Journal of Clinical and Investigative Dermatology
Download PDF
Case Report
Uncommon Petaloid Form of Seborrheic Dermatitis Seen In Fitzpatrick Skin Types V-VI
TongFan Wu1, Frommeyer TC1,2, Rohan CA1,2,3 and Travers JB 1,2,3*
1Department of Dermatology, Boonshoft School of Medicine at Wright State University, Dayton Ohio USA
2Department of Pharmacology & Toxicology, Boonshoft School of Medicine at Wright State University, Dayton Ohio, USA
3Department of Medicine (Dermatology), Dayton Veterans Administration Medical Center, Dayton, Ohio USA
2Department of Pharmacology & Toxicology, Boonshoft School of Medicine at Wright State University, Dayton Ohio, USA
3Department of Medicine (Dermatology), Dayton Veterans Administration Medical Center, Dayton, Ohio USA
*Address for Correspondence: Jeffrey B. Travers, M.D., Ph.D., Department of Pharmacology and Toxicology, Boonshoft School of Medicine at Wright State, University 3640 Col Glenn Hwy, Dayton, OH 45435. E-mail Id: jeffrey.travers@wright.edu
Submission: 26 June, 2023
Accepted: 24 July, 2023
Published: 27 July, 2023
Copyright: © 2023 Wu T, et al. This is an open access article
distributed under the Creative Commons Attri-bution License,
which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Keywords: Seborrhea-Like Dermatitis with Psoriasiform Elements
(C565217); 17-Hydroxycorticosteroids (D015065); Ketoconazole (D007654) ; Petaloid Seborrheic Dermatitis; Fitzpatrick V-VI, Skin of Color
Abstract
Background: Seborrheic dermatitis (SD) is an inflammatory disease
that has papulosquamous morphology in areas rich in sebaceous
glands such as the scalp, face, and body folds. Petaloid SD is an
uncommon presentation found in patients with dark skin (Fitzpatrick
Skin type V-VI). This form of SD can appear as pink or hypopigmented
polycyclic coalescing rings or scaly macules and patches in the typical
areas SD appears, which can mimic other conditions including lupus
erythematosus. There is significant disproportion in the representation of
darker skin types in dermatological textbooks and scarce literature on
petaloid SD. This case demonstrates the presentation of the petaloid
SD in an African American patient to contribute to the limited literature
on dermatological conditions within this population.
Case Report: A 25-year-old African American female with a history
of mild hidradenitis suppurativa and asthma who presented with
asymptomatic hypopigmented rashes throughout her face, scalp, and
chest. She was diagnosed with the petaloid form SD and treated with
ketoconazole shampoo once weekly, ketoconazole cream 1-2x daily,
and hydrocortisone 2.5% ointment twice daily as needed. At six-week
post-treatment follow-up, the patient’s rashes significantly improved.
Conclusions: The petaloid form of SD is commonly experienced in
dark-skinned patients. While common treatments for SD are effective
in this form of SD, special consideration of skin types, skincare habits,
and haircare in the African American population should be explored.
This case report demonstrates how this uncommon skin condition
presents in patients of Fitzpatrick skin type V-VI and a successful
treatment course.
Abbreviations:
Seborrheic dermatitis (SD); potassium hydroxide (KOH);
human immunodeficiency virus (HIV); Venereal Disease Research
Laboratory (VDRL); hidradenitis suppurativa (HS); rapid plasma
reagin (RPR)Introduction
Skin conditions often create social and psychological distress
to patients. Seborrheic dermatitis (SD) is ranked third behind
atopic and contact dermatitis as skin conditions with potential
to impair quality of life. SD is an inflammatory disease that has a
papulosquamous morphology in areas rich in sebaceous glands
such as the scalp, face, and body folds [1]. Potential etiologies are
disruption of the skin’s microbia, Malassezia species, increased
presence of unsaturated fatty acids on the skin surface, or disruption
of the cutaneous neurotransmitters [1]. Differential diagnoses include
atopic dermatitis, psoriasis, secondary syphilis, tinea faciei, discoid
lupus, cutaneous T-cell lymphoma, sarcoidosis, and fungal infection
[1,2]. Diagnosis of SD is often made clinically by the distribution of
lesions and appearance. Dermatopathology is not necessary due to
the absence of histologic features that are exclusively characteristic
or pathognomonic of SD. However, evaluations with a potassium
hydroxide (KOH) microscopic exam of skin scrapings, swab for
microscopy/culture, histology and direct immunofluorescence, and
human immunodeficiency virus (HIV) or Venereal Disease Research
Laboratory (VDRL) serology can be helpful in differentiating the
diagnoses [1].
Treatment of seborrheic dermatitis commonly consists of topical
corticosteroids, salicylic acid, selenium sulfide, and antifungal creams
[3]. The petaloid seborrheic dermatitis frequently presents in people
with dark skin (Fitzpatrick Skin type V-VI). These lesions appear to
be polycyclic coalescing rings that are slightly pink or hypopigmented
and may form arcuate or petal-like patches [2,3]. While diagnosis of
these dermatoses is not always difficult to make, special considerations
in patients with darker skin should be acknowledged such as hair type,
hair washing frequency, and tendency for hypopigmentation [3].
There is limited literature on the petaloid form of SD that tends to be
restricted to dark-skinned individuals. We present a case of petaloid
form seborrheic dermatitis in a young African American female, who
responded well to topical antifungals and steroids.
Case Report
A 25-year-old female with Fitzpatrick skin type V-VI, and history
of mild hidradenitis suppurativa (HS), tobacco use, and asthma
presented to the clinic with asymptomatic hypopigmented rashes
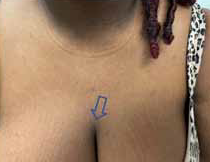
throughout her face, scalp, hairline,and chest [Figure 1,2]. She had
intermittent scaly rashes in these areas over the past 1-2 years, but
all were previously milder. The patient had no eruptions elsewhere
except for occasional Hurley Stage-1 HS inflammatory lesions in the
axilla/groin area. For her HS, she was treated with topical benzoyl
peroxide wash daily, doxycycline 100 mg daily, and clindamycin
phosphate 1% solution to inflammatory lesions daily as needed.
However, the patient reported never using clindamycin nor the
known irritant, benzoyl peroxide, on her face. Other medications
included albuterol and fluticasone inhalers. The patient had no other
medical risk factors, no known allergies, and her rapid plasma reagin
(RPR) workup was negative for syphilis. The differential diagnosis
included tinea corporis, pityrosporum (tinea versicolor), lupus
erythematosus, secondary syphilis, or the petaloid form of seborrheic
dermatitis. Histopathology of SD is usually nonspecific therefore
biopsy was not obtained. Moreover, as the eruption involved the face,
we did not wish to subject the patient to a procedure which would
result in scarring. Based on a negative KOH scraping, non-reactive
RPR syphilis test and the clinical findings, the patient was diagnosed
with the uncommon petaloid form of seborrheic dermatitis.
The patient was started on ketoconazole shampoo once weekly,
ketoconazole cream 1-2 times daily PRN, and hydrocortisone 2.5%
ointment daily. At her 6-week post-treatment follow up, the patient’s
dry scales were significantly diminished, although some areas of
hypopigmentation were still noted [Figure 3]. The patient continued
the treatment and at latest follow up (~6 months) her skin does not
demonstrate any abnormalities (not shown). This case demonstrates
an uncommon presentation of seborrheic dermatitis in a patient
with Fitzpatrick skin type V-VI that was successfully treated with
conservative topical treatments.
Figure 2: Initial presentation of patient with intramammary involvement of thin
scale on the chest (see arrow).
Discussion
Seborrheic dermatitis is a common, chronic, benign inflammatory
skin disease that affects all ethnic groups in all regions globally [1].
SD usually has a bimodal presentation, infancy and middle-age
adulthood. In adults, SD most commonly involves the face, scalp,
and chest. In children, SD usually appears in the second week of life
in areas such as face, diaper region, skin creases of the neck and the
axillae. Infantile SD is also known as cradle cap when presented on
the scalp with thick, dry, silvery or yellow scales [1]. In an overview
of the epidemiology of skin diseases in people of color, the 12 leading
dermatological diseases in African Americans or Blacks are acne
vulgaris, eczema, fungal infections, urticaria, scabies, impetigo,
seborrheic dermatitis, contact dermatitis, and verrucae vulgaris [4].
Of note, seborrheic dermatitis was also one of the most common
cutaneous diseases in the African American pediatric population
[4]. Two other reports of most common dermatologic conditions
in patients of color also indicate that seborrheic dermatitis is one of
the top five most common diagnoses in this population [5,6]. Other
research has shown that there may be a slight increase in incidences of
SD among African Americans and West Africans (2.9-6%) compared
to Caucasian skin [7]. As studies show, SD is a dermatologic concern
frequently encountered by people of color. However, a review of
dermatological textbooks found the most common skin types depicted
are Fitzpatrick types II-III [8]. By the authors’ search, there are scarce
reports of the petaloid form of SD in the published literature. The
presentation of this case will alert practitioners to this entity to allow
easier recognition of this diagnosis without having to subject the
patient to potentially scarring procedures such as a skin biopsy to
rule out other entities such as lupus erythematosus, tinea faciei, and
facial discoid dermatitis. This calls for an increased representation
and understanding of dermatological conditions in darker skin types.
Skin lesions appear in various ways in different skin types, and
thus a thorough understanding of presentations offers the most
competent care for patients of all skin types. The petaloid form of
seborrheic dermatitis is frequently associated with people with
dark skin (Fiztpatrick skin type V-VI) [2]. As seen in our patient,
the lesions appear as polycyclic coalescing rings that are light pink
or hypopigmented [3]. The hypopigmentation without scarring is
thought to result from inhibition of melanocyte tyrosinase function
and pigment production by yeast metabolites [9]. Unlike the common
presentation of scaly rashes, patients of darker skin usually do not
often show significant scale. In addition, the underlying erythema
of SD may be difficult to appreciate in darker skin [2]. Lesions on
the anterior chest and face tend to have a psoriasiform morphology
in petaloid SD, making psoriasis a common mimicking diagnosis
for petaloid SD in skin of color [1]. Annular facial dermatoses
in Fitzpatrick skin type V-VI can also closely resemble lesions of
secondary syphilis, although presence of lesions only on the face and
not a widespread eruption including the palms and soles would be
unusual [2,10]. Another interesting variant of SD presents similarly to
cutaneous sarcoidosis and is more likely to be encountered in African
American patients [11]. Cutaneous discoid lupus may progress
into hypopigmented lesions similar to petaloid SD, however, the
hypopigmentation occurs late in the chronic disease and is associated
with scarring. Majority of discoid lupus appear as erythematous,
inflamed plaques with well-demarcated hyperpigmentation at the
periphery and depressed central atrophy [12]. Fungal dermatoses,
including tinea corporis, usually present with an itchy, red rash on
the neck, trunk, or extremities. These lesions also demonstrate sharp
marginations with a raised erythematous scaly edge that may contain
vesicles. KOH preparations showing septae and branching hyphae
can confirm the diagnosis [13]. Conversely, SD rashes are commonly
flat patches without severe inflammation on the margins. The unique
dermatological presentations in patients of color can contribute
to difficulties in timely and accurate diagnosis. In our patient with
negative syphilis and fungal testing, characteristic presentation of SD
lesions, and insignificant past medical history, SD was the most likely
diagnosis and treatment was promptly started.
Treatment goals for SD is primarily to lessen visible signs and
reduce symptoms such as pruritus and erythema. Common treatment
includes over-the-counter shampoos and topical antifungals,
calcineurin inhibitors, and corticosteroids [14]. The efficacy of
ketoconazole shampoo in clearing scalp SD and dandruff and
preventing relapse has been established since the early 1990s [15]. A
more recent multicenter, double-blind, parallel group study showed
that miconazole nitrate shampoo is at least as effective and safe as
ketoconazole shampoo for treating SD in the scalp [16]. While similar
treatment may be used in skin of color, considerations of hair and
skin type, hair-washing frequency, and inappropriate oil use in people
of color may alter the outcomes of treatment [3,17]. In addition, SD
in people of color are associated with hair breakage, lichen simplex
chronicus, and folliculitis requiring careful utilization of antidandruff
shampoos. Encouraging patients to increase shampooing and decrease
use of scalp pomades and oils has been recommended [17] . Further,
chronic use of corticosteroids may exacerbate hypopigmentation
commonly seen in patients of color with SD. A pilot trial showed
1% pimecrolimus cream, a calcineurin inhibitor, as an excellent
alternative therapy for treating SD in African Americans, particularly
in those with associated hypopigmentation [18]. However, like
corticosteroids, some authors feel that calcineurin inhibitors should
only be used short-term in conjunction with antifungal shampoos
and topicals [12,19]. Seborrheic dermatitis is a chronic and relapsing
condition; therefore, prevention and prophylaxis management are
important.
Conclusion
A paucity of literature exists on the petaloid form of seborrheic
dermatitis, which is usually encountered only in dark-skinned
patients. It is important to recognize and understand the presentation
and treatment of petaloid SD seen in people of color to facilitate
culturally competent care. SD presents in dark skinned individuals
with scaly, hypopigmented macules and patches in typical areas of
involvement such as the face, scalp, hairline, beard, sternum, and
other skinfolds[3]. Uniquely, these lesions may appear annular or
petal-like, given the term petaloid SD. Petaloid SD in skin of color
may be similar to other hypopigmented skin conditions, however,
clinical judgment with thorough history should differentiate the
diseases. In rare cases, a skin scraping or biopsy may be necessary
to confirm the diagnosis or to rule out other etiologies. Treatment
for this form of SD is similar to the typical SD medications, which
includes antifungal topicals and shampoos, corticosteroids, and
calcineurin inhibitors. However, special considerations of different
skin type, skincare habits, and hair-care in this population should be
explored as these factors can affect the dermatological manifestation
and outcome for these patients. Excessive hair oil and pomade use,
and infrequent hair-washing may exacerbate SD in patients with
Fitzpatrick skin types V-VI, and should be discussed with patients.
There is a significant disproportion in the representation of darker
skin types in dermatological textbooks. This case demonstrates the
presentation of the petaloid form SD in an African American patient
to contribute to the limited literature on dermatological conditions
within this population.
Acknowledgements
The authors wish to acknowledge the financial assistance of the
Wright State University Department of Pharmacology & Toxicology.
This research was supported in part by grants from the National
Institutes of Health grants R01 HL062996 (J.B.T.), R01 ES031087
(C.A.R., J.B.T.).