Journal of Clinical & Medical Case Reports
Download PDF
Case Report
A Rare Case of Massive Cerobrospinal Fluid Ascite: A Late Complication of Ventriculoperitoneal Shunt
N´da Hermann Adonis*, Drogba Kporou Landry, Konan Landry Melaine, Derou Keableon Louis and Varlet Guy
- 1Service de Neurochirurgie, CHU de Yopougon, Abidjan, Côte d’Ivoire
*Address for Correspondence: N´da Hermann Adonis, Service de Neurochirurgie CHU de Yopougon, 21 BP 632 Abidjan, Cote d´Ivoire, Tel: +22523537592; E-mail: drndah@yahoo.fr
Citation: N’da HA, Drogba KL, Konan LM, Derou KL, Varlet G, et al. A Rare Case of Massive Cerobrospinal Fluid Ascite: A Late Complication of Ventriculoperitoneal Shunt. J Clin Med Case Reports. 2017;4(2): 2.
Copyright © 2017 N´da Hermann A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Medical Case Reports | ISSN: 2332-4120 | Volume: 4, Issue: 2
Submission: 23 November, 2017 | Accepted: 20 December, 2017 | Published: 23 December, 2017
Abstract
Introduction: Cerebrospinal ascites is defined as an intraperitonealcollection of Cerebrospinal Fluid (CSF). This is a rare complication of Ventriculo-Peritoneal (VP) shunt. Underlying mechanisms and etiology are still unclear. Here, we reported a unique case and reviewed the literature for plausible mechanisms explaining its occurrence.
Case report: A 18 years old patient, with history of VP shunt 17 yearago, was admitted for an abdominal distention. The abdominal CT scan revealed a massive intraperitoneal collection. The biology analysis of the ascites sample evoked a CSF. The patient was successfully treated by Ventriculo-Atrial (VA) shunt followed by ascites drainage.
Conclusion: Although no consistent explanation emerged fromthe literature review, a failure in peritoneal resorption ability without any primitive peritoneal pathology seems to play a leading role to this rare complication.
Keywords
CSF ascites; Ventriculoperitoneal shunt; Hydrocephalus; Complications
Introduction
The peritoneal cavity was used for shunting the CSF initially by Kaush in 1908 [1]. Since then, VP shunt became the most prevailing technique for the treatment of hydrocephalus. It has the highest longterm success rate [2]. Although numerous abdominal complications have been reported after VP shunt, CSF ascites is an uncommon complication occurring few years after surgery [3]. Ascites is a peritoneal liquid collection commonly observed in hepatic and cardiac diseases such as carcinoma, cirrhosis and congestive heart failure. The appearance of CSF ascites raises the concern about the etiopathology.
We report a unique case of CSF massive ascites occurring 17 years after surgery. To the best of our knowledge, it is the farthest delayed complication of VP shunt. Hence, through a literature review, we aim to discuss the evoked mechanisms and the therapeutic options available for this condition.
Case Report
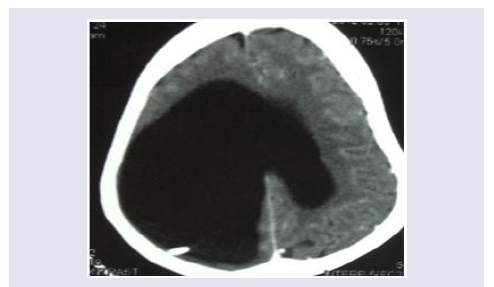
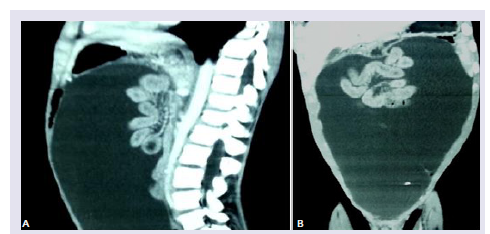
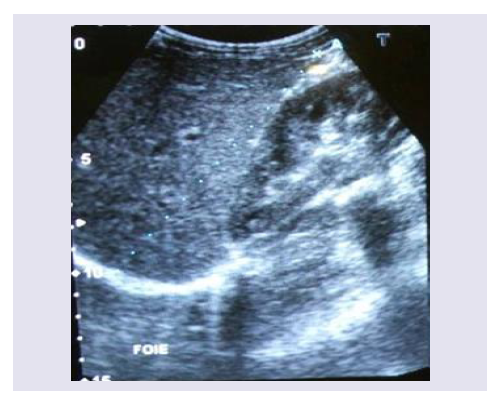
An 18 years old boy was admitted in our department for abdominal pain associated with an altered general status. The patient was a previous neurosurgical patient. Indeed, He was hospitalized at 1 year old age for a macrocephaly, left hemiparesis and convergent strabismus. The brain CT scan diagnosed a right univentricular hydrocephalus for which the patient subsequently underwent a VP shunt (Figure 1). The patient had a distal valve obstruction 10 months after surgery this first surgery which has been treated. The follow up was uneventful. Hence, 17 years later, he complained of painful abdominal distention. The physical examination revealed a poor general status, an umbilical diameter measuring 69cm; no abdominal mass was observed. Abdominal CT scan displayed a massive ascites with visceral compression (Figures 2A and 2B). The blood work and the oesophago-gastric endoscopy were uneventful therefore excluding hepatic condition. Brain CT scan exhibited the hydrocephalus suggesting a failure of the peritoneal resorption capacity. The ascitis sample was yellow pale and sterile. The patient was successfully treated by peritoneal drainage followed by a ventriculo-atrial shunt. Postoperative abdominal echography and the 3 months follow-up echography were normal (Figure 3). They were no abdominal distension 2 years after surgery.
Discussion
CSF ascites is a rare complication of VP shunt. Although unusual, the diagnostic is easy and therapeutic options are available. The main concern remains the physiopathology of this condition. In fact, CSF Ascitis seems resulted from multifactorial etiologies [4]. Four hypotheses emerge from the literature review: an overproduction of CSF, a protein increase in CSF, peritoneal infection and an immuneallergic disorder. Ray et al. evoked an overproduction when he reported a case of CSF ascitis resulting from plexus choroid papilloma [5]. However, this is not convincing since all cases of plexus choroid papilloma treated by VP shunts were not complicated CSF ascites. Next, Adegbite et al. claimed the hypothesis of idiopathic protein increase in CSF as the cause of CSF ascites [6]; yet this increase is generally observed in inflammatory processes such as peritoneal caricnosis, lymphatic drainage obstruction or peritoneal infection [7]. These were not present in our case. Several cases of CSF ascites have been reported but these were presented as pseudocysts or multiseptate collection peritoneal of CSF. Once again, not observed in our case. Dean et al. published a case of immune-allergic reactions after diphtheria and tetanus vaccine leading to CSF ascites [8].
Hence, although several hypotheses are evoked, those are not strong enough to explain all cases of CSF ascites. History of abdominal surgery may be a risk factor since this is found in several cases. In their report, Yukinaka et al. noticed CSF ascites occurring less than 2 years after surgery [9]. Our case is singular as the CSF ascites occurred 17 years later. Eosinophilic infiltration observed in peritoneal biopsy only is compatible with the presence of the shunt (foreign body) and cannot explain the resorption defect in patients [10].
In absence of previous peritoneal pathology, we suggest a progressive failure of peritoneal resorption ability due to prolonged presence of the shunt. Yet, researches are needed to confirm this hypothesis. If confirmed, long term carriers of VP shunt are at higher risk of developing CSF Ascites.
Conclusion
CSF ascites is a rare complication of VP shunt. We reported the first case to occur 17 years after of VP shunt insertion. The exact physiopathology remains to be elucidated. We suggest a progressive failure of the peritoneal resorption ability with valve aging. Hence, longtime carrier of VP shunt should be closely monitored for this complication.
References
- Chung JJ, Yu JS, Kim JH, Nam SJ, Kim JM (2009) Intra-abdominal complications secondary to ventriculoperitonealshunts: CT findings and review of the literature AJR 193: 1311-1317.
- Apparaci-Robles F, Molina-Fabrega R (2008) Abdominal cerebrospinal fluid pseudocyst: a complication of ventriculoperitoneal shunts in adults. J Med Imaging Radiat Oncol 52: 40-43.
- Popa F, Grigorean VT, Onose G, Popescu M, Strambu V, et al. (2009) Laparoscopic treatment of abdominal complications following ventriculoperitoneal shunt. J Med Life 2: 426-436.
- Yount RA, Glazier MC, Mealy J Jr, Kalsbeck JE (1984) Cerebrospinal fluid ascites complicating ventriculoperitoneal shunting: report of four cases. J Neurosurg 61: 180-183.
- Rays BS, Peck FC (1956) Papilloma of the choroid plexus of the lateral ventricles causing hydrocephalus in an infant. J Neurosurg 13: 317-322.
- Adegbite AB, Khan M (1982) Role of protein content in CSF ascite following ventriculoperitoneal shunting. J Neurosurg 57: 423-425.
- Ames RH (1967) Ventriculo-peritoneal shunts in the management of hydrocephalus. J Neurosurg 27: 525-529.
- Dean DF, Keller IB (1972) Cerebrospinal fluid ascites: a complication of ventriculoperitoneal shunt. J Neurol Neurosurg Psychiatry 35: 474-476.
- Yukinaka M, Nomura M, Mitani T, Kondo Y, Tabata T, et al. (1998) Cerebrospinal ascites developed 3 years after ventriculoperitoneal shunting in a hydrocephalic patient. Intern Med 37: 638-641.
- Chidambaram B, Balasubramaniam V (2000) CSF ascites: a rare complication of the ventriculoperitoneal shunts surgery. Neurol India 48: 378-380.