Journal of Clinical and Investigative Dermatology
Download PDF
Case Report
Verruca Plantaris with underlying Verrucous Carcinoma in a 63- year-old Filipino Male: A Case Report
Maan S. Gallardo*, Ron Michael P. Dagala and Andrea Marie Bernales-Mendoza
Department of Dermatology, Jose R. Reyes Memorial Medical Center, Philippines
*Address for Correspondence:Maan S. Gallardo, Department of Dermatology, Jose R. Reyes
Memorial Medical Center, Philippines. E-mail Id: gallardo.maan@gmail.com
Submission: 13 January, 2026
Accepted:27 January, 2026
Published: 29 January, 2026
Copyright: © 2026 Gallardo MS, et al. This is an open access
article distributed under the Creative Commons Attribution
License, which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is
properly cited.
Keywords: Carcinoma Cuniculatum; Dermatopathology; Foot
Neoplasm; Squamous Cell Carcinoma; Verrucous Carcinoma
Abstract
Background: Verrucous carcinoma is a rare, well-differentiated
variant of squamous cell carcinoma that most commonly arises on
acral and mucosal surfaces. Its indolent course and subtle histological
atypia often lead to diagnostic challenges.
Case Presentation: We report a 63-year-old Filipino male with a four-year history of a progressively enlarging verrucous plaque on the plantar surface of the left foot. Initial superficial biopsy revealed verruca plantaris, but a subsequent deep incisional biopsy confirmed verrucous carcinoma with underlying verruca plantaris. The patient underwent a wide local excision with histologically clear margins. Postoperative recovery was uneventful, and complete epithelialization was achieved, resulting in a satisfactory functional outcome.
Conclusions: This case highlights the diagnostic challenges of plantar verrucous carcinoma, which is often misdiagnosed as benign verruca vulgaris. Adequate deep tissue sampling and early surgical intervention are essential to prevent progressive local destruction and reduce the risk of amputation.
Case Presentation: We report a 63-year-old Filipino male with a four-year history of a progressively enlarging verrucous plaque on the plantar surface of the left foot. Initial superficial biopsy revealed verruca plantaris, but a subsequent deep incisional biopsy confirmed verrucous carcinoma with underlying verruca plantaris. The patient underwent a wide local excision with histologically clear margins. Postoperative recovery was uneventful, and complete epithelialization was achieved, resulting in a satisfactory functional outcome.
Conclusions: This case highlights the diagnostic challenges of plantar verrucous carcinoma, which is often misdiagnosed as benign verruca vulgaris. Adequate deep tissue sampling and early surgical intervention are essential to prevent progressive local destruction and reduce the risk of amputation.
Introduction
Verrucous carcinoma (VC) is an uncommon, well-differentiated
variant of squamous cell carcinoma characterized by a slow but locally
invasive growth pattern and minimal metastatic potential. It was first
described by Ackerman in 1948,[1] as a distinct clinicopathologic
entity and is now recognized to occur in various mucocutaneous
regions such as the oral cavity, anogenital area, and plantar surfaces.
[2] The plantar form, also referred to as epithelioma cuniculatum or
carcinoma cuniculatum, [3] presents a diagnostic challenge due to its
clinical resemblance to benign verrucous lesions like plantar warts or
chronic keratotic plaques. Misdiagnosis often results from superficial
biopsies that fail to capture the deep, endophytic component of the
lesion, leading to delays in definitive management and progressive
local destruction of surrounding soft tissue or bone.
Although cases of verrucous carcinoma arising on the foot are rarely reported globally and even less so in the Philippines, awareness of this entity remains essential among clinicians and dermatopathologists. Its indolent course, coupled with its potential for extensive local invasion, underscores the importance of early recognition and histopathologic confirmation through adequate tissue sampling. This case report aims to describe a rare presentation of plantar verrucous carcinoma arising in association with verruca plantaris in a Filipino patient, to emphasize the histopathologic pitfalls that contribute to diagnostic delay, and to highlight the value of prompt surgical management in achieving favorable functional and oncologic outcomes.
Although cases of verrucous carcinoma arising on the foot are rarely reported globally and even less so in the Philippines, awareness of this entity remains essential among clinicians and dermatopathologists. Its indolent course, coupled with its potential for extensive local invasion, underscores the importance of early recognition and histopathologic confirmation through adequate tissue sampling. This case report aims to describe a rare presentation of plantar verrucous carcinoma arising in association with verruca plantaris in a Filipino patient, to emphasize the histopathologic pitfalls that contribute to diagnostic delay, and to highlight the value of prompt surgical management in achieving favorable functional and oncologic outcomes.
Case Presentation
This is a case of a 63-year-old, Filipino male, who was seen at
the Department of Dermatology of Jose R. Reyes Memorial Medical
Center for an asymptomatic, oval fungating mass, approximately
2.5cm x 4.6cm x 1cm in size, that was hyperkeratotic and with areas
of ulceration, localized at the ball of the first digit of the left foot.
Four years prior to seeking consultation, the lesion appeared as a rough, hyperpigmented papule, with the patient reporting no history of manipulation or trauma. Over time, it progressed into a plaque, measuring 2 x 4 cm, causing mild discomfort while walking but without pain, itching, bleeding, or discharge. No medical consultations or treatments were sought at this point.
Three years later, the patient noticed the emergence of a protruding mass near the anus, measuring approximately 0.5 cm, which did not cause pain, bleeding, or discharge. Over time, this mass evolved into a cauliflower-like lesion, accompanied by sporadic episodes of bleeding and unintended weight loss. Several months later, the patient experienced rectal bleeding and sought medical attention at a tertiary hospital in Bulacan, where he received a diagnosis of Anal Adenocarcinoma and Synchronous Rectal Adenocarcinoma (T2N1bMx). Following this diagnosis, the patient was advised to transfer to a preferred hospital for debulking of the anal mass. Upon consultation at our institution, under the service of Medical Oncology, a plantar lesion was observed and subsequently biopsied, revealing Verruca plantaris. Following this, referral to the Department of Dermatology was made and an initial impression of verrucous squamous cell carcinoma was given.
Four years prior to seeking consultation, the lesion appeared as a rough, hyperpigmented papule, with the patient reporting no history of manipulation or trauma. Over time, it progressed into a plaque, measuring 2 x 4 cm, causing mild discomfort while walking but without pain, itching, bleeding, or discharge. No medical consultations or treatments were sought at this point.
Three years later, the patient noticed the emergence of a protruding mass near the anus, measuring approximately 0.5 cm, which did not cause pain, bleeding, or discharge. Over time, this mass evolved into a cauliflower-like lesion, accompanied by sporadic episodes of bleeding and unintended weight loss. Several months later, the patient experienced rectal bleeding and sought medical attention at a tertiary hospital in Bulacan, where he received a diagnosis of Anal Adenocarcinoma and Synchronous Rectal Adenocarcinoma (T2N1bMx). Following this diagnosis, the patient was advised to transfer to a preferred hospital for debulking of the anal mass. Upon consultation at our institution, under the service of Medical Oncology, a plantar lesion was observed and subsequently biopsied, revealing Verruca plantaris. Following this, referral to the Department of Dermatology was made and an initial impression of verrucous squamous cell carcinoma was given.
The patient has a medical history of Hypertension stage II and Type
2 Diabetes mellitus, both of which are well-managed with prescribed
medications. Presently, the patient is undergoing chemotherapy every
three weeks for tumor debulking. Previous surgical interventions
include hernia repair in 2013 and colostomy in 2023, both of which
were uneventful. There is a family history of hypertension and diabetes
mellitus, but no reported history of cancer among relatives. The
patient does not smoke, occasionally consumes alcohol, and denied
any illicit drug use. Dietary preferences include a preference for red
meat and infrequent consumption of fruits and vegetables. He earned
a high school degree. The patient began working as a fish porter at the
age of 16 and later held a position as a laundry utility man in Saudi
Arabia from 1991 to 2000. After returning home, he worked as a
driver until retiring in 2020 and has since chosen to stay home. The
patient frequently wears slippers and is regularly exposed to sunlight,
particularly in the morning between 8 AM and 2 PM, while working
as a driver, often with inadequate sun protection. There is no known
exposure to arsenic, cutting oils, polycyclic aromatic hydrocarbons,
or ionizing radiation. The patient has been sexually active with only
one partner and had no history of sexually transmitted diseases.
During the past year, the patient experienced a significant weight loss
of 21%.
Cutaneous examination revealed a solitary, well-defined,
oval-shaped plaque, measuring 2.5 x 4.6 x 1 cm, with a verrucous,
hyperpigmented, cauliflower-like appearance and ulcerated areas
located on the medial plantar aspect of the first digit of the left foot.
[Figure 1]. Additionally, an enlarged left inguinal lymph node,
measuring 1.5x1 cm in diameter, was palpated. The lymph node
exhibited no tenderness, was firm to the touch, and had normal
overlying skin. Hair, nail, mucosal, and other systemic examinations
yielded no notable findings.
The MRI of the left foot was done and revealed several findings
namely:
(i) Subchondral cysts, cartilage thinning, and joint space narrowing in the 1st metatarsophalangeal joint,
(ii) Crosion in the medial margin of the head of the 1st metatarsal bone, and
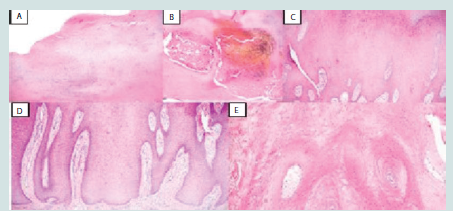
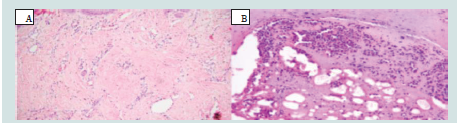
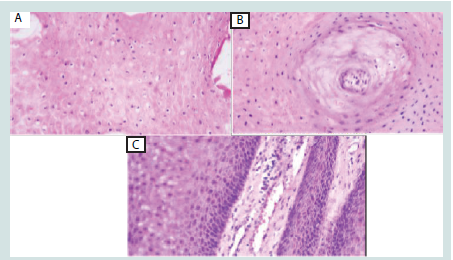
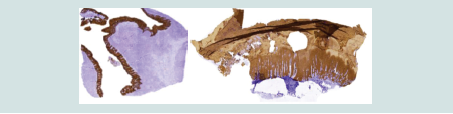
(iii) Formation of a bone spur in the lateral aspect of the base of the 1st proximal phalanx. Abdominal and chest computed tomography scans revealed normal findings. Laboratory tests indicated decreased levels of hemoglobin, hematocrit, and red blood cells, along with elevated levels of carcinoembryonic antigen (CEA). Incisional biopsy of the tumor was done revealing histopathologic findings indicative of verruca plantaris with underlying verrucous carcinoma. (Figures 2-5). Pancytokeratin stained positive (Figure 6). Periodic acid Schiff stain is negative for fungal elements.
A wide local excision was performed without any postoperative complications, and the patient’s recovery proceeded smoothly. To support optimal wound healing, the patient was prescribed a
(i) Subchondral cysts, cartilage thinning, and joint space narrowing in the 1st metatarsophalangeal joint,
(ii) Crosion in the medial margin of the head of the 1st metatarsal bone, and
(iii) Formation of a bone spur in the lateral aspect of the base of the 1st proximal phalanx. Abdominal and chest computed tomography scans revealed normal findings. Laboratory tests indicated decreased levels of hemoglobin, hematocrit, and red blood cells, along with elevated levels of carcinoembryonic antigen (CEA). Incisional biopsy of the tumor was done revealing histopathologic findings indicative of verruca plantaris with underlying verrucous carcinoma. (Figures 2-5). Pancytokeratin stained positive (Figure 6). Periodic acid Schiff stain is negative for fungal elements.
A wide local excision was performed without any postoperative complications, and the patient’s recovery proceeded smoothly. To support optimal wound healing, the patient was prescribed a
Figure 1: Solitary, well-defined, oval-shaped, verrucous, cauliflower-like,
hyperpigmented plaque with ulcerated areas, measuring 2.5 x 4.6 x 1 cm, on
the medial plantar aspect of the first digit of the left foot.
Figure 3: H&E staining (10x) showing (A) thick orthokeratosis, parakeratosis,
(B) hemorrhages, (C) large polygonal squamous cells with abundant pink
cytoplasm, (D) deep bulbous process, and (E) pushing border.
Figure 5:H&E staining (40x) showing (A) numerous koilocytic cells, (B)
whorled dyskeratotic and atypical keratinocytes, and (C) infiltration of
lymphocytes and blood vessels oriented perpendicular to the surface
Figure 7: Granulation tissue formation was observed along the wound edges,
accompanied by a reduction in the size of the ulcerated area, without any
discernible functional impairment. Clinical photos represent the lesion (A)
2 weeks, (B) 4 weeks, (C) 8 weeks and, (D) 12 weeks after the operation,
respectively.
daily regimen of Vitamin C + Zinc capsules, which serve to bolster
collagen synthesis and immune function. In addition, the patient
was instructed to apply Tretinoin 0.05% cream once daily to the
wound edges, thereby promoting enhanced epithelial regeneration
and tissue remodeling. An adjunctive measure involved applying
Oxytetracycline ointment via sandwich dressing twice daily,
providing both antimicrobial coverage and a protective barrier to
further facilitate wound repair. Continuous monitoring and periodic
follow-up assessments demonstrated favorable healing progress,
as evidenced by the formation of granulation tissue at the wound
margins and a corresponding reduction in the ulcerated area [Figure 7]. Throughout this period, no functional impairment was reported. The therapeutic approach, combining systemic supplementation
with targeted topical treatments, was instrumental in promoting a
successful clinical outcome.
Discussion
Cutaneous squamous cell carcinoma (cSCC) is estimated to be
the second most common type of skin cancer in immunocompetent
individuals and the most common type in immunocompromised
populations. It accounts for about 20% of nonmelanoma skin
cancers. [7,8] In a study by Kim et al., the yearly incidence rates of
cSCC among Chinese, Malays, and Asian Indians were 2.6, 1.3, and
1.4 per 100,000 individuals, respectively.[7] In the local context, skin
cancers represent around 1% of all diagnosed cancers documented
in the Philippine Cancer Registry. Villanueva et al. found that the
head and neck region emerged as the primary site for malignant skin
tumors.[9]
Verrucous carcinoma (VC), commonly referred to as Ackerman tumor, is typically observed in regions such as the oral cavity and anogenital area. Its occurrence in the foot is relatively rare, presenting unique challenges in diagnosis and management compared to the more typical sites [1,2]. VC of the foot, also termed carcinoma cuniculatum (CC) [3,4] is an uncommon, low-grade variant of squamous cell carcinoma characterized by locally aggressive clinical behavior and low metastatic potential. It was first described in the English-language medical literature by Aird et al. in 1954. CC primarily affects men in their 4th to 6th decade of life and is most frequently observed on the sole, especially the ball of the foot. [5,15] The lesion often follows a chronic course, evolving from a discrete focal lesion to a large fungating mass that deeply invades underlying tissues, often complicated by secondary infection. Many tumors have initially been mistaken for recalcitrant warts or corns, contributing to treatment delays [5,18].
Verrucous carcinoma (VC), commonly referred to as Ackerman tumor, is typically observed in regions such as the oral cavity and anogenital area. Its occurrence in the foot is relatively rare, presenting unique challenges in diagnosis and management compared to the more typical sites [1,2]. VC of the foot, also termed carcinoma cuniculatum (CC) [3,4] is an uncommon, low-grade variant of squamous cell carcinoma characterized by locally aggressive clinical behavior and low metastatic potential. It was first described in the English-language medical literature by Aird et al. in 1954. CC primarily affects men in their 4th to 6th decade of life and is most frequently observed on the sole, especially the ball of the foot. [5,15] The lesion often follows a chronic course, evolving from a discrete focal lesion to a large fungating mass that deeply invades underlying tissues, often complicated by secondary infection. Many tumors have initially been mistaken for recalcitrant warts or corns, contributing to treatment delays [5,18].
Globally, the incidence of carcinoma cuniculatum is unknown,
with only a limited number of cases reported. In the Philippines, one
study by Cubillan et al. described a case of VC of the foot arising
from a muscle flap and skin graft site in a 74-year-old Filipino female.
[6] Other local reports focus on verrucous carcinomas involving the
oral and anogenital areas. Although verrucous carcinoma is well described,
reports of plantar lesions with co-existing verruca plantaris
in Filipino patients remain scarce.
The pathogenesis of carcinoma cuniculatum remains unclear. Several potential contributors have been proposed, including abnormal expression of the p53 tumor suppressor protein, human papillomavirus (particularly subtypes 11, 16, 18, and 33), chronic inflammation, repeated trauma or pressure on weight-bearing areas, poor local hygiene, tobacco use, and chemical carcinogen exposure. [10,11,12] In darker skin phenotypes, cSCC often arises in sunprotected areas, suggesting ultraviolet radiation may have a lesser role in tumor induction. [12]
Clinically, CC may present as a bulky, exophytic lesion with ulceration and sinus tract formation, from which foul-smelling purulent keratinous material may discharge. Histological confirmation is essential. Biopsies must include deep dermis and subcutaneous tissue, as superficial samples may be insufficient. Hallmark features include exophytic and endophytic growth patterns with well-differentiated keratinocytes, pronounced hyperkeratosis, and papillomatosis. [13,14] In the study by Ray et al., CC was reported to arise from a wart on the heel; histologic sections revealed koilocytosis, as observed in our case. [13]
Imaging is recommended to assess bony involvement. CT scans are preferred for evaluating bone infiltration, while MRI provides detailed assessment of tumor size and depth. [6,14]
Currently, wide local excision is the treatment of choice for VC due to its tendency to distort adjacent tissues, which makes intraoperative margin determination difficult. However, this approach is associated with recurrence rates as high as 19-75%.15 Mohs micrographic surgery is gaining popularity as it allows margin control and may reduce recurrence, though further evidence is needed to establish its definitive role.16 In advanced cases, amputation may be warranted, especially in the context of poor vascular status, recurrent tumors, or extensive tissue involvement.
Post-excision defects may be reconstructed using full-thickness skin grafts or free flaps. Adjunctive treatments such as topical chemotherapy, cryotherapy, electrocautery, and laser therapy have been attempted but are associated with high recurrence rates. Radiotherapy is not typically recommended due to the potential for malignant transformation. [2,15]
A recent study by Prince et al. found that tumors on nonglabrous areas of the foot (e.g., dorsal surfaces and great toe) had a higher recurrence rate than those on plantar surfaces, despite negative surgical margins.[17] Recurrences typically appeared within months, often in areas of highest tissue stress, including graft sites.
VC generally has a favorable prognosis, with cure rates reported as high as 99% when treated promptly and adequately. [5,18] Nonetheless, long-term surveillance remains essential to monitor for recurrence and rare metastatic progression.
The pathogenesis of carcinoma cuniculatum remains unclear. Several potential contributors have been proposed, including abnormal expression of the p53 tumor suppressor protein, human papillomavirus (particularly subtypes 11, 16, 18, and 33), chronic inflammation, repeated trauma or pressure on weight-bearing areas, poor local hygiene, tobacco use, and chemical carcinogen exposure. [10,11,12] In darker skin phenotypes, cSCC often arises in sunprotected areas, suggesting ultraviolet radiation may have a lesser role in tumor induction. [12]
Clinically, CC may present as a bulky, exophytic lesion with ulceration and sinus tract formation, from which foul-smelling purulent keratinous material may discharge. Histological confirmation is essential. Biopsies must include deep dermis and subcutaneous tissue, as superficial samples may be insufficient. Hallmark features include exophytic and endophytic growth patterns with well-differentiated keratinocytes, pronounced hyperkeratosis, and papillomatosis. [13,14] In the study by Ray et al., CC was reported to arise from a wart on the heel; histologic sections revealed koilocytosis, as observed in our case. [13]
Imaging is recommended to assess bony involvement. CT scans are preferred for evaluating bone infiltration, while MRI provides detailed assessment of tumor size and depth. [6,14]
Currently, wide local excision is the treatment of choice for VC due to its tendency to distort adjacent tissues, which makes intraoperative margin determination difficult. However, this approach is associated with recurrence rates as high as 19-75%.15 Mohs micrographic surgery is gaining popularity as it allows margin control and may reduce recurrence, though further evidence is needed to establish its definitive role.16 In advanced cases, amputation may be warranted, especially in the context of poor vascular status, recurrent tumors, or extensive tissue involvement.
Post-excision defects may be reconstructed using full-thickness skin grafts or free flaps. Adjunctive treatments such as topical chemotherapy, cryotherapy, electrocautery, and laser therapy have been attempted but are associated with high recurrence rates. Radiotherapy is not typically recommended due to the potential for malignant transformation. [2,15]
A recent study by Prince et al. found that tumors on nonglabrous areas of the foot (e.g., dorsal surfaces and great toe) had a higher recurrence rate than those on plantar surfaces, despite negative surgical margins.[17] Recurrences typically appeared within months, often in areas of highest tissue stress, including graft sites.
VC generally has a favorable prognosis, with cure rates reported as high as 99% when treated promptly and adequately. [5,18] Nonetheless, long-term surveillance remains essential to monitor for recurrence and rare metastatic progression.
Conclusion
Diagnosing verrucous carcinoma (VC) can be particularly
challenging due to its varied clinical presentations, as individual
patients often exhibit distinct findings. In the present case, although
certain hallmark features were noted, others were less apparent.
Furthermore, plantar VC is notably rare, especially among Filipino
patients, which adds complexity to timely diagnosis. Superficial
biopsies of a highly proliferative neoplasm frequently led to
misdiagnosis underscoring the importance of obtaining specimens
that include the deep dermis and subcutaneous fat to capture
the lesion’s full architectural profile. Maintaining a high index of
suspicion, both clinically and histologically, is essential for prompt
recognition and appropriate management, as delayed intervention
may permit progressive local invasion. Finally, given the elevated risk
of recurrence associated with VC, vigilant follow-up and routine
evaluations are recommended until complete healing is confirmed.
Disclosures:
All authors declared no conflicts of interest.Availability of Data & Materials:
Data supporting this study are available from the corresponding
author upon reasonable request.Ethical Considerations:
The research involved no more than minimal risk and used
only the medical data of the patient. Secured data collection was
implemented, involving only the researcher and the Medical Records
staff responsible for patient records. Only necessary information
such as diagnosis, ICD-10 codes used, family history, and treatment
outcome were collected. No other identifying personal information
was recorded throughout the study. A non-disclosure agreement was
established, and only redacted data was recorded. This study protocol
was reviewed and approved by the Institutional Review Board of Jose
R. Reyes Memorial Medical Center (Protocol No. 2024-157).Informed Consent:
Written informed consent was obtained from the patient for this
case report and accompanying clinical images.