pediatric trauma care [12]. In 2006, Aaland et al also advocated the use of risk-adjusted mortality based on TRISS to critically evaluate pediatric trauma deaths [13]. Stelfox HT et al. systematically reviewed quality indicators for evaluating pediatric trauma care and suggested that “TRISS analysis may be a useful tool for identifying children with unexpected deaths whose care should be further reviewed” [14]. The results of our review support this statement as we found that all PD’s occurred in patients with a TRISS >50%. As a result, we currently calculate TRISS for all pediatric trauma deaths and apply the primary and secondary review process outlined previously those with a TRISS >50. Patients with a TRISS <50 are reviewed once during trauma M&M.
Conclusion
In conclusion, the overall PDR for pediatric trauma patients is 6% at a mature trauma center. A TRISS >50% correlates significantly with PD. The causes of PD in the pediatric population were failure to control hemorrhage and failure to secure an airway.
References
- Miller TR, Romano EO, Spicer RS (2000) The cost of childhood unintentional injuries and the value of prevention. Future Child 10: 137-163.
- Sharar SR (2012) The ongoing and worldwide challenge of pediatric trauma. Int J Crit Illn Inj Sci 2: 111-113.
- Ramenofsky ML, Luterman A, Quindlen E, Riddick L, Curreri PW (1984) Maximum survival in pediatric trauma: the ideal system. J Trauma 24: 818-823.
- MacKenzie EJ (1999) Review of evidence regarding trauma system effectiveness resulting from panel studies. J Trauma 47 (3 Suppl): S34-S41.
- Esposito TJ, Sanddal ND, Dean JM, Hansen JD, Reynolds SA, et al. (1999) Analysis of preventable pediatric trauma deaths and inappropriate care in Montana. J Trauma 47: 243-253.
- Diamond IR, Parkin PC, Wales PW, Bohn D, Kreller MA, et al. (2009) Preventable pediatric trauma deaths in Ontario: a comparative population-based study. J Trauma 66: 1189-1195.
- Amini R, Lavoie A, Moore L, Sirois MJ, Emond M (2011) Pediatric trauma mortality by type of designated hospital in a mature inclusive trauma system. J Emerg Trauma Shock 4: 12-19.
- Pracht EE, Tepas JJ 3rd, Langland-Orban B, Simpson L, Pieper P, et al. (2008) Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? J Pediatr Surg 43: 212-221.
- Osler TM, Vane DW, Tepas JJ, Rogers FB, Shackford SR, et al. (2001) Do pediatric trauma centers have better survival rates than adult trauma centers? An examination of the National Pediatric Trauma Registry. J Trauma 50: 96-101.
- Aaland MO, Hlaing T (2006) Pediatric trauma deaths: a three-part analysis from a nonacademic trauma center. Am Surg 72: 249-259.
- West JG (1981) An autopsy method for evaluating trauma care. J Trauma 21: 32-34.
- Kaufman CR, Maier RV, Kaufmann EJ, Rivara FP, Carrico CJ (1991) Validity of applying adult TRISS analysis to injured children. J Trauma 31: 691-698.
- (2014) Resources for optimal care of the injured patient. Committee on Trauma American College of Surgeons, Chicago, USA, pp. 1-221.
- Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE (2010) A systematic review of quality indicators for evaluating pediatric trauma care. Crit Care Med 38: 1187-1196.