Journal of Clinical and Investigative Dermatology
Download PDF
Research Article
Expert Perspectives on Clinical Practices and Treatment Preferences for Azelaic Acid and Combination Therapy in Various Dermatological Conditions in the Indian Setting
Manjula S* and Krishna Kumar M
Department of Medical Services, Micro Labs Limited, Bangalore, Karnataka, India
*Address for Correspondence:Dr Manjula S, Department of Medical Services, Micro Labs Limited,
Bangalore. Telephone no: (080) 22370451 E-mail Id: drmanjulas@gmail.com
Submission:13 November, 2025
Accepted: 08 December, 2025
Published:10 December, 2025
Copyright: © 2025 Manjula S, et al. This is an open access article
distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Keywords: Azelaic Acid; Glycolic Acid; Acne Vulgaris; Melasma; Post-
Inflammatory Hyperpigmentation; Combination Therapy
Abstract
Objective:To assess clinicians’ perspectives on the management
of melasma, acne vulgaris, and post-inflammatory hyperpigmentation
(PIH) in Indian settings, with a focus on the use of azelaic acid and its
combination with glycolic acid in various dermatological conditions.
Methods:This cross-sectional study was conducted using a 23- item questionnaire to gather perspectives from dermatologists across Indian settings. The survey focused on clinical experiences, physician preferences, and observations regarding the use of both monotherapy and combination therapy in managing pigmentary disorders and acne. Responses were analyzed using descriptive statistical methods.
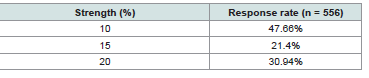
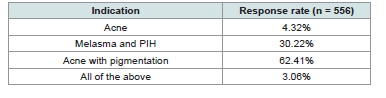
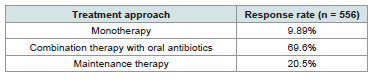
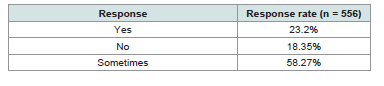
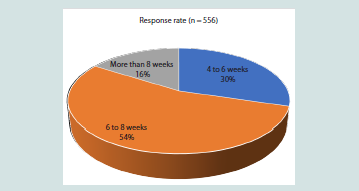
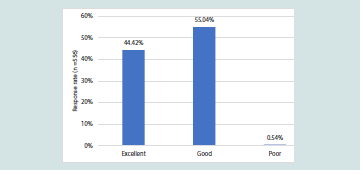
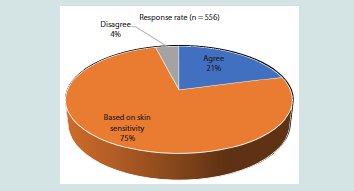
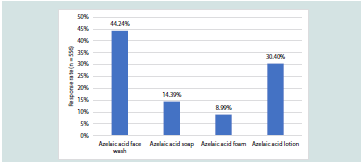
Results:Among the 556 participants, approximately 48% indicated that a 10% concentration of azelaic acid is most commonly recommended in routine clinical practice. Around 62% of clinicians reported that acne associated with pigmentation is the primary indication for azelaic acid use. More than half (54.32%) of respondents recommended an optimal treatment duration of 6-8 weeks when using a combination of azelaic acid and glycolic acid for acne management. Nearly 55% rated the azelaic acid + glycolic acid combination as effective for treating post-acne pigmentation. A majority (70%) favored combining azelaic acid with oral antibiotics for mild to moderate papulopustular acne. About 58% noted that azelaic acid + glycolic acid therapy occasionally required the use of a moisturizer. Most respondents (75.18%) emphasized that dose escalation of azelaic acid in acne management should depend on individual skin sensitivity. Additionally, around 44% reported that, among newer formulations, azelaic acid face wash was the most recommended option.
Conclusion:This study highlights that dermatologists commonly prefer 10% azelaic acid cream for acne with pigmentation. A combination of azelaic acid and glycolic acid used for 6-8 weeks has shown excellent perceived efficacy in improving post-acne hyperpigmentation. Treatment decisions based on an individual’s skin sensitivity, with face wash formulations, gained popularity, and short term contact therapy was recommended initially.
Methods:This cross-sectional study was conducted using a 23- item questionnaire to gather perspectives from dermatologists across Indian settings. The survey focused on clinical experiences, physician preferences, and observations regarding the use of both monotherapy and combination therapy in managing pigmentary disorders and acne. Responses were analyzed using descriptive statistical methods.
Results:Among the 556 participants, approximately 48% indicated that a 10% concentration of azelaic acid is most commonly recommended in routine clinical practice. Around 62% of clinicians reported that acne associated with pigmentation is the primary indication for azelaic acid use. More than half (54.32%) of respondents recommended an optimal treatment duration of 6-8 weeks when using a combination of azelaic acid and glycolic acid for acne management. Nearly 55% rated the azelaic acid + glycolic acid combination as effective for treating post-acne pigmentation. A majority (70%) favored combining azelaic acid with oral antibiotics for mild to moderate papulopustular acne. About 58% noted that azelaic acid + glycolic acid therapy occasionally required the use of a moisturizer. Most respondents (75.18%) emphasized that dose escalation of azelaic acid in acne management should depend on individual skin sensitivity. Additionally, around 44% reported that, among newer formulations, azelaic acid face wash was the most recommended option.
Conclusion:This study highlights that dermatologists commonly prefer 10% azelaic acid cream for acne with pigmentation. A combination of azelaic acid and glycolic acid used for 6-8 weeks has shown excellent perceived efficacy in improving post-acne hyperpigmentation. Treatment decisions based on an individual’s skin sensitivity, with face wash formulations, gained popularity, and short term contact therapy was recommended initially.
Introduction
Disorders of pigmentation and follicular inflammation represent
a significant dermatological burden, contributing to substantial
psychosocial distress and a reduced quality of life across diverse
populations.[1-4] Acne vulgaris affects approximately 9.4% of the
global population, making it one of the most prevalent dermatological
conditions.[5] A meta-analysis reported a global prevalence of 0.99%
(95% CI: 0.67–1.46%) for hidradenitis suppurativa.[6] The prevalence
of melasma and other pigmentary disorders varies widely across
regions, ranging from about 1% in the general population to as high
as 40% in high-risk groups, depending on factors such as skin type,
ultraviolet exposure, and geographic location. [6]
In India, a multicentric study across four regions reported
melasma in 331 patients with a mean age of approximately 37 years
and a female-to-male ratio of 4:1. [6] Among Indian adults (>25 years),
a large hospital-based study observed acne vulgaris in 0.74% of 24,056
patients. [7] Furthermore, post-inflammatory hyperpigmentation
(PIH) is common in Indian populations, with over 70% of individuals
younger than 35 years with a history of acne exhibiting residual
pigmented lesions. [8] Melasma, PIH, and acne-related pigmentation
are particularly prevalent in individuals with darker skin types, which
constitute a substantial proportion of the Indian population. [8,9]
The management of these conditions requires careful consideration
of efficacy, safety, and tolerability, particularly given the propensity
for PIH following inflammatory skin conditions in this demographic.
Azelaic acid emerges as a promising, versatile treatment for
pigmentary disorders and acne in the Indian population, with a
significant number of studies and expert consensus. The drug exerts
its antibacterial activity by inhibiting cellular protein synthesis in
both aerobic and anaerobic bacteria, particularly Staphylococcus
epidermidis and Propionibacterium acnes. In aerobic organisms, it
reversibly inhibits several oxidoreductive enzymes such as tyrosinase,
mitochondrial respiratory chain enzymes, thioredoxin reductase,
5-α-reductase, and DNA polymerases. In anaerobic bacteria, it
disrupts glycolysis. Additionally, azelaic acid improves acne vulgaris
by normalizing keratinization and reducing microcomedo formation.
[10].
The mechanism of action of glycolic acid involves targeted disruption of desmosomal (corneosomal) bonds in the outer stratum corneum, leading to reduced cohesion between corneocytes and enhanced exfoliation. This promotes controlled desquamation of the stratum disjunctum without compromising the integrity or barrier function of the skin.[11] Azelaic acid and glycolic acid together improve acne and hyperpigmentation by enhancing skin renewal, reducing bacterial load, and evening skin tone. [12-14]
The mechanism of action of glycolic acid involves targeted disruption of desmosomal (corneosomal) bonds in the outer stratum corneum, leading to reduced cohesion between corneocytes and enhanced exfoliation. This promotes controlled desquamation of the stratum disjunctum without compromising the integrity or barrier function of the skin.[11] Azelaic acid and glycolic acid together improve acne and hyperpigmentation by enhancing skin renewal, reducing bacterial load, and evening skin tone. [12-14]
This study aimed to gather the clinicians’ experiences and
preferences regarding azelaic acid monotherapy and combination
therapy, which may provide insights into current clinical practices
and help inform future treatment strategies for pigmentary disorders
and acne management.
Methodology
Study Settings:
A cross-sectional study was carried out among dermatologists
involved in the management of a wide range of dermatological
conditions in the major Indian cities from June 2024 to December
2024. The study was conducted after getting approval from Bangalore
Ethics, an Independent Ethics Committee, which was recognized by
the Indian Regulatory Authority, the Drug Controller General of
India.Study participants:
An invitation was sent to leading dermatologists in managing
a wide range of dermatological conditions in the month of March
2024 for participation in this Indian survey. About 556 clinicians
from major cities of all Indian states, representing the geographical
distribution, shared their willingness to participate and provide
necessary data.Study Procedure:
The questionnaire booklet titled AGILE study was sent to the
clinicians who were interested in participating in the survey. The
study questionnaire comprised 23 questions that assessed key
aspects, including clinical practices, treatment preferences, and the
use of azelaic acid and its combination with glycolic acid for various
dermatological conditions. Reliability, as determined by a split-half
test (coefficient alpha), was adequate but should be improved in
future versions of the questionnaire. A study of criterion validity
was undertaken to test the questionnaire and to develop methods of
testing the validity of measures of Physicians’ Perspectives. However,
the extraneous variables in this include the clinician’s experience,
usage of the newer drugs, etc. The two criteria used were the doctors’
perspectives from the clinical practice and the assessment of an
external assessor and statistician. Clinicians had the option to skip
questions as desired and were instructed to complete the survey
independently, without peer consultation. Before participating in the
survey, all respondents provided written informed consent.Statistical analysis:
Data were analyzed using descriptive statistics, with categorical
variables summarized as frequencies and percentages. To visualize
the distribution of the categorical variables, pie charts and bar
charts were created using Microsoft Excel 2013 (version 2409, build
16.0.18025.20030).Results
Out of 556 participants, 52% of the respondents indicated that
11-25 patients with melasma are treated monthly in their clinical
practice. About 44% of respondents reported that 26-50 patients
are treated with acne vulgaris monthly in clinical practice. Similarly,
about 46% of the participants reported that 11-20 patients are treated
for PIH in clinical practice monthly. About 48% of the participants
reported that a 10% strength of azelaic acid is mostly preferred in day to-
day practice [Table 1].
The majority (60.97%) of participants indicated cream as their
preferred azelaic acid formulation used in routine practice. About
62% reported that acne with pigmentation is the preferred indication
for azelaic acid use [Table 2]. More than half (63.85%) stated that
they would sometimes consider recommending azelaic acid as part
of a combination therapy. Approximately half (49.82%) indicated
a preference for using the azelaic acid + glycolic acid combination
in 26–50% of their patients. According to 54% of participants, the
optimal treatment duration for this combination in acne management
is 6 to 8 weeks [Figure 1], and 49% recommended the same duration
for hyperpigmentation treatment.
The majority (62.95%) reported that they would sometimes
recommend azelaic acid + glycolic acid for truncal acne treatment.
About 55% of participants rated this combination as good for postacne
pigmentation [Figure 2], and around 70% favored azelaic acid
combination therapy with oral antibiotics for mild to moderate
papulopustular acne [Table 3]. Nearly half (49.82%) indicated that
they would sometimes recommend azelaic acid with oral minocycline
or doxycycline in the management of hidradenitis suppurativa.
Around 56% of respondents reported that patients should sometimes
be advised on how to use azelaic acid + glycolic acid. About 58%
indicated that azelaic acid + glycolic acid therapy sometimes required
the use of a moisturizer [Table 4].
Table 1:Distribution of responses on the most preferred strength of azelaic acid
in day-to-day practice
Table 3:Distribution of responses on the recommendation of azelaic acid in mild
to moderate papulopustular acne
Table 4:Distribution of responses on the requirement for moisturiser use during
azelaic acid + glycolic acid therapy
Figure 1:Distribution of response on recommendation for optimal duration of
azelaic acid + glycolic acid therapy in acne.
Figure 2:Distribution of responses on opinion regarding azelaic acid +
glycolic acid in post-acne pigmentation
Figure 3:Distribution of responses on agreement with the recommendation
of dose escalation of azelaic acid in the management of acne
More than half (53.6%) of the experts reported that they would
sometimes recommend topical azelaic acid + glycolic acid for the
treatment of keratosis pilaris. However, for lentigo maligna, 53% of
participants indicated that they would not recommend the topical
azelaic acid + glycolic acid combination. Approximately 53% reported
that azelaic acid + glycolic acid prescriptions were sometimes altered
by seasonal changes or geographical location. The majority (75.18%)
emphasized that azelaic acid dose escalation in acne management
should be based on skin sensitivity [Figure 3].
Nearly 44% of respondents reported that, among new
formulations, azelaic acid face wash was the most recommended
option [Figure 4]. A substantial majority (67.09%) of participants
advised patients to use short-term contact treatment when applying
azelaic acid + glycolic acid for the first time. Based on clinical
experience, 48% of respondents reported that only 11–20% of patients
with hyperpigmentation completed the prescribed course of therapy.
Discussion
The predominant use of 10% azelaic acid cream suggests that it
is well-tolerated and effective for routine dermatological practice,
making it a suitable first-line formulation for acne and pigmentation
disorders. In addition, the azelaic acid face wash was identified
as a promising new formulation, reflecting a shift toward more
convenient, cosmetically acceptable, and better-tolerated options
that may enhance patient adherence. Evidence from clinical studies
supports these observations. Ivona Tomić et al. compared the efficacy
of a 10% azelaic acid nanocrystal hydrogel with a 20% azelaic acid
cream for acne treatment and found a treatment success rate of
36.51% for the 10% nanocrystal hydrogel, compared to 30.37% for
the 20% cream. [15] Similarly, Anil Kumar et al. reported that most
commercially available topical formulations contain azelaic acid
concentrations ranging between 15% and 20%, indicating variability
in practice but growing recognition of lower concentrations as
effective and well-tolerated options.[16] In a previous study, it was
observed that the azelaic acid face wash formulation was commonly
preferred by dermatologists (48% of respondents) for the treatment
of mild-to-moderate papulopustular acne.
[17]
The preference for azelaic acid in acne with pigmentation
underscores its unique advantage in targeting both inflammatory
lesions and PIH, making it particularly valuable for patients with
darker skin types who are more prone to PIH. Supporting evidence
from Heather Woolery-Lloyd et al. demonstrates that azelaic
acid exhibits anti-tyrosinase activity, reduces inflammation, and
effectively manages both acne lesions and residual pigmentation.
[18] Furthermore, in a previous survey conducted by the current
authors, approximately 37% of experts recommended a 20%
daily concentration as optimal for managing acne and associated
pigmentation disorders.[19] Similarly, Archana Rede et al. reported
favorable outcomes with this combination, particularly among
individuals with darker skin, showing a significant reduction in
inflammatory lesions.[20] According to Kircik et al., azelaic acid
inhibits melanocyte activity and reduces hyperpigmentation, while
glycolic acid complements this action by promoting exfoliation and
enhancing skin renewal.[21]
In this study, a consensus that around a 6-8-week treatment
duration and the use of short-contact therapy during initiation
highlight the importance of balancing therapeutic benefit with
cutaneous tolerability. In line with these findings, a previous survey
involving 467 dermatologists reported that 56% recommended
a 6-8-week regimen, and 66% preferred the azelaic acid–glycolic
acid combination for acne therapy.[19] Similarly, Spellman et al.
reported in a 12-week clinical study that this combination led to a
significantly greater reduction in inflammatory lesions compared to
other treatment options. [12]
Approximately 70% of dermatologists supported combining
azelaic acid with oral antibiotics for managing mild-to-moderate
papulopustular acne, reflecting its established role within multimodal
therapeutic regimens. Evidence from Pazoki-Toroudi et al.
demonstrated that a formulation containing 5% azelaic acid and 2%
erythromycin led to a significant reduction in papules, pustules, and
comedones compared with monotherapy.[22] Similarly, Gollnick et
al. demonstrated that combining 20% azelaic acid cream with oral
minocycline resulted in an 88% reduction in papules and pustules
and complete resolution of deep inflammatory lesions.[23] Further
evidence from Pazoki-Toroudi et al. confirmed enhanced therapeutic
outcomes when azelaic acid was combined with clindamycin.
[24]
Many participants noted that the use of azelaic acid and glycolic
acid combinations often required the concurrent use of a moisturizer
to minimize irritation, and the majority emphasized that dose
escalation of azelaic acid in acne management should be guided by
individual skin sensitivity. Supporting evidence aligns with these
observations. Guevara et al. reported that in a melasma study, 53%
of patients required a moisturizer after eight weeks of treatment with
a glycolic acid–based cream.[25] Similarly, Kakita et al. observed that
patients using azelaic acid and glycolic acid combinations experienced
slightly higher incidences of peeling, burning, stinging, and dryness
compared to other therapies.[13] Rosso et al. further emphasized
that moisturizers help alleviate these side effects and support skin
barrier maintenance.[26] Moreover, the Guidelines of Care for the
Management of Acne Vulgaris by Reynolds et al. emphasized that
azelaic acid is particularly suitable for individuals with sensitive skin,
underscoring the need for flexible dosing and adjustments based on
local irritation and formulation tolerability.[26]
The key strength of this study is its large sample size of 556
dermatologists, providing a comprehensive overview of clinical
preferences and perceived efficacy for azelaic acid and its combinations.
It offers valuable insights into formulation choices, dosage preferences,
and treatment practices across various dermatological conditions.
The inclusion of comparative and literature-based evidence further
enhances its clinical relevance. However, the study’s limitations
include reliance on self-reported data, which may introduce response
bias, and the absence of patient-level clinical outcomes. Additionally,
the survey did not account for regional variations or long-term
efficacy and safety data of the evaluated formulations.
Conclusion
This survey highlights current trends in managing pigmentary
disorders and acne in India. Dermatologists predominantly use
10% azelaic acid cream, especially for acne with pigmentation.
The azelaic acid + glycolic acid combination, used for 6-8 weeks,
has shown excellent perceived efficacy in improving post-acne
hyperpigmentation. Combination therapy with oral antibiotics is
preferred for mild-to-moderate papulopustular acne. Dose escalation
and moisturizer use are individualized based on skin sensitivity.
Face wash formulations gain increasing acceptance, and short contact
therapy is commonly advised for first-time users to improve
tolerability.
Acknowledgement
We would like to thank all the Dermatologists who participated
in this study.
Conflict of interest:
None declared