Journal of Clinical & Medical Case Reports
Download PDF
Case Report
Lung Cancer Metastasis to the Breast: Consideration of an unusual Presentation
Barron N1, MG Schammel C2, Rainer R2 and SchammelDP2
1Department of Internal Medicine, Prisma Health Upstate, Greenville
SC, USA
2Pathology Associates, Greenville SC, USA
Address for Correspondence:
MG Schammel C, USCSOMG, Pathology Associates, 8 Memorial
Medical Ct. Greenville SC 29605, USA E-mail: Christine.
schammel@prismahealth.org
Submission: 12 March, 2023
Accepted: 21 April, 2023
Published: 24 April, 2023
Copyright: © 2023 Barron N, et al. This is an open access
article distributed under the Creative Commons Attribution
License, which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
Abstract
Background: The EML4-ALK fusion oncogene is found in 2 to 7% of
all non-small cell lung cancers, most of which are adenocarcinomas.
These rare ALK-positive lung malignancies represent approximately 4%
of all adenocarcinoma non-small-cell lung cancer; metastatic spread
to the breast is exceedingly rare, with an incidence between 0.2-3% of
reported cases. Here we present a case of ALK-positive lung cancer
metastasizing first to the breast and then to the spine.
Case Report: A 60-year-old female with a left upper lobe pulmonary
lesion suspicious for malignancy underwent a wedge resection;
pathology revealed pulmonary adenocarcinoma with positive nodes.
While an EML4-ALK fusion was identified, the patient refused adjuvant
therapy. One month later, a 7mm lesion in the right lower mid-breast
was identified; a biopsy identified poorly differentiated carcinoma
consistent with lung origin. Pemetrexed, Cisplatin, and Carboplatin
were initiated. Two months later, with new onset of back pain, a
PET scan revealed a hypermetabolic bony lesion in the third lumbar
vertebral body. A biopsy revealed metastatic adenocarcinoma from
the lung. The patient began radiation therapy and, given the EML4-
ALK fusion, transitioned from standard chemotherapy to targeted
therapy. Currently, following the completion of radiation therapy, the
bony metastasis has resolved, and the patient continues to tolerate
targeted therapy well.
Conclusion: Metastases to the breast from other primary locations
account for only 0.2-1.3% of all breast malignancies, but most often,
these are lung cancer. EML4-ALK fusions are found in 2-7% of pulmonary
adenocarcinomas, but indicate the use of targeted therapy which
portends a high and durable response rate. This is the fifth EML4-ALK
fusion oncogene identified in lung cancer metastasis to the breast
that is managed with targeted therapy, emphasizing the importance
of bioanalysis in management.
Keywords
Lung cancer metastases; Metastases to the breast; EML4-
ALK fusions; Bioanalysis for targeted mutations
Abbreviations
EML4-ALK: (echinoderm microtubule-associated proteinlike
4)-(anaplastic lymphoma kinase); ALK: anaplastic lymphoma
kinase; ED: emergency department; CT: computed tomography;
PET: positron emission tomography; ER: estrogen receptor;
PR: progesterone receptor; Her-2: human epidermal growth
factor receptor-2; GATA3: transcription factor important in the
differentiation of breast epithelia
TTF-1: thyroid transcription factor 1; SOS-10: son of sevenless-10;
developmental protein that stops DNA repair; TKI: tyrosine kinase
inhibitor; Napsin-1: functional aspartic proteinase that is a new
marker for lung cancer.
Introduction
Lung cancer is the most commonly diagnosed cancer, with
over 238,000 cases and over 127,000 deaths expected in 2023 [1].
Lung cancer is classified into two categories: small-cell lung cancer, representing 15% of cases, and the more prevalent non-small cell lung
cancer representing 85% of cases [1].
The EML4-ALK fusion oncogene is found in 2 to 7% of all nonsmall
cell lung cancers, most of which are adenocarcinomas. These
gene rearrangements are more prevalent in females, young patients,
and non-smokers, as well as in Asian and Western populations [2].
Metastases typically present in the liver, adrenals, bone, and brain.
While there are treatments with molecularly targeted therapy, which
have been noted to increase survival [3], the prognostic significance
of the EML4-ALK oncogene is controversial [4].
Breast metastases from extramammary locations are rare,
representing 0.2%-1.3% of all breast malignancies [5], typically
portending a poor prognosis given that, in most cases, widely diffused
metastases of the primary cancer are often present at the time of
the breast metastasis discovery [5]. However, in the limited reports
of patients with EML4-ALK-positive lung cancer metastasizing the
breast, patients have demonstrated favorable outcomes to targeted
therapy. Here we present a case of ALK-positive lung cancer
metastasizing first to the breast and then to the spine.
Clinical Case
A 60-year-old female presented to the ED for dyspnea and
tachycardia. A CT angiogram of the chest incidentally revealed a left
upper lobe spiculated pulmonary lesion (1.4 cm) that was suspicious
for malignancy; no mediastinal hilar lymphadenopathy was noted.
CT/PET demonstrated a single hypermetabolic left upper lobe lesion
with no other evidence of disease. A robotic wedge resection and left
upper lobectomy were completed; pathology revealed an invasive
pulmonary adenocarcinoma that invaded the visceral pleura, as
confirmed on elastin stain, with negative margins; 1/12 nodes were
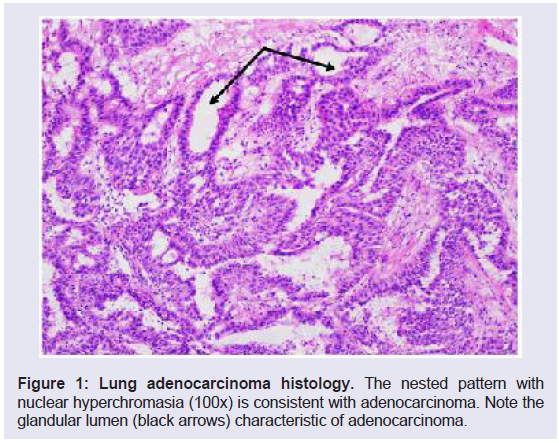
positive for metastatic carcinoma (T2aN1; Figure 1).
Figure 1: Lung adenocarcinoma histology. The nested pattern with
nuclear hyperchromasia (100x) is consistent with adenocarcinoma. Note the
glandular lumen (black arrows) characteristic of adenocarcinoma.
Biomarker analysis (FoundationOne; Cambridge, MA) identified
EML4-ALK fusion; the patient refused oral targeted therapy. Adjuvant cisplatin/pemetrexed was initiated; however, the patient terminated
therapy after one cycle due to nausea and facial swelling. Carboplatin/
pemetrexed was initiated, but after two cycles, was terminated by the
patient due to nausea.
Upon a routine screening mammogram one month later, a
new 7mm lesion in the right lower mid -breast, which had not
been visualized at the previous year’s screening, was identified and
felt to be suspicious. Subsequent ultrasound of the lesion revealed
posterior acoustic shadowing consistent with a solid lesion; a biopsy
was recommended and completed at an outside institution. Outside
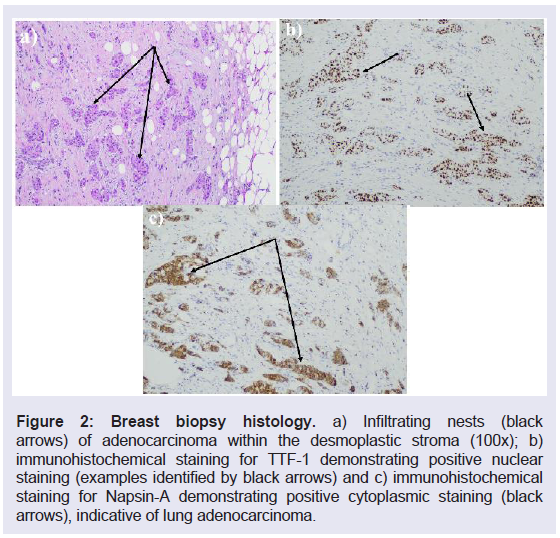
pathology reviewed at our institution noted a poorly differentiated
carcinoma inconsistent with a breast primary (Figure 2a) with a nonbreast
immunohistochemical profile (11% ER +, PR-, Her-2-); cells
were negative for GATA3 and mammoglobin, but were positive for
TTF-I (Figure 2b) and Napsin A (Figure 2c), suggesting a lung origin.
Figure 2: Breast biopsy histology.a) Infiltrating nests (black
arrows) of adenocarcinoma within the desmoplastic stroma (100x); b)
immunohistochemical staining for TTF-1 demonstrating positive nuclear
staining (examples identified by black arrows) and c) immunohistochemical
staining for Napsin-A demonstrating positive cytoplasmic staining (black
arrows), indicative of lung adenocarcinoma.
Concordance with the lung adenocarcinoma confirmed that the
breast lesion was consistent with metastatic lung cancer (GATA-
, mammoglobin -, TTF-1+, Napsin A+, SOS-10+). A staging PET/
CT scan revealed no uptake in the lung, minimal uptake in the
right breast lesion, and a concerning lesion at L3. MRI of the brain
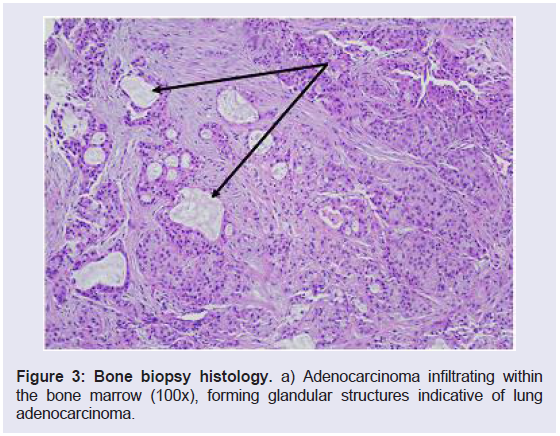
was negative for intracranial metastatic disease. An interventional
radiology vertebral biopsy revealed metastatic adenocarcinoma
diffusely positive for CK7, TTF-1, and Napsin A consistent with the
lung primary (ER and GATA3 negative; Figure 3).
Figure 3: Bone biopsy histology.a) Adenocarcinoma infiltrating within
the bone marrow (100x), forming glandular structures indicative of lung
adenocarcinoma.
Breast lumpectomy was completed; pathology identified
metastatic pulmonary adenocarcinoma forming a 0.8cm mass which
stained positive for TTF-1 and Napsin. All margins were negative,
with the closest margin being 1.2 cm
Radiation therapy for the bony lesion was initiated (stereotactic
body radiation to the L3 vertebral body; 700Gy for 5 days; total dose
3500Gy). Once the radiation was completed, and given the EML4-
ALK fusion, the patient was transitioned to, and continues to take,
targeted therapy (alectinib; Tyrosine Kinase Inhibitor; TKI). Serial
follow-up CT chest/abdomen/pelvis at three months for a year and
then every six months, along with brain MRIs every six months, have
revealed stable findings with no evidence of new or recurrent disease
18 months postdiagnosis.
Discussion
Breast cancer accounts for 30% of all cancers in women [6];
however, metastases to the breast from other primary locations
accounts for only 0.2-1.3% of all breast malignancies [5]. Tumors
most often metastatic to the breast are lung cancer (22% of cases),
lymphomas (15%), melanoma (13%), gastrointestinal cancers
(8%), and papillary serous carcinomas (4%) [7]. Typically, tumors
metastatic to the breast portend a poor prognosis as most patients
have widely disseminated disease [5].
Histologic analysis and immunohistochemical evaluation of
breast lesions can differentiate between primary and metastatic
disease. In the case presented here, the IHC of the breast lesion
indicated low ER expression with absent PR and Her-2, negative
GATA3 and mammaglobin [8,9], inconsistent with a breast primary;
the positive expression of TTF-1 and Napsin A, characteristic of 75%
and 84% of lung adenocarcinomas, respectively suggested lung origin [10,11]. While TTF-1 is one of the most commonly utilized IHC
markers in diagnosing lung cancers, it can also distinguish primary
lung adenocarcinoma from tumors of other sources, substantiating
the breast and spine lesions as lung metastases [12,13].
A comprehensive review of the literature noted 179 reports of
lung carcinoma metastases to the breast between 1965 and 2013. In
2013, a systematic review of 31 previously published cases (1989-
2013) identified that 87% of patients with lung metastases to the breast
were female, 62% were nonsmokers, and the median age of diagnosis
was 54. Pathologically, 58% of the tumors were adenocarcinomas,
none of which expressed ER, PR, or HER-2 positivity [14]. In the
case presented here, the presence of the EML4-ALK fusion in both
the lung primary and the breast and spine lesions not only suggested
metastatic disease, as EML4-ALK fusions are found in only 2-7%
of pulmonary adenocarcinomas [2,15,16], but also indicated use of
a targeted therapy that inhibits this fusion kinase and demonstrates
high and often durable response [17].
To date, there are only three other reports identifying the EML4-
ALK fusion oncogene in lung cancer metastasis to the breast and one
widely metastatic breast cancer with this genetic profile.
All patients were eventually managed with TKIs that showed
tumor regression [18,19,20].
Conclusion
Metastasis to the breast is an uncommon phenomenon but must
be considered upon discovery of a breast mass in a woman with a
history of cancer, especially primary lung cancer. Management of the
breast is not the primary concern in such cases, as is evidenced by the
current case where the additional systemic disease was discovered and
thus identified the need for effective systemic therapy. The current
management of non-small cell lung cancer demands an evaluation
of possible actionable mutations. Typically, biomarker assessment
is performed with nextgeneration sequencing panels looking for an
ever-growing number of mutations that indicate targeted therapy,
often oral agents with a high degree of initial disease control. As
noted in our case, targeted therapy allows for effective management
of a disease that would typically portend a poor prognosis.