Journal of Clinical and Investigative Dermatology
Download PDF
Research Article
Inter- and Intra-Physician Variation in Quantifying Actinic Keratosis Skin Photodamage
Schmeusser B1, Borchers C1, Travers JB1,3,5, Borchers S3, Trevino J3, Rubin M3, Donnelly H3, Kellawan K3, Carpenter L3, Bahl S3, Rohan C3, Muennich E3, Guenthner S5, Hahn H3, Ali Rkein3, Darst M6, Mousdicas N7, Cates E1, Sunar U2 and Bihl T1,2*
1Department of Pharmacology & Toxicology, Boonshoft School of Medicine, USA
2Department of Biomedical, Industrial & Human Factors Engineering, USA
3Department of Dermatology, Boonshoft School of Medicine, USA
4Dayton Veterans Administration Medical Center, USA
5The Indiana Clinical Trials Center, PC, USA
6Charlotte Dermatology, Charlotte, USA
7Richard L. Roudebush VA Medical Center, Indianapolis, USA
*Address for Correspondence: Bihl T, Department of Pharmacology & Toxicology, Boonshoft School of Medicine, Wright State University, Dayton, OH, 45435, USA, Fax: 937-775-7221, Tel: 937-775-2463, Email: trevor.bihl@wright.edu
Submission: 19 August, 2020;
Accepted: 1 September, 2020;
Published: 6 September, 2020
Copyright: © 2020 Schmeusser B, et al. This is an open access article
distributed under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
Abstract
We investigated the variations in physician evaluation of skin photodamage
based on a published photodamage scale. Of interest is the utility of a 10-level
scale ranging from none and mild photodamage to actinic keratosis (AK). The
dorsal forearms of 55 adult subjects with various amounts of photodamage were
considered. Each forearm was independently evaluated by 15 board-certified
dermatologists according to the Global Assessment Severity Scale ranging from
0 (less severe) to 9 (the most progressed stage of skin damage). Dermatologists
rated the levels of photodamage based upon the photographs in blinded fashion.
Results show substantial disagreement amongst the dermatologists on the severity
of photodamage. Our results indicate that ratings could be more consistent if
using a scale of less levels (3-levels). Ultimately, clinicians can use this knowledge
to provide better interpretation of inter-rater evaluations and provide more reliable
assessment and frequent monitoring of high-risk populations.
Keywords
Rating scale; Dermatology; Rater reliability; Rctinic
damage; Kappa; Physician variation
Abbreviations
AK: Actinic Keratosis; BCC: Basal Cell Carcinoma; CV: Coefficient
of Variation; CI: Confidence Interval; FFPAS: Dermatologic
Assessment Form Forearm Photographic Assessment Scale; NMSC:
Non-Melanoma Skin Cancer; SCC: Squamous Cell Carcinoma; UV:
Ultraviolet
Introduction
Non-melanoma skin cancers are the most common form of
malignancy within North America, whose prevalence is only rising
with nearly 3.5 million cases diagnosed within the United States
alone each year. This is associated with a substantial financial impact,
currently estimated at $5 billion to treat non-melanoma skin cancers
(NMSCs), including basal cell carcinomas (BCCs) and squamous
cell carcinomas (SCCs) [1]. Major causes of skin pathologies are
exposure to ultraviolet (UV) radiation, commonly from sunlight and
artificial sources such as tanning beds. The term actinic neoplasia
is used for AKs and NMSC to denote the role of UV and advanced
age. Skin pathologies related to photodamage include precancerous
actinic keratosis, which can progress into basal cell carcinoma and
squamous cell carcinoma.
Although classified as pre-cancerous, AK progression to NMSC is
variable. A majority of NMSC arises from AKs, but a majority of AKs
do not become cancer or will even be clinically present in 1-5 years [2].
Most AKs are diagnosed clinically, yet the current gold standard for
diagnosis of an AK is a classified as an invasive procedure, involving
a biopsy of the lesion with subsequent histopathology [3]. NMSC are
diagnosed by histology.
Given the considerable morbidity and occasional mortality
associated with actinic neoplasia, strategies including use of
cyclooxygenase-2 inhibitor celecoxib [4] and nicotinamide [5] have
been tested. To assess risk factors for actinic neoplasia, as well
response to rejuvenation techniques, there is a need for a reliable
method to evaluate photodamage. In particular, presence of
photodamage is strongly associated with actinic neoplasia. One of
the primary methods for quantifying photodamage is the 10-point
Dermatologic Assessment Form Forearm Photographic Assessment
Scale (FFPAS) of [6].
Recent studies have suggested that noninvasive imaging of skin
could detect and monitor precancerous lesions using hemoglobin
contrast [7]. However, complicating both manual and computer
detection of AKs, is the complexity of the FFPAS evaluation
mechanism. In performing a clinical trial (N=55 subjects; 110 dorsal
forearms; N=15 physicians), we noticed significant disagreement
across diagnoses. Such disagreements in the community, if realized
through conflicting second opinions, could result in some receiving
overly aggressive treatments while others receive insufficient
treatment. In this paper, we examine these results and pose various
suggestions to improve the FFPAS process.
Materials and Methods
A clinical trial was performed on subjects who are patients in
the Wright State University Department of Dermatology clinics.
This was performed under an institutional review board-approved
protocol, and informed consent was obtained from all the patients before the measurements.
Selection of patients and photos:
The patients were 35 years old or older with “fair” skin (Fitzpatrick
scale I or II) [8] and did not have recent (< 6 month) history of use
of a tanning bed/significant sun exposure. A total of 55 subjects were
recruited and these subjects expressed various levels of photodamage,
including clinically-apparent AKs. Each subject had each of their
forearms photographed, resulting in a total of 110 photos of arms to
be evaluated. Examples of a forearm exhibiting mild, moderate, and
severe photodamage is shown in Figure 1.Selection of raters and rating process:
Each forearm was evaluated for photodamage by board-certified
dermatologists (N=15 physicians) trained in evaluating actinic
damage. This group consisted of dermatologists from both academic
(4) as well as private practice (11) backgrounds who had a minimum
of 5 years of post-residency experience. For evaluation in this study,
the dermatologists used the 10-point FFPAS of McKenzie et al. (2011)
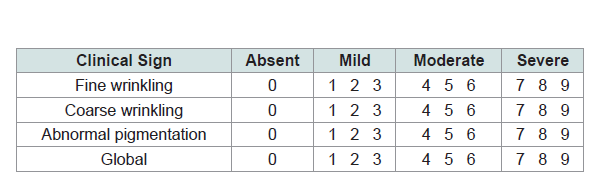
[6]. As shown in Table 1, FFPAS is a subjective measure to examines
clinical signs of UV-induced skin damage along four dimensions: fine
wrinkling, coarse wrinkling, abnormal pigmentation, and a global
assessment [6]. In using the FFPAS approach, each individual clinical
sign is scored, and a global assessment is provided to rank the overall
actinic damage [6].Dermatologists in this study were trained in FFPAS by reviewing
the examples in the published McKenzie scale [9]. Once trained,
the dermatologists individually, independently, and separately
evaluated each arm of participants from a PowerPoint presentation of
photographs which consisted of not only the 110 forearms from the
55 subjects, but an additional 20 forearm pictures duplicated to assess
intra-rater reliability. The raters provided the global assessment
for each arm. No identification of the patient, arm, or initial
assessment was provided and the arms were randomly organized
in their presentation. Each dermatologist was also given unlimited
time for assessment. The raters were blinded to clinical information
and the source of the photos, and were not allowed to discuss their
observations with other raters.
Down Sampling Ratings:
Travers et al. [7] down sampled, or pooled, the 10 FFPAS categories
into three groups (Mild/none, Moderate, and Severe). Notionally, these 3 down sampled groups followed the general groupings of
Table 1, where scores of 0, 1, 2, and 3 are mild, scores of 4, 5, or 6 are
moderate, and scores of 7, 8, and 9 are severe. Consistent with [7],
scores of 0 are grouped into mild due there being few observations of
0 in the study. These groups were in the implicit groupings of Table 1 and were used in [7] to develop a three-class machine learning
classifier for actinic damage classification. This down sampled FFPAS
scores are used herein to understand how different multitudes of
ratings might affect rater reliability.Statistics:
The data was analyzed using JMP (SAS), Matlab 2019a a (Mathworks, Boston, MA) and the Fleisses Kappa software package in Matlab [10]. Inter- and intra-rater reliability was assessed using
coefficient of variation (CV) [11], Fleiss’s κ [12], Cohen’s κ [13], and graphical means. For any confidence interval (CI) or hypothesis test,
α = 5% was used.The CV between each dermatologist for each of the arms rated
with the equation:
CV=s/x
which scales the sample variance for a given arm by the sample
mean [11]
Intra-rater reliability was analyzed using Cohen’s κ [13]. The
κ values were calculated for each dermatologist for their assessment
of the 20 duplicated samples. Inter-rater reliability was analyzed
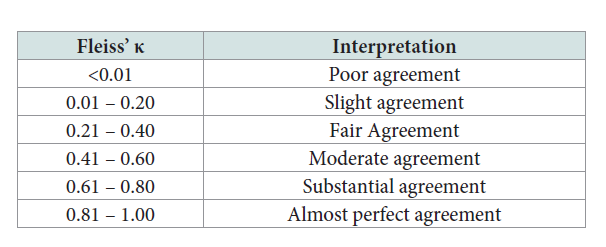
using Fleiss’s κ [12], an extension of Cohen’s κ. In addition to the
confidence intervals and hypothesis tests of both methods, κ has a
further interpretation with general hierarchy of [14], seen in Table 2.
Results
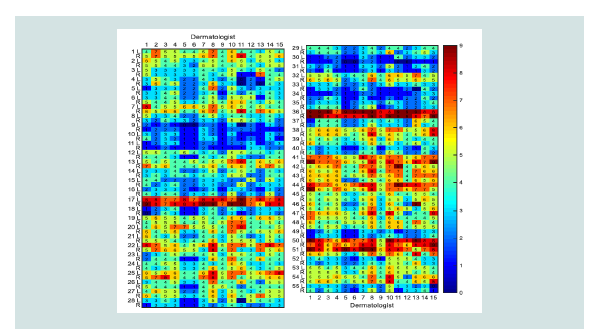
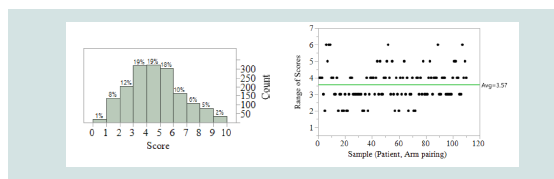
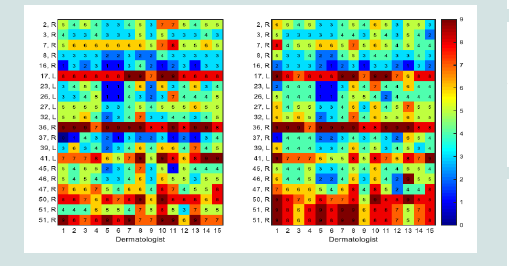
The results from this study are presented in Figure 2 which presents
a heat map where subjects are the rows and the rating dermatologists
(consistent throughout this study) are the columns. Two rows are
presented for each subject, for left (L) and right (R) arms. The colors
in Figure 2 range from blue, for 0, to red, for 9. The scores are further
provided in each cell for the rating each dermatologist gave a specific
arm. While, overall, scores tended towards the middle values (Figure 3a), it is visually apparent in Figure 2 that some subjects generally
have more severe actinic damage than others. Considering the range
of scores by each patient-arm pairing, Figure 3b, it is further apparent that there is general disagreement by raters. An example illustrates
this disagreement using patient 1’s left arm; in row 1 of Figure 2 we
see scores ranging from 3 (mild), by dermatologist 13, to 7 (severe),
by dermatologists 2 and 8, giving a range of 4, as seen in Figure 3b.
Collectively, Figure 3b illustrates the general differences in diagnosis
with a mean range of 3.57 across all arms in this study. Since each of
the groups of FFPAS (Mild, Moderate, Severe) encompass 3 scores,
the average range of scores in this study indicates very different
diagnoses were given for each arm (e.g. Mild to some, Moderate to
others). Similarly, this could possibly result in the prognosis would
greatly changing for a subject, for example, depending on which
dermatologist a subject would visit.
Figure 2: Physician scores (0-9) associated with each arm, numbers along
rows indicate patient number along with left (“L”) or right (“R”) arm. Columns
indicate which physician evaluated the patient. Colors and numbers in each
cell are the score given.
Table 1: The Dermatologic Assessment Form Forearm Photographic
Assessment Scale (FFPAS) of McKenzie et al. (2011) [6]
Table 2: General interpretation of κ [14].
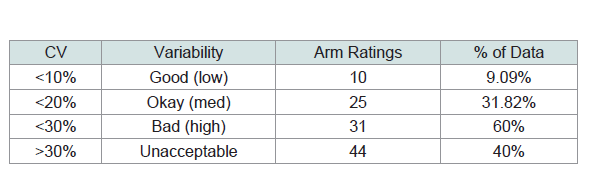
Inter-rater reliability:
The inter-rater reliability was overall slight for the data in Figure 2
(κ = 0.114, CI 0.111-0.116). For the hypothesis that the raters provide
equal ratings, the null was rejected at a 5% level of significance with
P < 0.001. Using the hierarchy of [14] in Table 2, we would find that
there is only slight agreement between raters. Considering the CV,
we further see a high degree of variability between the dermatologists.
Utilizing a maximum acceptability CV of 10% (good/low variability)
only 4/110 ratings of the patient arms studied by the 15 dermatologists
met criteria. If utilizing a maximum acceptability CV of 20% (okay/
medium variability), still only 18/110 of the rating of the patient arms
by the dermatologists met criteria. A CV of less than 30% (bad/high
variability) represented 59/110 ratings. The remaining 51/110 ratings
had CV greater than 30%, indicating unacceptable variability. Overall,
80.1% of the CV met standards of high-unacceptable variability.
These results can be summarized below in Table 2.Intra-rater reliability:
The intra-rater reliability differed heavily by dermatologist, as
visualized by the heatmap in Figure 4. Overall, 20 arm pictures were
repeated and provided in the study with one arm given three times.
The heatmap in Figure 4a show ratings for the repeated images and
the heatmap in Figure 4b provides the original values from Figure 2
for direct comparison. Arm 51 right is listed twice in Figure 4b to aid
comparison against Figure 4a as arm 51 right as dermatologists rated
this arm 3 times. Figure 4 is evaluated by comparing columns in 4a
to columns in 4b to look for consistency; for example, dermatologist
1 frequently did not rate consistently whereas dermatologist 6 almost always provided the same rating. Evaluating the intra-rater reliability
with Cohen’s κ found the mean intra-rater reliability to be moderate
(κ=0.473, 95% CI 0.377-0.570).Down Sampling Rating:
With the three down sampled groups, the dermatologists had
moderate agreement (κ = 0.41, 95% CI 0.3968-0.4060 Examining the
CV for this grouping, we find the results in Table 3 which illustrate
that the overall variability is much lower (45.5% of patients getting
highly variable results versus 83.7% before) when using the down
sampled rating scale. Intra-rater reliability for the down sampled
ratings was found to have substantial agreement (κ=0.753, 95% CI
0.684 - 0.823).Discussion
Assessment of dermatological conditions is often highly
subjective in nature and the result of the complex interaction
between standards, experience, training, personalities, as well as
patient medical histories and overall health. Thus, understanding
the severity of actinic damage is a challenge in daily clinical practice.
Such challenges are exacerbated as telemedicine increases in use
for triage [15] with photography-based prerounds recommended
for dermatological assessment [16]. Although the Form Forearm Photographic Assessment Scale (FFPAS) [6] is used clinically in
actinic damage assessment, to the best of our knowledge, its interand intrarater reliability has never been determined.
Table 3: Results from coefficient of variation analysis of dermatologist ratings.
Results indicate a high variability/CV, with 19.9% of the data having Okay to
Good (low) variability.
Figure 3: (left) Physician clinical scores of skin damage. (right) Range of
scores from dermatologists. From (Travers, et al., 2019) [7].
Figure 4: Physician scores (0-9) associated with each arm for (left) repeated
samples with second/third look and (right) for the original ratings from Figure 2. Numbers along rows indicate patient number along with left (“L”) or right
(“R”) arm. Columns indicate which dermatologist evaluated the patient. Colors
and numbers in each cell are the score given. Notably, subject 51’s right arm
was examined 3 times by all dermatologists (2 repeated evaluations). The
original scores for 51, R is repeated twice in b) to facilitate readability.
Table 4: Results from coefficient of variation analysis of dermatologist ratings
with a revised FFPAS for 3 levels only. Results indicate lower variability/CV than
with 10 levels, with 31.8% of the data having Okay or Good (low) variability.
This study considered FFPAS in a clinical study of N=55 patients
and ND = 15 board certified dermatologists. To evaluate these results,
the authors used both graphical and statistical methods. Graphical
heat maps were used to visualize the ratings of dermatologists by
sample and kappa statistics were used to evaluate inter- and intra-rater
reliability. As noted in [17], heatmaps are seldom used to visualize
patient data across repeated visits despite their value in visualizing
patient progress; the work presented herein illustrates the value of
heatmaps for similar purposes, including high-level assessment of
agreement by an external observer.
When considering the 10 level FFPAS scoring, the authors found
slight inter-rater agreement and moderate intra-rater agreement by
dermatologists in the FFPAS ratings, which were both on the lower
side of rater reliability assessment. The result of such a problem
is that severe actinic damage could go untreated if rated low by a
dermatologist. This is a recurring phenomenon in dermatology
due to the subjective nature of some aspects and the fact that every
dermatologist has varying amounts of experience and clinical
expertise.
In addition to the standard 10 levels of FFPAS, the authors
further down sampled the ratings into 3 groups, the mild, moderate,
and severe high level groups of [6] as used in the prior work of [7].
When considering the down sampled groups, we found moderate
interrater agreement and substantial intrarater agreement, both an
improvement over the 10 levels of FFPAS.
While studies suggest that there is no optimal number of levels in
a Likert-like questionnaire [17,18] and FFPAS is consistent with such
recommendations, the results indicate the possibility that FFPAS has
too many levels. Thus, it appears that more consistent results would
be possible with a simpler, i.e. less levels, assessment scale.
The authors do acknowledge some limitations in this study.
The selection of pictures may have not represented all possible
actinic damage conditions seen in clinical practice; additionally,
these pictures do not precisely represent the normal anatomical
distribution [19]. The authors were also unable to collect the mean
time the raters spent on completing the questionnaire since this was
emailed to participants. Additionally, while the authors illustrated
some benefit in both inter- and intra-rater reliability using a down
sampled FFPAS scoring system, this study did not query the
participating dermatologists on using a revised scale, the authors
cannot definitively say that FFPAS scoring with 3 scales is better, but
such a simplification warrants further study.
Acknowledgement
Ohio Third Frontier to the Ohio Imaging Research and Innovation Network
(OIRAIN) 667750 (US); National Institutes of Health ES020866 (JBT),
AG048946 (JBT); and Veteran’s Administration Merit Awards 5I01BX000853
(JBT) and 1101CX000809 (JBT).