Journal of Clinical and Investigative Dermatology
Download PDF
Case Report
Linear Pigmented Discoid Lupus Erythematosus on the Scalp of a 52-Year-Old Male, Filipino Treated with Pico Laser: A Case Report
Michaela Gabrielle G. Guieb*, Ma. Flordeliz Abad- Casintahan and Ma. Eleanor Cathryn D. Salonga
Department of Dermatology, Jose R. Reyes Memorial Medical Center, Manila, Philippines
*Address for Correspondence:Michaela Gabrielle G. Guieb, Department of Dermatology, Jose
R. Reyes Memorial Medical Center, Manila, Philippines. E-mail Id: micaaaguieb@gmail.com
Submission: 13 September, 2025
Accepted: 07 October, 2025
Published:10 October, 2025
Accepted: 07 October, 2025
Published:10 October, 2025
Copyright: © 2025 Guieb MGG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Linear Pigmented Discoid Lupus Erythematosus; DLE;
Super High Potency Corticosteroid; Calcineurin Inhibitor; Pico Laser
Abstract
Linear cutaneous lupus erythematosus is an exceptionally rare
variant of cutaneous lupus erythematosus (CLE) characterized by
linear erythematous plaques along the lines of Blaschko. This case
report describes a unique presentation of linear pigmented discoid
lupus erythematosus (DLE) in a 52-year-old, male, Filipino with a history
of intense sun exposure. The patient presented with a progressive
hyperpigmented linear plaque on the left frontal and left parietal area,
without systemic symptoms. The patient demonstrated improvement
following a treatment of super high potency topical corticosteroid then
topical calcineurin inhibitor with strict photoprotection, and adjunctive
measures. The lesions decreased in thickness, hyperpigmentation,
and scaling. The Cutaneous Lupus Erythematosus Disease Area and
Severity Index showed a decrease in the activity score from six to
two, indicating a positive treatment response. Hyperpigmentation
of the plaques decreased after two treatment sessions and showed
further improvement at one-year follow-up. This is the first reported
case of linear DLE on the scalp among local journals in the Philippines,
highlighting the importance of considering CLE in the differential
diagnosis of linear hyperpigmented plaques, even in the absence of
systemic symptoms. This is also the first known case to use pico laser
as treatment for DLE, based from our knowledge and from published
literature.
Introduction
Lupus erythematosus, a multisystem disorder affecting the skin,
involves complex interactions between immunologic, genetic, and
environmental factors.[1] In the Philippines, it occurs in 30 to 50
per 100,000 people, compared to 20 to 150 per 100,000 in the United
States [2]. Linear cutaneous lupus erythematosus (LCLE) is a rare
variant, characterized by linear erythematous plaques along Blaschko
lines, with the first case reported in 1998.[3] Among reported LCLE
cases, 39.2% were diagnosed as DLE. Nine cases of adult-onset linear
CLE on the forehead have been documented.[4] Due to LCLE’s rarity
and limited data, further research and case studies are needed to
enhance our understanding of its pathogenesis, clinical features, and
optimal management.
Discoid lupus erythematosus is a chronic form of cutaneous
lupus, primarily affects the skin characterized by round or disk shaped
lesions that may be scaly, red, and inflamed. It can cause
changes in skin pigmentation and may lead to scarring or hair loss.
It occurs more frequently in women during their fourth and fifth
decades of life. The prevalence of lupus can vary between different
populations and regions.[2]
Linear cutaneous lupus erythematosus primarily affects children
and young adults, with a mean age of onset of 22 years. It shows no
gender predilection and involves single or multiple asymptomatic
linear erythematous plaques following the lines of Blaschko. The most
affected areas include the head, neck, trunk, then extremities.[4]
As far as the available records indicate, only 16 cases of LCLE
involving the scalp have been reported in the English language
as of 2022.[5] Only 23 patients reported patients were from Asia.
[3,6,7] In the Philippines, there has been 724 cases of discoid lupus
erythematosus with no reported case of being linear in pattern from
2011 to 2022.[8]
It is a connective tissue disease with a complex mix of
immunologic, genetic, and environmental factors. Possible triggers
include trauma, viral infections, irritation, or exposure to agents like
ultraviolet (UV) light, drugs, pesticides, metals, and more. Among
these, UV radiation is particularly linked to lupus-specific skin
issues in this patient. Photosensitivity and antinuclear antibody
(ANA) test results are usually negative or weakly positive in linear
cutaneous lupus erythematosus.[9] Histologically, it shows features
like hyperkeratosis, follicular plugging, epidermal atrophy, and
basal layer degeneration with dense lymphocyte infiltration around
blood vessels and adnexal structures, along with dermal pigmentary
changes.[10]
It has been observed that 5% to 15% of patients with DLE have
the potential to progress and develop SLE.[9] The timeframe between
the initial diagnosis of DLE and the onset of SLE vary significantly
with intervals ranging from four months to 34 years.[11] From our
knowledge and from published literature, no current data of linear
DLE has developed to SLE.
Case Report
A 52-year-old, male, Filipino who is a retired medical
technologist from Cavite presented with a 3-month history of solitary,
hyperpigmented linear plaque on the left frontal area extending to the
forehead. There were no pain, tenderness, pruritus, scales, hair loss,
malar rash, oral ulcers, fever, dyspnea, chest pain, bubbly urine, joint
pains, muscle pains, seizures, dizziness and pallor. No topical agents
used prior. He went to the beach with no sun protection one month
prior to the appearance of lesion. No medications were taken nor
applied. Interval history showed increase in size and pigmentation of
the lesion extending in a linear, downward fashion and appearance
of fine, whitish, adherent scales. Persistence of the linear plaque
prompted consultation.
He has no comorbidities and no known allergy. He has had no
prior surgeries, injuries and accidents and did not receive blood
transfusion or any of its components. He has no record of taking
any medications and supplements. He has no history of prolonged
exposure to ionizing radiation. He has no history of herpes zoster
infection. He has a family history of hypertension, diabetes mellitus,
psoriasis and rheumatoid arthritis. He is a 20 pack-year smoker and
occasional alcoholic beverage drinker.
He presented with a solitary, well demarcated, linear violaceous
to hyperpigmented plaque measuring 8 cm in length and 2 cm
in width diameter with flat hyperpigmented borders and central
hypopigmented area with scanty, fine adherent scale in the left
frontal area extending to the forehead [Figure 1A] and a solitary,
well demarcated, irregularly shaped, slightly hyperpigmented plaque
measuring 3 cm by 2 cm with scanty, fine, adherent whitish scale with
hair loss on the left parietal area [Figure 1B]. There was a positive
carpet tack sign. No hair loss but with hair thinning was noted.
There were no lesions on the neck, chest and abdomen, back,
axilla, both upper and lower extremities, palms and soles. No nail
changes were seen.
Ancillaries showed leukopenia and eosinophilia. Chemistry panel of blood urea nitrogen, creatinine, fasting blood sugar, hemoglobin A1C, aspartate aminotransferase, alanine aminotransferase and blood uric acid were all normal. Lipid profile showed elevated lowdensity lipoprotein. No casts, no hematuria, no proteinuria were seen on urinalysis. C-reactive protein and antinuclear antibody were both negative. Chest X-ray showed essentially unremarkable findings.
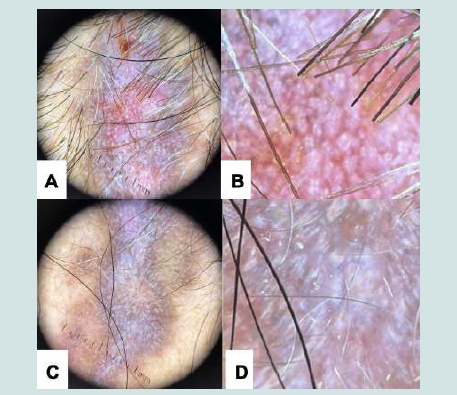
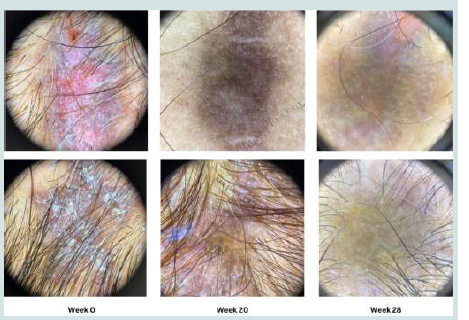
Dermoscopy on the left frontal area showed follicular keratotic plugs with perifollicular white halos, rosettes, yellow dots and irregular linear vessels. There is presence of white structureless areas and pink white background and speckled brown pigmentation [Figure 2].
Dermoscopy on the left parietal area of the scalp revealed perifollicular white yellowish scales and follicular keratotic plugs [Figure 3].
Ancillaries showed leukopenia and eosinophilia. Chemistry panel of blood urea nitrogen, creatinine, fasting blood sugar, hemoglobin A1C, aspartate aminotransferase, alanine aminotransferase and blood uric acid were all normal. Lipid profile showed elevated lowdensity lipoprotein. No casts, no hematuria, no proteinuria were seen on urinalysis. C-reactive protein and antinuclear antibody were both negative. Chest X-ray showed essentially unremarkable findings.
Dermoscopy on the left frontal area showed follicular keratotic plugs with perifollicular white halos, rosettes, yellow dots and irregular linear vessels. There is presence of white structureless areas and pink white background and speckled brown pigmentation [Figure 2].
Dermoscopy on the left parietal area of the scalp revealed perifollicular white yellowish scales and follicular keratotic plugs [Figure 3].
Figure 1: Initial photo of the patient showing a plaque on left frontal area (A)
and left parietal area (B)
There were no proximal nailfold capillary changes seen in
capillaroscopy.
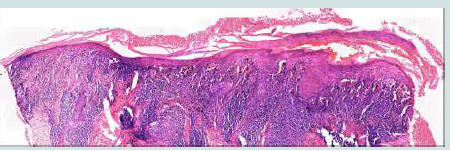
Biopsy was done on the left frontal area. Stratum corneum showed marked parakeratosis. The epidermis was atrophic with focal areas of hyperplasia [Figure 4].
There was extensive basal vacuolar alteration with presence of melanophages in the papillary dermis [Figure 5A] with presence of some necrotic keratinocytes [Figure 5B]. In the dermis are lichenoid, superficial and deep patchy dense perivascular and periadnexal infiltrates of lymphohistiocytes [Figure 5C]. The blood vessels were telangiectatic in the upper dermis [Figure 5D].
Biopsy was done on the left frontal area. Stratum corneum showed marked parakeratosis. The epidermis was atrophic with focal areas of hyperplasia [Figure 4].
There was extensive basal vacuolar alteration with presence of melanophages in the papillary dermis [Figure 5A] with presence of some necrotic keratinocytes [Figure 5B]. In the dermis are lichenoid, superficial and deep patchy dense perivascular and periadnexal infiltrates of lymphohistiocytes [Figure 5C]. The blood vessels were telangiectatic in the upper dermis [Figure 5D].
Figure 5:Hematoxylin-Eosin-stained section with 40x magnification (A.
vacuolar interface, B. necrotic keratinocytes, C. patchy dense infiltrates, D.
telangiectatic blood vessels)
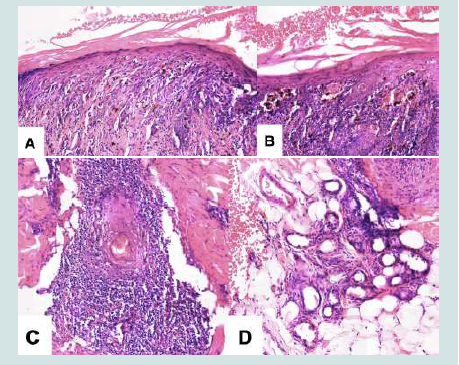
Alcian blue staining was strongly positive for interstitial mucin
deposition with enhancement of the blue color both in the dermis and
around the perivascular and periadnexal structures [Figure 6].
Patient was treated with super high potency topical corticosteroid, clobetasol propionate 0.05% ointment twice a day for two weeks then once a day for the next two weeks. He was advised with strict photoprotection, mild soap and emollients. He was encouraged to discontinue cigarette smoking and to follow-up after two weeks.
There was decrease in the thickness, hyperpigmentation, scaling of plaques on forehead and scalp on follow-up. In week four, medication was shifted to topical calcineurin inhibitor, tacrolimus 0.1% ointment applied twice a day to lesions for 20 weeks. Further decrease in the thickness, hyperpigmentation and scaling of plaques on forehead and scalp was seen [Figure 7] [Figure 8]. Dermoscopy showed disappearance of the follicular plugs, perifollicular white halos, rosettes, yellow dots, and telangiectatic vessels from the baseline. Only brown pigmentation and few white structureless areas remained (Figure 9).
Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI) was measured and activity score decreased from six to two suggesting a positive response to the treatment.
Thereafter, the patient had pico laser treatment. The treatment parameters of Nd:YAG picosecond laser were 1,064 nm, 3-mm spot size, fluences 0.8 J/cm2, 1 Hz with one pass and whitish gray spot as the end point. Regular follow-up appointments of every four weeks were scheduled and showed adverse effects of pruritus. There was decrease in hyperpigmentation on the plaques after two sessions. Furthermore, there was decrease in hyperpigmentation after one-year of follow-up with constant sun protection.
Patient was treated with super high potency topical corticosteroid, clobetasol propionate 0.05% ointment twice a day for two weeks then once a day for the next two weeks. He was advised with strict photoprotection, mild soap and emollients. He was encouraged to discontinue cigarette smoking and to follow-up after two weeks.
There was decrease in the thickness, hyperpigmentation, scaling of plaques on forehead and scalp on follow-up. In week four, medication was shifted to topical calcineurin inhibitor, tacrolimus 0.1% ointment applied twice a day to lesions for 20 weeks. Further decrease in the thickness, hyperpigmentation and scaling of plaques on forehead and scalp was seen [Figure 7] [Figure 8]. Dermoscopy showed disappearance of the follicular plugs, perifollicular white halos, rosettes, yellow dots, and telangiectatic vessels from the baseline. Only brown pigmentation and few white structureless areas remained (Figure 9).
Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI) was measured and activity score decreased from six to two suggesting a positive response to the treatment.
Thereafter, the patient had pico laser treatment. The treatment parameters of Nd:YAG picosecond laser were 1,064 nm, 3-mm spot size, fluences 0.8 J/cm2, 1 Hz with one pass and whitish gray spot as the end point. Regular follow-up appointments of every four weeks were scheduled and showed adverse effects of pruritus. There was decrease in hyperpigmentation on the plaques after two sessions. Furthermore, there was decrease in hyperpigmentation after one-year of follow-up with constant sun protection.
Discussion
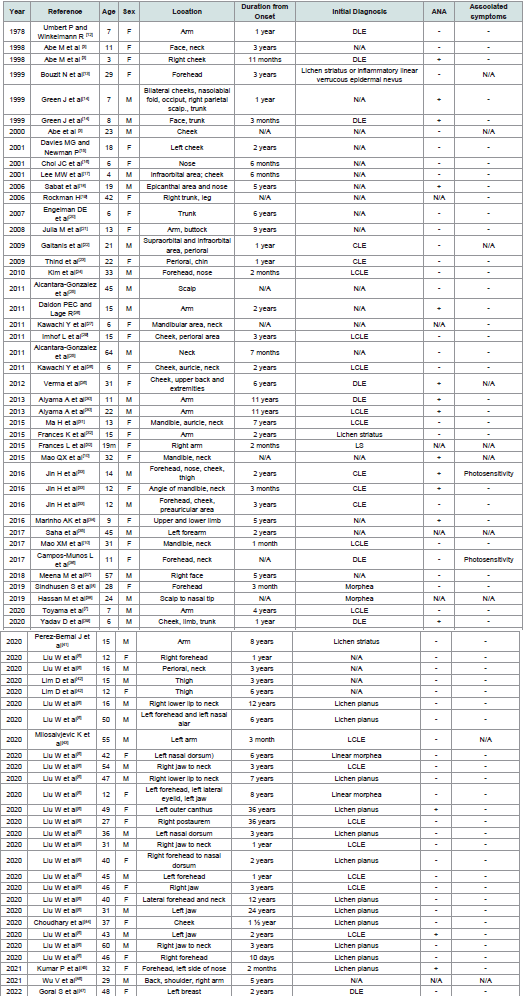
From 1978 to 2022, 72 cases of linear DLE were reported in 45
global journals. The patients had an average age of 24.47 years, and
there was nearly an equal distribution between genders, with 35 males
and 37 females [Table 1].
The most affected location was the face (72%) followed by upper
extremities (21%), neck (19%), trunk (7%), lower extremities (5.5%),
scalp (4.1%), back (3%), and buttock (1.3%) [Table 1]. The average
duration from onset to presentation was approximately 4.5 years.
The initial diagnoses included linear cutaneous lupus erythematosus (24%), lichen planus (18%), discoid lupus erythematosus (12%), morphea (7%), lichen striatus (6%), epidermal nevus (2%), and unspecified diagnosis (31%). Among the patients, 22% had positive ANA tests, and 4.6% experienced photosensitivity symptoms (Table 1). Treatment strategies included photoprotection, topical or intralesional corticosteroids, and calcineurin inhibitors. Some used hydroxychloroquine alongside strict sun protection. While some patients improved, others had persistent posthyperpigmentation despite treatment.
The initial diagnoses included linear cutaneous lupus erythematosus (24%), lichen planus (18%), discoid lupus erythematosus (12%), morphea (7%), lichen striatus (6%), epidermal nevus (2%), and unspecified diagnosis (31%). Among the patients, 22% had positive ANA tests, and 4.6% experienced photosensitivity symptoms (Table 1). Treatment strategies included photoprotection, topical or intralesional corticosteroids, and calcineurin inhibitors. Some used hydroxychloroquine alongside strict sun protection. While some patients improved, others had persistent posthyperpigmentation despite treatment.
Acute exacerbations of DLE are typically treated with high
potency topical corticosteroids to reduce inflammation and promote
healing. Improvement is often seen within two weeks. Once lesions
show signs of inactivity, treatment can stop. Prolonged use of topical
corticosteroids may cause skin thinning. Alternative therapies can be
considered if there is no response to topical corticosteroids. Topical
calcineurin inhibitors like tacrolimus or pimecrolimus are options,
especially for facial involvement. They modulate the skin’s immune
response without causing atrophy. Physical treatments like laser
therapy, cryotherapy, and dermabrasion can also manage CLE.[9]
Previous research found that combining intense pulsed light
(IPL) and Q-switched 1,064-nm Nd:YAG laser effectively treated
DLE scarring lesions without worsening them.[48]
In a separate study, a 1,064-nm long-pulse Nd:YAG laser improved DLE lesions in three sessions, three weeks apart. [49]
Another study used pulsed dye laser (PDL) on 12 DLE patients three times, six weeks apart, resulting in decreased erythema and scaling/hypertrophy scores after six weeks, but no significant change in damage CLASI scores.[50]
In a different study, flashlamp PDL and long PDL showed an average improvement in over 60% of treated lesions, with some side effects like transient hyperpigmentation, mild scarring, and a few relapses after more than a year of treatment.[51]
In a separate study, a 1,064-nm long-pulse Nd:YAG laser improved DLE lesions in three sessions, three weeks apart. [49]
Another study used pulsed dye laser (PDL) on 12 DLE patients three times, six weeks apart, resulting in decreased erythema and scaling/hypertrophy scores after six weeks, but no significant change in damage CLASI scores.[50]
In a different study, flashlamp PDL and long PDL showed an average improvement in over 60% of treated lesions, with some side effects like transient hyperpigmentation, mild scarring, and a few relapses after more than a year of treatment.[51]
Erbium-doped yttrium-aluminum-garnet (Er:YAG) laser
treatment involved two sessions with six to ten passes. After one
week, treated areas reepithelialized smoothly with minimal residual
erythema and no scarring. There was no disease reactivation observed
in both treated and untreated areas at a two-year follow-up.[52]
Pico laser, or picosecond Nd: YAG laser, delivers ultra-short
laser pulses, approximately 1/1000 of a nanosecond, compared to
traditional lasers. It targets skin concerns like tattoo removal, wrinkle
reduction, and pigmentation removal efficiently and precisely. Its
rapid energy delivery breaks down pigment or tissue without harming
surrounding skin, reducing burns and pigmentation changes. Pico
laser’s faster rate breaks up ink or pigmentation into smaller particles,
potentially speeding up and enhancing removal safely.[53] Based from
our knowledge and from published literature, no linear DLE has been
treated with pico laser. For this patient, pico laser was used for two
sessions and regular follow-up appointments of every four weeks were
scheduled. It showed adverse effects of pruritus. Hyperpigmentation
of the plaques decreased after two treatment sessions and showed
further improvement at one-year follow-up.
An additional consideration is whether the patient had a prior history of herpes zoster. Discoid lupus erythematosus has been reported to occur at sites of healed herpes zoster, often interpreted as an example of Wolf’s isotopic response. [54-57] Although this history was not present in our patient, including such detail may provide important clinical context in similar cases. Notably, herpes zoster has also been observed on the scalp following Gam-COVIDVac vaccination,[58] underscoring the potential interplay between viral infections, immune modulation, and cutaneous autoimmune manifestations.
An additional consideration is whether the patient had a prior history of herpes zoster. Discoid lupus erythematosus has been reported to occur at sites of healed herpes zoster, often interpreted as an example of Wolf’s isotopic response. [54-57] Although this history was not present in our patient, including such detail may provide important clinical context in similar cases. Notably, herpes zoster has also been observed on the scalp following Gam-COVIDVac vaccination,[58] underscoring the potential interplay between viral infections, immune modulation, and cutaneous autoimmune manifestations.
Conclusion
This is the first reported case of linear pigmented DLE on the
scalp in the Philippines. It is also the first known case to use pico laser
as treatment for DLE, based from our knowledge and from published
literature. The case involves a 52-year-old Filipino male with a rare
presentation of linear pigmented DLE. He had a hyperpigmented
linear plaque on the left frontal and parietal areas, preceded by intense
sun exposure. No systemic symptoms were reported, and the patient
had no significant medical history or known allergies.
This case emphasizes considering CLE as a potential diagnosis in patients with linear hyperpigmented plaques and sun exposure history, even without systemic symptoms. Treatment included a super high potency topical corticosteroid, strict photoprotection, and adjunctive measures, leading to decreased thickness, hyperpigmentation, and scaling. Topical calcineurin inhibitor was applied twice daily for 20 weeks, further improving the lesions. Dermoscopy revealed significant improvement, with only brown pigmentation and a few white areas left after 20 weeks. The CLASI score decreased from six to two, indicating a positive response to treatment. Hyperpigmentation of the plaques decreased after two treatment sessions and showed further improvement at one-year follow-up.
This case emphasizes considering CLE as a potential diagnosis in patients with linear hyperpigmented plaques and sun exposure history, even without systemic symptoms. Treatment included a super high potency topical corticosteroid, strict photoprotection, and adjunctive measures, leading to decreased thickness, hyperpigmentation, and scaling. Topical calcineurin inhibitor was applied twice daily for 20 weeks, further improving the lesions. Dermoscopy revealed significant improvement, with only brown pigmentation and a few white areas left after 20 weeks. The CLASI score decreased from six to two, indicating a positive response to treatment. Hyperpigmentation of the plaques decreased after two treatment sessions and showed further improvement at one-year follow-up.