Journal of Clinical and Investigative Dermatology
Download PDF
A complete cutaneous examination was done. A painless, nonpruritic, 3.5 x 3.5 cm nodule with a surrounding hyperpigmented patch was observed in the middle metatarsal of the left plantar foot. Incision biopsy was performed.
Microscopic evaluation of the tissue specimen showed a hyperplastic epidermis and presence of nests of atypical melanocytes along the dermo-epidermal junction extending to the stratum corneum signifying a pagetoid spread. HMB staining was positive. Correlation between the clinical presentation and the pathology findings established the diagnosis of acral nodular melanoma. The patient was referred to Orthopedic Surgery and a below-the-knee amputation was done. Cranial, chest and pelvic CT scan revealed no metastasis. There has been no recurrence of the mass after two months of follow-up.
History of trauma was noted resulting in erosion and light bleeding on the nodule which progressed to a painful ulceration.
A complete cutaneous examination was done. A tender, pruritic, 1.3 x 1. 3 cm pigmented nodule with an irregular black border was observed on the medial aspect of her left palm. An incision biopsy was performed.
Microscopic evaluation of the tissue specimen showed markedly acanthotic epidermis, nests of melanocytes in both the epidermis and dermis, and presence of dense infiltrates. Atypical cells stained positive for S-100.
The patient was referred to the department of orthopedic surgery for wide local excision.
A complete cutaneous examination was done. A non-tender, non-pruritic irregular black nodule was noted on the medial surface of the 5th digit of her left foot. There were three, solid, non-tender, palpable, lymphadenopathies on the left inguinal area. Incision biopsy was done.
Case Report
Nodular Presentation of Acral Melanoma: A Case Series of Four Filipino Patients
Rochelle Gabrielle G. Galvez*, Katherine Joy B. Sayo-Aguiling and Ma., and Christina B. Gulfan
Department of Dermatology, Jose R. Reyes Memorial Medical Center,
Manila, Philippines
*Address for Correspondence: Rochelle Gabrielle G. Galvez, Department of Dermatology, Jose
R. Reyes Memorial Medical Center, Manila, Philippines E-mail Id: rochelleggalvez@gmail.com
Submission: 09 October, 2025
Accepted: 29 October, 2025
Published: 31 October, 2025
Copyright: © 2025 Galvez RGG, et al. This is an open access
article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Keywords:Melanoma; Acral Melanoma; Acral Nodular Melanoma;
Trauma
Abstract
Cutaneous melanoma (CM), recognized as the most aggressive
form of skin cancer, presents a significant global health burden.
Acral lentiginous melanoma (ALM), a distinct subtype of CM
primarily affecting individuals with darker skin tones, poses diagnostic
challenges due to its diverse clinical presentations. While ALM is
commonly characterized by flat, pigmented lesions, rare reports
have documented its manifestation as a nodular growth. This
case series includes four Filipino cases of nodular ALM, allowing
for a comprehensive analysis and comparison with typical ALM
presentations. Additionally, two case reports of ALM progressing to
nodular growth are presented, further highlighting the clinical variation
within this subtype. The series underscores the importance of accurate
diagnosis through histopathological examination and specific stains,
enabling differentiation from other conditions. Treatment strategies
involve wide local excision or amputation, with additional therapeutic
options for advanced cases. Improved awareness among healthcare
professionals regarding nodular presentations of ALM is crucial for early
detection and optimal management. Further research is needed to
enhance our understanding and refine management strategies for this
challenging subtype of melanoma.
Introduction
Cutaneous melanoma (CM), recognized as the most aggressive
form of skin cancer [1], represents approximately 1% of skin cancers,
yet it accounts for over 80% of skin cancer deaths worldwide. [2,3]
Acral lentiginous melanoma (ALM) or acral melanoma is a distinct
subtype of cutaneous melanoma that primarily affects individuals
with darker skin, like African Americans and Asians.[3,6,7] While
ALM is conventionally characterized by an asymmetric, brown to
black macular lesion with irregular borders, ulcerations, or verrucous
lesions [4,5,6] there have been a few case reports demonstrating the
progression of these lesions to a nodular form [16,17] adding to the
clinical variation and diagnostic complexity of this subtype. Due to
the underreporting of nodular presentations of ALM, differentiating
acral melanoma from other benign nodular lesions, such as
pigmented poromas, and pyogenic granulomas, which are commonly
encountered on acral skin, can pose substantial challenges. [7,8,10,14,18] Misdiagnosis rates for ALM have been reported to be
as high as 25-36%, leading to missed opportunities for early detection
and intervention. [6,7] It is crucial to highlight that ALM is associated
with the poorest prognosis compared to other melanoma subtypes.
[5,12] Studies have consistently shown that ALM is associated with
more advanced disease at diagnosis, resulting in poorer outcomes
and higher mortality rates. [5,6,7,8,13]
In this case series, we aim to shed light on the nodular presentation
of acral melanoma, which represents a rare but significant subset of
cutaneous melanoma cases. Through the presentation and analysis of
four compelling cases, we emphasize the multifaceted nature of its
clinical features. Furthermore, we explore the potential association
between a history of trauma and the development of acral melanoma,
aiming to raise awareness about this unique aspect.
Case Reports
Case 1:
A 63-year-old, male, Filipino farmer presented with a nodular
mass on the middle metatarsal of the left plantar foot. It had begun as
an asymptomatic, dark brown macule which progressively enlarged.
Ten years prior to consultation, the lesion was subjected to trauma
resulting in erosion and subsequent bleeding. Interim revealed rapid
growth of the lesion into an exophytic nodular mass.A complete cutaneous examination was done. A painless, nonpruritic, 3.5 x 3.5 cm nodule with a surrounding hyperpigmented patch was observed in the middle metatarsal of the left plantar foot. Incision biopsy was performed.
Microscopic evaluation of the tissue specimen showed a hyperplastic epidermis and presence of nests of atypical melanocytes along the dermo-epidermal junction extending to the stratum corneum signifying a pagetoid spread. HMB staining was positive. Correlation between the clinical presentation and the pathology findings established the diagnosis of acral nodular melanoma. The patient was referred to Orthopedic Surgery and a below-the-knee amputation was done. Cranial, chest and pelvic CT scan revealed no metastasis. There has been no recurrence of the mass after two months of follow-up.
Case 2:
A 42-year-old female, garment factory worker presented with
a hyperpigmented nodule on the right lateral heel. The lesion had
begun thirty years prior to consult, as a hyperpigmented macule
which gradually enlarged into a patch until two years prior to consult
when the lesion suddenly evolved into a hyperpigmented nodule.History of trauma was noted resulting in erosion and light bleeding on the nodule which progressed to a painful ulceration.
A complete cutaneous examination was done. A slightly tender,
non-pruritic, brownish-black 3x3 cm nodule with a surrounding
hyperpigmented patch was seen on her right lateral heel. There
was a palpable, non-movable, tender lymphadenopathy in the right
inguinal region. An incision biopsy was done.
Microscopic evaluation of the tissue specimen revealed focal absence of the epidermis. Throughout the dermis are nests and sheets of cells. Most of which are large, atypical and have hyperchromatic nuclei. There is also irregular pigment distribution throughout the lesion. Mitotic rate is 1-2 per square millimeter, Clark level IV. HMB 45, MELAN A, and CD34 stained atypical cells.
Following the diagnosis of stage IIC melanoma, a wide local excision was performed with a 2 cm margin and a depth margin of 5 mm. The excised tissue was found to be free of malignant cells. To repair the excisional defect, punch grafting was conducted using skin harvested from the lower abdomen. The patient was advised to have weekly follow-ups for dressing changes. On the thirteenth week after operation, there was noted leveling of the defect with surrounding normal skin and no recurrence of the tumor.
Microscopic evaluation of the tissue specimen revealed focal absence of the epidermis. Throughout the dermis are nests and sheets of cells. Most of which are large, atypical and have hyperchromatic nuclei. There is also irregular pigment distribution throughout the lesion. Mitotic rate is 1-2 per square millimeter, Clark level IV. HMB 45, MELAN A, and CD34 stained atypical cells.
Following the diagnosis of stage IIC melanoma, a wide local excision was performed with a 2 cm margin and a depth margin of 5 mm. The excised tissue was found to be free of malignant cells. To repair the excisional defect, punch grafting was conducted using skin harvested from the lower abdomen. The patient was advised to have weekly follow-ups for dressing changes. On the thirteenth week after operation, there was noted leveling of the defect with surrounding normal skin and no recurrence of the tumor.
Case 3:
A 30-year-old Filipino female sales staff presented with a nodule
on the medial area of her left palm. The patient claims that the lesion
had been present since birth initially as a pigmented linear patch on
her left palm. The lesion remained stable until one year prior to consult
when it gradually expanded into a round black patch. She habitually
picked at the lesion, resulting to an erosion with purulent and bloody
discharge. A thickened hyperpigmented plaque developed, with
irregular borders which further progressed into a nodule with colors
of brown, black, yellow, and red.A complete cutaneous examination was done. A tender, pruritic, 1.3 x 1. 3 cm pigmented nodule with an irregular black border was observed on the medial aspect of her left palm. An incision biopsy was performed.
Microscopic evaluation of the tissue specimen showed markedly acanthotic epidermis, nests of melanocytes in both the epidermis and dermis, and presence of dense infiltrates. Atypical cells stained positive for S-100.
The patient was referred to the department of orthopedic surgery for wide local excision.
Case 4:
A 72-year-old Filipino housewife presented with a nodular mass
on the fifth digit of her left foot. The patient claims that she has always
had a black macule on the medial surface of the 5th digit of her left
foot since childhood. Interim was unremarkable until three weeks
prior to consult when she noted whitish discharge from the macule.
The macule gradually expanded and thickened into a nodule. She
noted pain and changes in color, but no bleeding or ulceration.A complete cutaneous examination was done. A non-tender, non-pruritic irregular black nodule was noted on the medial surface of the 5th digit of her left foot. There were three, solid, non-tender, palpable, lymphadenopathies on the left inguinal area. Incision biopsy was done.
Microscopic evaluation of the tissue specimen revealed stratum
corneum with overlying pigment, acanthosis and papillomatosis,
with nests of melanocytes and lentiginous proliferation at the basal
layer of the epidermis. Nests of atypical melanocytes with mitoses and
pigments were most prominent in the upper dermis.
The patient was referred to the service of orthopedic surgery for surgical removal but was lost to follow-up.
The patient was referred to the service of orthopedic surgery for surgical removal but was lost to follow-up.
Discussion
Acral lentiginous melanoma, named by Reed, is a subtype of
melanoma that primarily affects acral regions of the body. [19] Its
diagnosis has been based on its histological intra-dermal features
showing a diffuse proliferation of large atypical melanocytes along
the epidermal-dermal junction which is dispersed in a lentiginous
pattern with marked acanthosis and elongation of rete ridges. [8,11]
The aforementioned histopathological findings are consistent with
previous reports. [4,11,14] Existing literature describes ALM as
initially pigmented flat lesions that gradually expand and develop
into hyperkeratotic plaques, often with concurrent ulcerations.
[4,7,8,11,14] However, the transformation of stable, long-standing
pigmented lesions to large nodular exophytic growths remains
inadequately reported.
In our institution, a tertiary hospital in Manila, Philippines, only seven cases of acral melanoma have been diagnosed in the past 10 years. According to the Philippine Dermatological Society-Health Information System (PDS-HIS), there have only been 88 recorded cases of acral melanomas from 2013 to 2023 from all PDS-accredited institutions. However, this value is limited to dermatology institutions in the country and does not represent national data.
To the best of our knowledge, only two published reports documented the progression of acral melanoma into a nodular growth. Our study presents four Filipino cases of acral nodular melanoma and discusses two previously published international cases, totaling six cases analyzed.
Smith et al. reported a case involving a 47-year-old Caucasian man with a six-year history of trauma to his left great toe, resulting in toenail damage and ulceration16. Ten months prior to presentation, rapid growth, foul-smelling discharge, tissue sloughing, and bleeding were noted. Examination revealed a 30 x 17-cm fungating, nodular, necrotic mass engulfing his great toe and the majority of the distal medial aspect of his left foot. Three months prior to consult, a mass appeared in the patient’s left groin, along with scattered firm nodules on the left calf and thigh. Biopsy confirmed the diagnosis of primary melanoma and metastatic melanoma, with histology showing atypical S100 epithelioid cells with perineural invasion. Imaging revealed widespread metastasis. Partial surgical excision of the left foot mass was performed to improve the patient’s quality of life. Subsequently, the patient participated in an Ipilimumab monotherapy clinical trial, which was discontinued due to an immune-related adverse event. Unfortunately, he succumbed to metastatic disease four months after initial presentation.
In our institution, a tertiary hospital in Manila, Philippines, only seven cases of acral melanoma have been diagnosed in the past 10 years. According to the Philippine Dermatological Society-Health Information System (PDS-HIS), there have only been 88 recorded cases of acral melanomas from 2013 to 2023 from all PDS-accredited institutions. However, this value is limited to dermatology institutions in the country and does not represent national data.
To the best of our knowledge, only two published reports documented the progression of acral melanoma into a nodular growth. Our study presents four Filipino cases of acral nodular melanoma and discusses two previously published international cases, totaling six cases analyzed.
Smith et al. reported a case involving a 47-year-old Caucasian man with a six-year history of trauma to his left great toe, resulting in toenail damage and ulceration16. Ten months prior to presentation, rapid growth, foul-smelling discharge, tissue sloughing, and bleeding were noted. Examination revealed a 30 x 17-cm fungating, nodular, necrotic mass engulfing his great toe and the majority of the distal medial aspect of his left foot. Three months prior to consult, a mass appeared in the patient’s left groin, along with scattered firm nodules on the left calf and thigh. Biopsy confirmed the diagnosis of primary melanoma and metastatic melanoma, with histology showing atypical S100 epithelioid cells with perineural invasion. Imaging revealed widespread metastasis. Partial surgical excision of the left foot mass was performed to improve the patient’s quality of life. Subsequently, the patient participated in an Ipilimumab monotherapy clinical trial, which was discontinued due to an immune-related adverse event. Unfortunately, he succumbed to metastatic disease four months after initial presentation.
The second report by Putnam, et al. that described a 68-year-old
Sierra Leonean woman who presented with a painful, ulcerating mass
on her left foot [15]. Initially, the lesion appeared as hyperpigmentation
and gradually progressed into a necrotic patch over a year. Despite
the progression of the lesion, the patient delayed seeking medical
attention. The initial excision of the lesion at a local health facility
lacked pathological examination. In the following months, the lesion
grew into a 10 cm x 5 cm fungating mass with contact bleeding.
Biopsy analysis confirmed the diagnosis of malignant melanoma,
characterized by pleomorphic cells, necrotic areas, and a high
mitotic rate with positive S100 and Melan A expression. Below-knee
amputation was performed, but the patient was subsequently lost to
follow-up.
To augment these findings, our study includes four Filipino cases,
contributing to an in-depth analysis of six acral nodular melanomas.
Essential characteristics of these cases are outlined in both
[Table 1] and [Table 2] . Our case series uniquely stands out by presenting a distinctive demographic profile. Notably, our patients had a
relatively younger age, with an average of 55.3 years, challenging the
conventional norms reported in earlier research, which indicated
mean ages ranging from 63.166 to 63.914. This discrepancy prompts
us to reevaluate the factors influencing age-related variations in acral
melanoma presentation, potentially uncovering new risk factors or
genetic predispositions.
Of the six cases, five were localized on the foot, while one occurred
on the hand. This aligns with previous findings on typical ALM, where
the majority of lesions occur on the feet, particularly the soles.
[22,23]
The evolution of lesions from flat to nodular forms displayed
varying timeframes, ranging from three weeks to twenty-four months.
This unique observation highlights a crucial aspect previously
unexplored, offering a novel perspective on the transformation of
these lesions.
Remarkably, all cases except one demonstrated the intriguing
occurrence of nodular growth following a history of trauma. The
transformation from stable pigmented flat lesions or ulcers to nodular
growths, often correlated with trauma, signifies a distinct pattern
within this subset of patients. The conjectured role of trauma in
ALM formation has been explored in several studies. [9,13,14,20] A
retrospective investigation by Hao et al. suggested that trauma led to
rapid progression and a shorter disease duration in pre-existing acral
melanomas, a trend paralleled in five out of six patients in our study.
However, the precise relationship between trauma and ALM remains
contentious, as indicated by divergent findings in other studies
[8,21], underscoring the need for further investigation.
Histopathological analysis consistently unveils typical ALM
characteristics, encompassing melanocyte nests within the DEJ
and dermis, pagetoid melanocyte dispersion, atypical mitoses, and
heightened apoptosis. Immunostaining for biomarkers related to
malignant melanocytes, including S-100, HMB-45, and Melan-A,
aids both diagnosis and differential diagnosis, providing valuable
insights for clinicians.
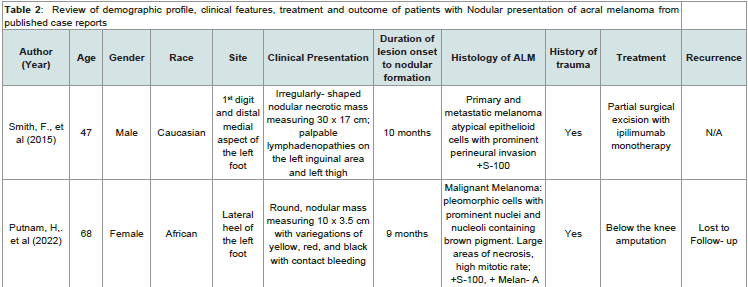
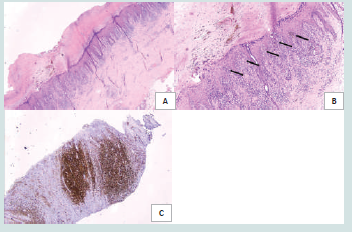
Table 1:Review of demographic profile, clinical features, treatment and outcome of patients with Nodular presentation of Acral Melanoma
Table2: Review of demographic profile, clinical features, treatment and outcome of patients with Nodular presentation of acral melanoma from published case reports
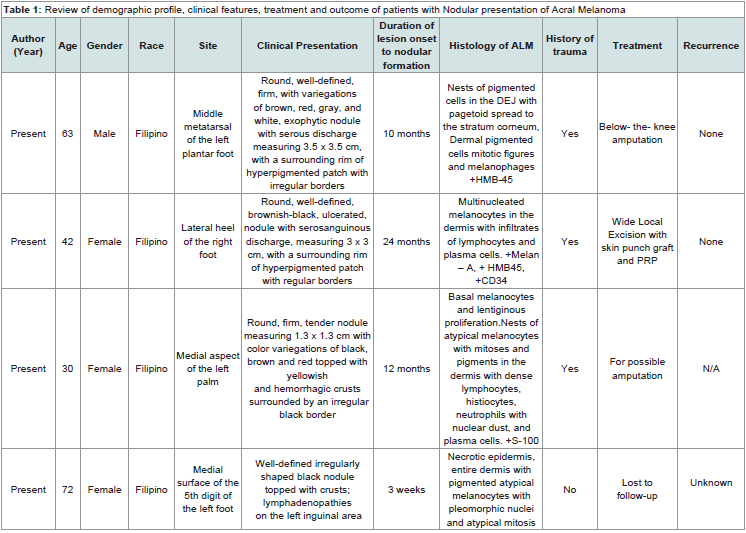
Figure 1: Morphologic features of acral melanoma
Figure 1: A close view of acral melanoma presenting as a solitary, round, well-defined, firm, with variegations of brown, red, gray, and white, exophytic nodule with serous discharge, measuring 3.5 x 3.5 cm, with a surrounding rim of hyperpigmented patch with irregular borders, on the middle metatarsal of the left plantar foot of a 63-year-old Fitzpatrick skin type IV Filipino male.
Figure 1: A close view of acral melanoma presenting as a solitary, round, well-defined, firm, with variegations of brown, red, gray, and white, exophytic nodule with serous discharge, measuring 3.5 x 3.5 cm, with a surrounding rim of hyperpigmented patch with irregular borders, on the middle metatarsal of the left plantar foot of a 63-year-old Fitzpatrick skin type IV Filipino male.
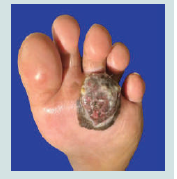
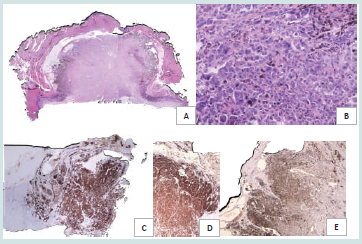
Figure 2: Histopathologic features of acral melanoma
Figure 2: Distant (A, C) and closer (B) views of microscopic findings of acral melanoma. Stratum corneum with hyperkeratosis, epidermis with hypergranulosis and basal layer hyperpigmentation, dense, bandlike infiltrates of lymphocytes and histiocytes in the dermis (A). Nests of atypical pigmented cells (black arrows) from the DEJ extending up to the stratum corneum signifying pagetoid spread (B). HMB-45 staining was strongly positive and very extensive. It highlighted the nests of melanocytic cells in the entire dermis, with no maturation and dispersion (C).
Figure 2: Distant (A, C) and closer (B) views of microscopic findings of acral melanoma. Stratum corneum with hyperkeratosis, epidermis with hypergranulosis and basal layer hyperpigmentation, dense, bandlike infiltrates of lymphocytes and histiocytes in the dermis (A). Nests of atypical pigmented cells (black arrows) from the DEJ extending up to the stratum corneum signifying pagetoid spread (B). HMB-45 staining was strongly positive and very extensive. It highlighted the nests of melanocytic cells in the entire dermis, with no maturation and dispersion (C).
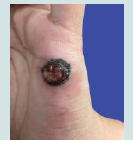
Figure 3: Clinical features of acral melanoma
Figure 3: A solitary, round, well-defined, brownish-black, ulcerated, nodule with serosanguinous discharge, measuring 3 x 3 cm, with a surrounding rim of hyperpigmented patch with regular borders, on the right lateral heel of a 42-year-old Fitzpatrick skin type IV Filipino female.
Figure 3: A solitary, round, well-defined, brownish-black, ulcerated, nodule with serosanguinous discharge, measuring 3 x 3 cm, with a surrounding rim of hyperpigmented patch with regular borders, on the right lateral heel of a 42-year-old Fitzpatrick skin type IV Filipino female.
Figure 4:Pathologic features of acral melanoma
Figure 4:The scanning view (A) reveals a tumor with a stratum corneum presenting with thick compact orthokeratosis, acanthotic epidermis with hypergranulosis, a dermis with multiple nests and sheets of atypical cells with melanin pigment. On closer magnification (B), there are multinucleated melanocytes and surrounding infiltrates of lymphocytes and plasma cells in the dermis. The tissue section showed diffuse staining of melanocytes in the dermis and yield a positive Melan – A (C), HMB-45 (D), and CD34 (E).
Figure 4:The scanning view (A) reveals a tumor with a stratum corneum presenting with thick compact orthokeratosis, acanthotic epidermis with hypergranulosis, a dermis with multiple nests and sheets of atypical cells with melanin pigment. On closer magnification (B), there are multinucleated melanocytes and surrounding infiltrates of lymphocytes and plasma cells in the dermis. The tissue section showed diffuse staining of melanocytes in the dermis and yield a positive Melan – A (C), HMB-45 (D), and CD34 (E).
Figure 5: Acral melanoma presenting as a nodule on the left palm
Figure 5:A solitary 1.3 x 1.3 cm round, firm, tender nodule with color variegations of black, brown and red topped with yellowish and hemorrhagic crusts surrounded by an irregular black border on the ulnar aspect of the left palm of a 30-year-old Fitzpatrick IV Filipino female.
Figure 5:A solitary 1.3 x 1.3 cm round, firm, tender nodule with color variegations of black, brown and red topped with yellowish and hemorrhagic crusts surrounded by an irregular black border on the ulnar aspect of the left palm of a 30-year-old Fitzpatrick IV Filipino female.
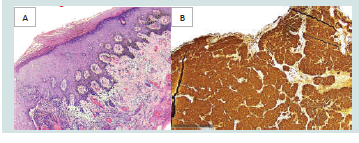
Figure 6: Acral melanoma with characteristic pathologic features
Figure 6:The epidermis shows acanthosis and papillomatosis with nests of melanocytes and lentiginous proliferation at the basal layer (A). In the dermis are nests of atypical melanocytes with mitoses and pigments surrounding the dilated and congested blood vessels (A). There are dense infiltrates of the lymphocytes, histiocytes, neutrophils with nuclear dust, and some plasma cells (A). Special staining with S-100 was positive (B).
Figure 6:The epidermis shows acanthosis and papillomatosis with nests of melanocytes and lentiginous proliferation at the basal layer (A). In the dermis are nests of atypical melanocytes with mitoses and pigments surrounding the dilated and congested blood vessels (A). There are dense infiltrates of the lymphocytes, histiocytes, neutrophils with nuclear dust, and some plasma cells (A). Special staining with S-100 was positive (B).
Figure 7:Acral melanoma with characteristic pathologic features
Figure 7:A solitary well defined, irregularly- shaped, black nodule topped with crusts on the medial surface of the 5th digit of the left foot of a 72-year-old Fitzpatrick IV Filipino female.
Figure 7:A solitary well defined, irregularly- shaped, black nodule topped with crusts on the medial surface of the 5th digit of the left foot of a 72-year-old Fitzpatrick IV Filipino female.
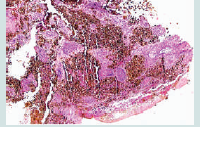
Figure 8:Microscopic features of acral melanoma
Figure 8:Stratum corneum with overlying pigment, acanthosis and papillomatosis, with nests of melanocytes and lentiginous proliferation at the basal layer of the epidermis. Nests of atypical melanocytes with mitoses and pigments were most prominent in the upper dermis.
Figure 8:Stratum corneum with overlying pigment, acanthosis and papillomatosis, with nests of melanocytes and lentiginous proliferation at the basal layer of the epidermis. Nests of atypical melanocytes with mitoses and pigments were most prominent in the upper dermis.
The diagnostic landscape of ALM is challenging, often mirroring
various conditions such as chronic foot diabetic ulcers, acral
lentiginous nevi, hematoma, ischemic necrosis, and palmoplantar
warts—frequently encountered as differential diagnoses. [8,9,11,15,19]
Moreover, the nodular presentation of ALM occasionally intertwines
with other acral nodular lesions like pyogenic granuloma, poroma,
and schwannoma, exacerbating the already high rate of misdiagnosis.
[8,9,11,15,19] To ensure accurate differentiation, biopsies coupled
with specific stains and biomarkers remain integral components of a
definitive diagnosis for nodular ALM.
In terms of treatment strategies, ALM primarily necessitates
wide local excision (WLE) to achieve tumor-free margins or
amputation.[3,4,11,14 ]Tailoring treatment to factors like tumor location,
size, depth of invasion, and sentinel lymph node (SLN) status may
warrant a sentinel lymph node biopsy.[11,12,14] Advanced stages
may call for alternative interventions like radiotherapy, cryotherapy,
and immunotherapy if surgical interventions are ineffective.
[1] Among our cases, three patients underwent amputation, one received
wide local excision with skin punch graft and platelet-rich plasma
therapy, while another pursued partial surgical excision coupled
with ipilimumab monotherapy-tragically succumbing to metastatic
disease. Regrettably, one patient’s outcome remained uncertain due to
loss of follow-up. Encouragingly, survivors exhibited no recurrences
of the disease.
Our findings have broad implications for both clinical practice and
research, providing new insights that encourage further exploration
within the medical community. By examining demographics and
investigating the potential influence of trauma on ALM progression,
our study highlights the complex nature of this disease and the need
for deeper investigation. While we acknowledge the limitations, such
as our relatively small sample size, we invite future research to build
upon our findings, potentially refining diagnostic approaches and
improving treatments.
Conclusion
In summary, our study on acral nodular melanomas provides
important insights into a less-explored aspect of melanoma. Our
findings on the progression from stable pigmented lesions to
nodular growths, often linked with trauma, offer a fresh perspective
not previously investigated. The unique demographic profile we
observed, with a younger patient population, challenges existing
norms and prompts further exploration into age-related variations
in acral melanoma presentation. The diagnostic challenges, due
to similarities with other acral lesions, highlight the importance of
precise diagnostics. Our study contributes to clinical understanding
and underscores the ongoing need for research into ALM progression
and treatment response. While mindful of our study’s limitations,
including sample size, we encourage future research to build on our
findings, potentially refining diagnosis and treatment approaches.
References
2. Saginala K, Barsouk A, Aluru JS, Rawla P, Barsouk A. (2021) Epidemiology of melanoma. Med Sci 9: 63.