Journal of Clinical & Medical Case Reports
Download PDF
Case Report
Foreskin Retraction and Circumcision: Possible Late Consequences
Jargin SV*
Department of Pathology, People’s Friendship University of Russia,
Russian Federation
Address for Correspondence:Jargin SV, People’s Friendship University of Russia, Clementovski
per 6-82, 115184 Moscow, Russia; Tel: 7 495 9516788; Email: sjargin@mail.ru
Submission: 06 December, 2021;
Accepted: 23 December, 2021;
Published: 27 December, 2021
Copyright: © 2021 Jargin SV. This is an open access article
distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction
in any medium, provided the original work is properly cited
Abstract
This case report is about spontaneous foreskin retraction but it is
relevant also to the status after circumcision. Non-therapeutic male
circumcision remains controversial; there is evidence in support of
its benefits; however, good hygiene may achieve some of the aims.
Late consequences are understudied, in particular, those related
to atrophy of the ageing genital skin and mucous membranes. A
superficial scald burn of the genital area occurred to a 3-years-old boy
in conditions of child neglect. Immediate medical help was not sought.
In the following years, symptoms of balanoposthitis were repeatedly
noticed. Along with the pubertal development, the foreskin became
completely and permanently retracted. There has never been any
strangulation or compression in terms of paraphimosis. The symptoms
started appearing at the age of about 58 years: recurring superficial
erosions in the frenular area, preputial rim and adjacent surfaces. The
penis binding with a soft cloth and occasional topical treatment is
necessary as atrophic skin is sensitive and vulnerable. Derangements of
blood supply may contribute to atrophic changes; therefore, vascular
diseases and diabetes mellitus must be included in the differential
diagnosis. Potential adverse effects discussed in this report emphasize
the fact that non-therapeutic neonatal circumcision is an invasive
procedure performed without patients’ consent.
Introduction
This case report is about spontaneous foreskin retraction but it is
relevant also to the status after circumcision. The aim of this report
was to draw attention to the understudied late consequences of the
permanent glans exposure and to call into question, once again,
the rationale behind the routine newborn circumcision. Neonatal
circumcision remains controversial, with rates varying over years.
There is evidence in support of its benefits [1,2]; but good hygiene may
also achieve some of the goals [3]. Male circumcision as a method of
HIV prevention, reportedly used in Africa with success [4], is beyond
the scope of this article. Some aspects of adult and newborn nontherapeutic
circumcision should be discussed separately. In adults,
the procedure is generally performed according to the principle of
informed consent. In the case of minors or newborns, this principle is
not observed, while the operation is justified by preventive purposes
or religious arguments [5]. The latter are not discussed here; it
should be only mentioned that obscurantists can influence broad
population strata diverting them from evidence-based medicine and
thus from their own and their children’s best interest. With regard to
prevention, the American Academy of Pediatrics (AAP) concluded
the following: “Existing scientific evidence demonstrates potential
medical benefits of newborn male circumcision; however, this data is
not sufficient to recommend routine newborn circumcision” [6]. The
AAP Committee on Bioethics stated that interventions that can safely
wait until the child can provide his own consent should be delayed
until that consent can be obtained [5].
Results of a recent meta-analysis indicated that overall risk of
complications requiring treatment after male circumcisions was
3.84% (95% confidence interval 3.35-4.37) [7]. According to some
authors, a lower frequency of complications is observed when
the procedure is performed on newborns; others believe that the
difference is caused by a better documentation of adverse events in
older patients. The complications include hemorrhages, infections,
adhesions and stenosis of the urethral meatus. In the absence of
anesthesia, the common adverse effect is pain, confirmed by changes
of the heartbeat and the newborn’s cry [5]. Neonatal circumcision
without clinical indications can be seen as invasive procedure with
a complication risk, performed without patients’ consent [8]. Since
preventive male circumcision leads to a permanent anatomical
alteration, some authors opine that it may be applied only in subjects
capable of giving consent [5]. The voluntariness in children should be
maximized by involving them as much as their age and understanding
would permit in the treatment planning [9]. Long-term consequences
of the glans exposure due to circumcision or permanent foreskin
retraction remain understudied, in particular, those related to atrophy
and vulnerability of the ageing genital skin and mucous membranes.
Case History
In the case of burns in children, child abuse and neglect should
be taken into consideration [10]. It has been estimated that up to
20% of burn injuries are the result of child abuse or neglect, with
highest incidence among children 0-4 years of age [11]. A superficial
scald burn of the genital area with hot soup occurred to a 3-yearsold
boy in conditions of child neglect[12]. Immediate medical help
was not sought. Subsequently, the fact of the burn was concealed
from medics. When the healing ensued, the child started scratching
the area. In the following years, symptoms of balanoposthitis were
repeatedly noticed. Along with the pubertal development, the foreskin
became completely and permanently retracted. There has never been
any strangulation or compression in terms of paraphimosis. The
symptoms started appearing at the age of about 58 years: recurrent
superficial erosions in the frenular area, preputial rim and adjacent
surfaces, occasional symptoms of distal urethritis. With a sexual
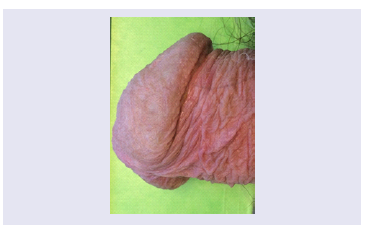
abstinence the condition comes to remission; but the penis binding with a soft cloth is necessary as thin atrophic skin is sensitive and
vulnerable (Figure 1). Ointments or vegetable oil are used to prevent
the sticking with the cloth in case of erosion or urethral discharge.
The topical treatment with Solcoseryl® or Actovegin® cream and seabuckthorn
oil [13] led to visible improvements
Discussion
The loss of double-layered prepuce exposes the glans and meatus
to direct abrasion and trauma [14] that may become noticeable in
conditions of age-related atrophy. Impairments of blood supply
can contribute to atrophic changes; therefore, vascular diseases and
diabetes mellitus must be included in the differential diagnosis in
such cases. Doppler ultrasonography is useful for the assessment
of vasculature [15]. A circulation derangement may be caused by
hernia and/or perineal descensus resulting e.g. from lifting of heavy
weights at a young age. Possible causes of the foreskin retraction
should be considered: lichen planus, squamous cell carcinoma and
premalignant lesions, other foreskin conditions as well as congenitally
underdeveloped prepuce (microposthia). Of note, comparable
gynecological conditions (atrophic vaginitis) are given more attention
in the literature, which can be seen as example of sexism in medicine.
Sexism and ageism in the healthcare are known topics [16]. Certain
ailments of ageing people are not given sufficient attention.
Conclusion
The glans exposure as a result of circumcision, permanent foreskin retraction or congenital microposthia may become symptomatic
along with progressive age-related atrophy and vulnerability of the
preputial and glans skin. Potential adverse effects discussed in this
report, as well as others, must draw attention to the fact that nontherapeutic
neonatal circumcision is an invasive procedure performed
without patients’ consent.