Journal of Clinical and Investigative Dermatology
Download PDF
Letter to Editor
Valuing the Inpatient Dermatology Consult Service at a Single Academic Institution
Latoni D1, Kranseler J2, Cohen S2, Elliot E2, Yanovsky Dufner R2, Moody K2 and Yang FC2*
1Tufts University School of Medicine, Boston, Massachusetts, USA
2Department of Dermatology, Tufts Medical Center, Boston, Massachusetts,
USA
*Address for Correspondence:
Yang FC, Department of Dermatology, Tufts Medical Center, 260
Tremont St, Boston, MA 02116; USA, E-mail: fyang1@
tuftsmedicalcenter.org
Submission: 22 August, 2022
Accepted: 29 August, 2022
Published: 05 September, 2022
Copyright: © 2022 Latoni D, et al. This is an open access article
distributed under the Creative Commons Attri-bution License,
which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Keywords
Inpatient dermatology; Dermatology consults; Value
quantification; Hospital admissions; Cost quantification
Introduction
Despite increasing evidence that dermatology inpatient services
add significant value and cost savings to health systems [1-4],
obtaining hospital support for inpatient dermatology hospitalists can
be challenging and professional reimbursement alone is insufficient
to support the time required for this service [2-4]. We performed
a retrospective, cross-sectional cohort study to characterize the
inpatient population with skin-related conditions at Tufts Medical
Center (TMC) in Boston in order to quantify the value of inpatient
dermatologic consultations.
Our analysis included all hospital admissions at TMC in between
January 1 to December 31, 2019. Out of 17,844 inpatient admissions,
2,468 (13.8%) had one or more skin diagnoses, with 179 patients
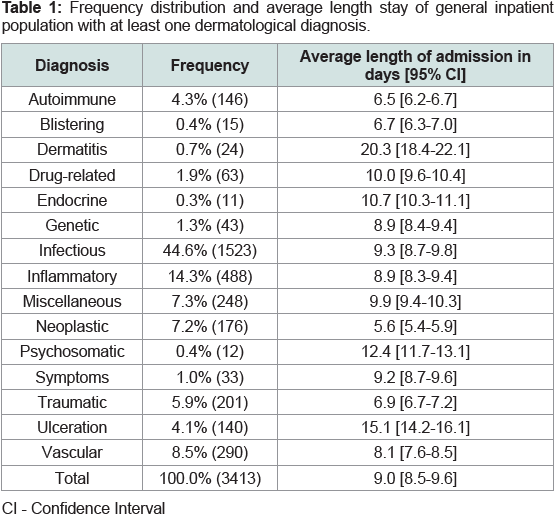
(1.0%) receiving at least one dermatology consult. Table 1 provides the
diagnostic breakdown of all coded inpatient dermatologic diagnoses.
Infectious diagnoses were the most common at 44.6% (1523), of which
51.3% (781) were cellulitis, 29.3% (446) were abscesses, and 19.4%
(296) were other infections. The mean duration of admission was 9.0
days [8.5-9.6] for patients with at least one dermatological diagnosis,
versus 5.7 days [5.5-5.8] for the entire inpatient population. The mean
admission duration of patients with dermatology consults was 11.4
days [8.2-14.5], suggesting higher complexity of disease.
Table 1: Frequency distribution and average length stay of general inpatient
population with at least one dermatological diagnosis.
The dermatology inpatient service was most consulted for
suspected infectious conditions 32.4% (59), unknown diagnoses 16.4%
(30), and inflammatory conditions 14.8% (27). Of the 19 consults for
suspected cellulitis only 7 cases (36.8%) were clinically consistent with
cellulitis. This is consistent with a previous study in which the cellulitis
misdiagnosis rate was 74% [1]. Of the 12 remaining cases admitted for
presumed cellulitis, 8 still required admission and 4 were preventable
admissions ultimately diagnosed as: dermatitis (3), and lymphedema
(1). Performing a sensitivity analysis, at an average length of stay of 5.7
days and a national mean cost of $2,607 per day of hospitalization [5],
dermatology consultation could have saved the health system $59,440
on these four preventable admissions. Savings could be as high as
$2,443,280 in 2019 at this institution if extrapolated to all inpatients
with presumed cellulitis. These savings exclude the opportunity cost
of turning away admissions given limited bed capacity. This upper
limit of savings may be an overestimation since consultation cases
may be more challenging to diagnose. Two prospective studies which
randomly evaluated cellulitis in patients, showed a mis-diagnosis
rate of 30.7-33.6% [1], translating to approximately $2.5 million in
savings.
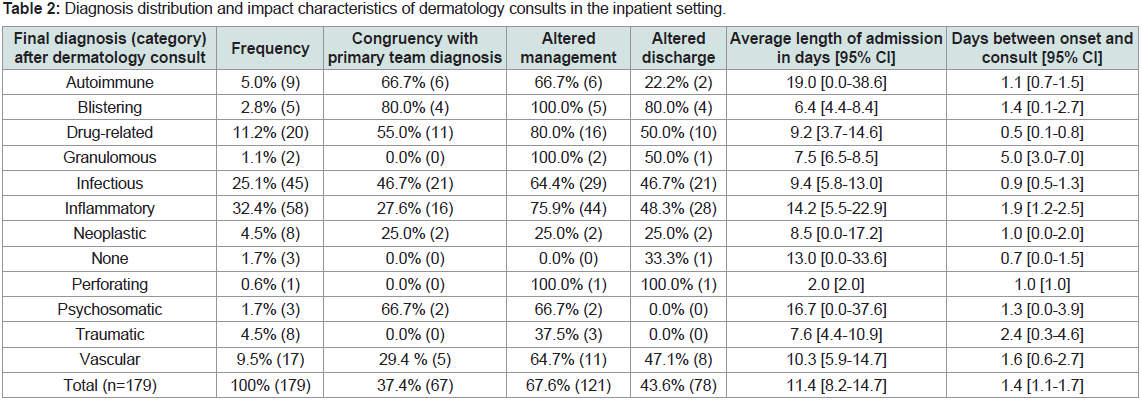
Table 2 provides the diagnosis distribution and impact
characteristics. About 62.6% of primary team diagnoses were
incongruent with dermatology team diagnoses. Dermatology consults
altered management in 67.6% of cases. On average, it took 1.4 days
[1.1-1.7] for inpatient teams to initiate a dermatology consult once a
skin condition was noticed. The average time to consult for specific
categories of dermatology team final diagnoses is presented in Table 2.
Table 2: Diagnosis distribution and impact characteristics of dermatology consults in the inpatient setting.
The results of this study show the significant impact dermatology
consults can have on hospital admissions, from changes in
management to avoidance of hospitalization altogether. Furthermore,
these demonstrated cost savings justify hospital funding of dedicated
inpatient dermatology consultative services that otherwise would be
difficult to sustain through professional billing services alone.