Journal of Clinical and Investigative Dermatology
Download PDF
Research article
Successful Treatment of Post Herpetic Neuralgia and Herpes Zoster (Shingles) with Homeopathic Medicines
Swami Shraddhamayananda*
- Ramakrishna Mission Charitable Dispensary, Belur Math, Howrah, WestBengal, India
*Address for Correspondence: Swami Shraddhamayananda, Ramakrishna Mission Charitable Dispensary,Belur Math, Howrah, West Bengal, India, Tel: 91- 9143415986; E-mail: gopalmj.belurmath@gmail.com
Citation: Shraddhamayananda S. Successful Treatment of Post Herpetic Neuralgia and Herpes Zoster (Shingles) with Homeopathic Medicines. J ClinInvestigat Dermatol. 2017; 5(1): 4.
Copyright: © 2017 Shraddhamayananda S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & InvestigativeDermatology| ISSN: 2373-1044 | Volume: 5, Issue: 1
Submission: 06 March, 2017| Accepted:25 March, 2017 | Published: 06 April, 2017
Submission: 06 March, 2017| Accepted:25 March, 2017 | Published: 06 April, 2017
Abstract
Herpes Zoster (HZ) is a viral disease resulting from the reactivation of Vericella Zoster virus (VZV) which remains latent in the nerve ganglion after primary infection. The commonest complication of HZ is Post herpetic neuralgia (PHN). When the body immunity goes down then the latent VZV become active in the sensory ganglia and causes inflammatory neural damage which subsequently leads to the incidence of PHN and acute neuralgic pain. Both the central and peripheral nervous system are affected. But the intensity of suffering of this disease is less in children than in adults. Incidence of PHN is common in elderly persons and is a serious problem to them with sleepless nights (insomnia) that may persists several years. There is no definite consensus on the definition of PHN but in the latest studies it is defined as pain persisting more than 3 months after the rash has healed.
In this study we treated 100 HZ cases of different age and sex; with homeopathic medicines (Rhus tox & Thuja oc.) but no one developed PHN after one to six months of follow up and in all patients rashes or lesions were healed within 8-12 days, which may indicate the positive role of these medicines to prevent PHN. The results of this study were very encouraging indicating a definite role of homoeopathic medicine in HZ and PHN.
Keywords
Herpes zoster; Homeopathy; Post herpetic neuralgia
Introduction
HZ is commonly characterized by unilateral painful vesicles in the affected dermatome of the respective sensory ganglion. PHN is a common complication of HZ. PHN can last several years, and is the most common sequel of HZ [1,2]. The frequency of PHN has been reported to be from 10% to 34% depending on its definition [1,2]. If PHN is defined as persistent pain three months after the onset of the HZ rash, the incidence of PHN is 10% to 20% [2,3]. The quality of life of patients experienced by patients with PHN can be negatively affected not only by the pain, but also by comorbid conditions such as atigue and insomnia, and decreased social activities [4,5]. The true incidence of PHN is difficult to establish and depends partly on the definition used. Data from a number of studies indicate that 5 to 57 per cent of patients have pain persisting for one month or more [6] and that incidence increases with advancing age[7,8].
The pathophysiology of PHN is not well understood. But it is clear that HZ affects the central and peripheral nervous systems, particularly when body vitality goes down, the latent VZ virus become active in the sensory ganglia and leads to inflammatory neural damage that subsequently lead to the occurrence of PHN and acute zoster pain. Sometimes motor paresis may occur due to the spread of infection and inflammation from the dorsal horn to the anterior horn [9].
Although many clinicians have tried to distinguish acute herpetic neuralgia from chronic herpetic neuralgia, there is no definite consensus on the definition of PHN. However, from the recent studies, it appears valid to define three phases of pain following HZ: (1) acute herpetic neuralgia, defined as pain that occurs within a month after the onset of rash; (2) subacute herpetic neuralgia, defined as pain that occurs from the acute phase of HZ to the chronic phase of PHN; and (3) PHN, defined as pain that persists beyond three months after rash appearance. It was found that PHN that continues six months after the onset of rash is more likely to be obstinately persistent for severalyears [10,11].
The patients usually complain burning sensation and redness at the site of the lesion followed by skin eruption or rash and pain along the course of the nerve.
The well-defined risk factors for PHN in patients with HZ include older age, the presence of prodromal pain, the extent and severity of rash, and the severity of acute HZ pain [12].
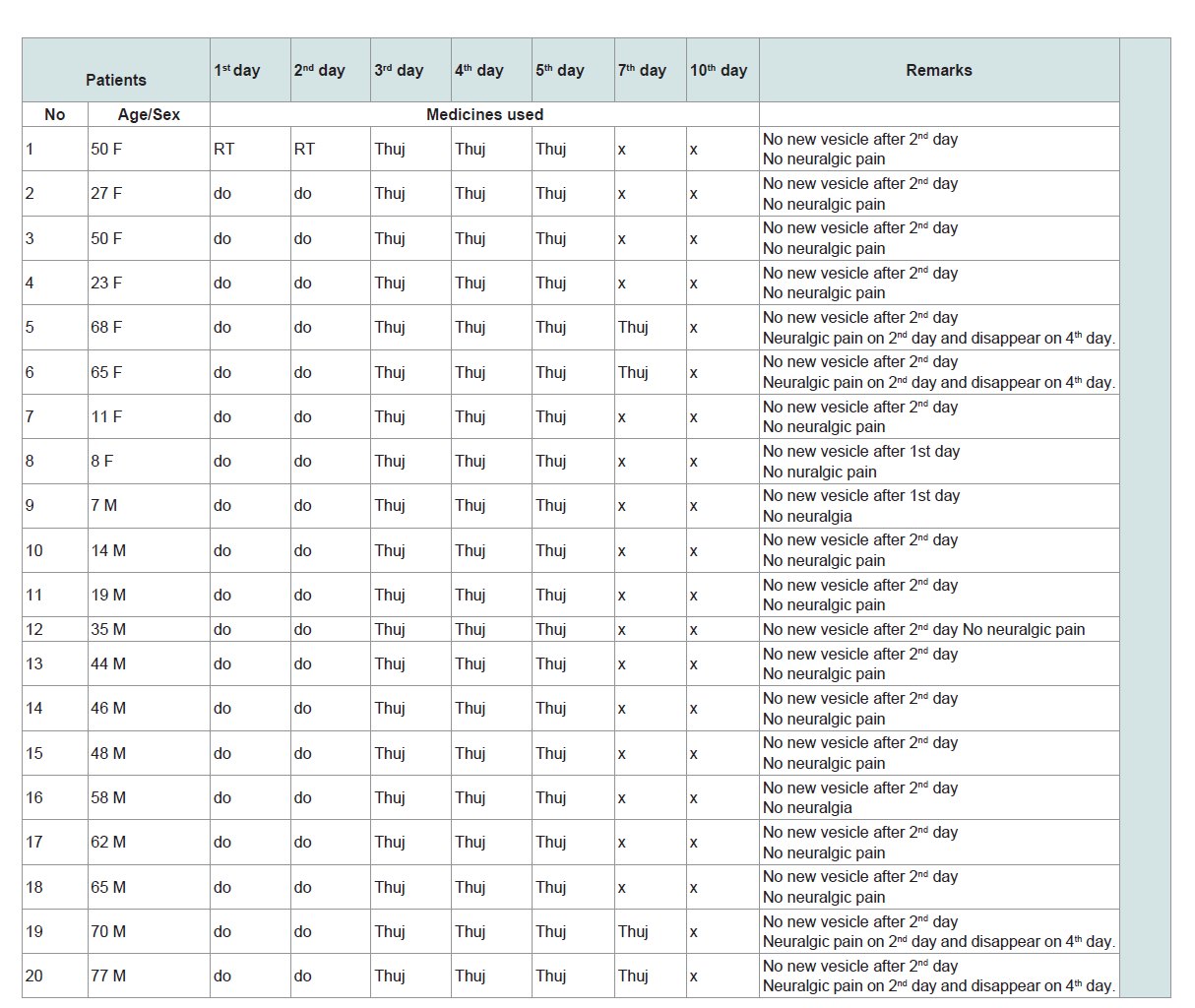
In our clinic, while treating Chicken pox patients, we have seen Rhus tox and Thuja oc. were very much effective medicine in Chicken pox to control pain and inflammation quickly, and prevent secondary infection. Then we thought that these drugs may be helpful for treatment of HZ and PHN. With this knowledge, we did first a pilotstudy with 20 Herpes Zoster patients (as the same virus is responsible for Chicken pox and Herpes Zoster) with these two drugs and the result was excellent. Then we planned a master study with 100 HZ patients who were treated with homeopathic medicines, along with a separate group of 20 cases (which we called as placebo group in the main experiment) who were treated with allopathic medicine in the same clinic (Table 1andTable 2). Details of our findings are given in the following sections.
Table 1:Result of the pilot study with 20 patients, the final experiment was based on the result of this pilot study.
Materials and Methods
The patients
Total 100 patients were enrolled in this study of different age, sex and religions. Only gravid mothers were excluded in this study. Male:Female ratio was ~1.2:1. The patients were selected from the general patients attending our dermatology clinic. They were diagnosed, categorized and followed up by our Dermatologist of theInstitution. The patients were enrolled after taking consent either from the patients or from their parents. Permission of this study was also taken from Ethical Committee of the Institute. All dermographic records of the patients were maintained after the final diagnosis byour dermatologist when the patients were enrolled for the study. Allpatients were instructed to attend the clinic daily for 7 days and thentwice in a month for six months.
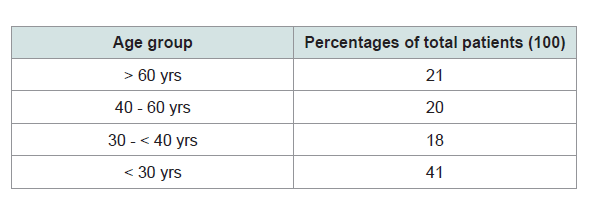
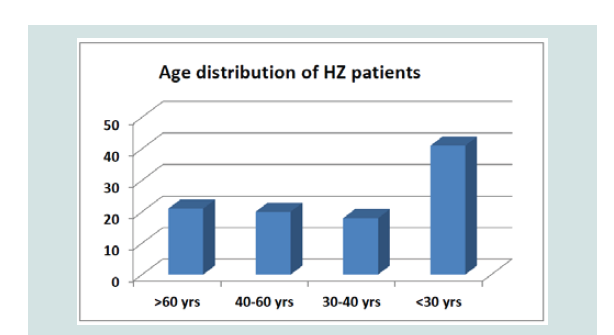
To include placebo group was considered as unethical by our Ethical Committee, so we recorded and followed up side by side the patients who were treated with allopathic medicine (Acyclovir and other allopathic medicines) in the same clinic which we considered as control study. Total 20 patients were enrolled in this group (male 14, female 6; > 60 yrs - 14; 30-60 yrs - 6) (Figure 1).
Treatment (the homeopathic medicines):Only two medicines (Rhus Tox. 1000 and Thuja Oc. 1000) were used in this study and they were given following the results of our pilot study with 20 patientswhich are given in the result section. The same medicines were given to all the patients except the control group. For first two days Rhus Tox 1000 was given one drop orally twice a day for body ache and pain and to control inflammation. No more new vesicles appeared after 48 hrs of taking Rhus Tox. Then on the following days Thuja 1000 was given one drop daily for 3 to 4 days to prevent secondary infection and for quick healing. Only single oral homeopathic medicine was used for all patients, at a time, without any local application. The other group who were treated with Allopathic medicines in the samehospital by our dermatologist.
Result and Discussion
Results of Pilot study-Detailed of this pilot study with resultsare given in Table 1.
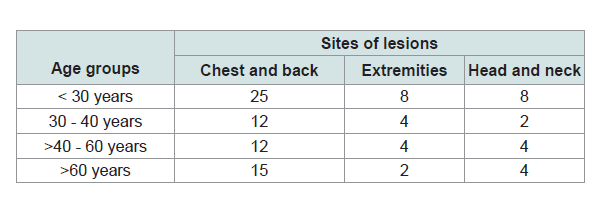
Affected parts of the patients
Most of them presented with lesion in thorax (chest+back),extremities, face and neck, given in Table 3.
Outcome of the final study
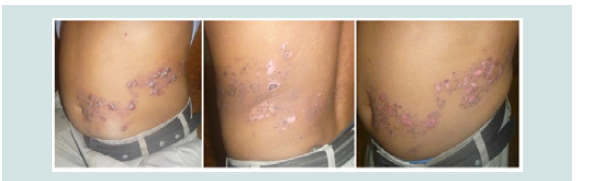
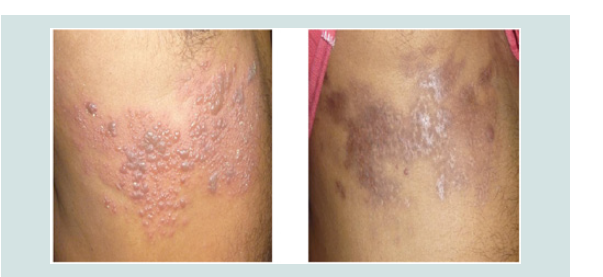
In almost all the cases after giving Rhus Tox, within 24 hrs, all the vesicles comes out and no new vesicles seen after 48 hrs of treatment. The body pain and inflammations were reduced and the vesicles were dried up within 4-6 days of starting treatment. Few of them noticed severe neuralgic pain, 2-3 day after the onset of irruption and pain disappear with the same medicines in most of the cases within 2-3 days and only in two cases pain continued. All were cured within 8-10 days (Figure 2andFigure 3). Only two patients felt PH neuralgic pain after one to six months of follow up.
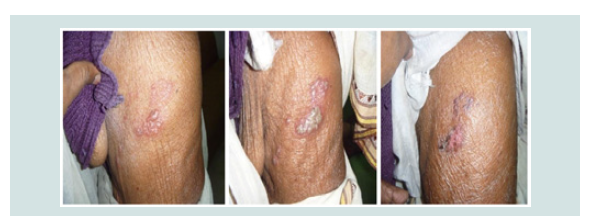
Those who were taking allopathic medicines under theDermatologist of the same clinic, out of 20 patients only 4 patients hadno symptoms of PHN of which one > 60 yrs and the remaining threewere below 50 yrs. In 4 cases pain persisted over one year (in spiteof analgesic/corticosteroid therapy and neural block). All the vesiclesdried up within 7 days and no more new vesicles appeared after 4 daysof starting treatment. But all 16 patients felt severe neuralgic painafter 5-7 days of irruption and it continued over 6 months (Figure 4-Figure 6). Many had sleepless night.
Discussion
The incidence of PHN increases with increasing patient age. Earlydiagnosis of HZ and treatment with antiviral medications decreasesthe risk of PHN. Post herpetic neuralgia is very difficult to treat.Even with the use of a variety of medications and referral to a painspecialist, pain relief may be incomplete.
Allopathic treatment of HZ include antiviral agents (such as acyclovir, famciclovir, and valacyclovir), analgesics, corticosteroids, and neural blockade (Interventional treatments like nerve block, spinal cord stimulation). The primary importance of treatment is to prevent PHN. Antiviral agents such as acyclovir, famciclovir, and valacyclovir have been shown to reduce acute HZ pain, speed lesion healing, and prevent the occurrence of PHN. Based on the results of clinical trials, antiviral therapy should be initiated within 72 hours of the skin eruption [13-15] in patients with neurological complications, good results were also found even when it is initiated beyond 72 hours of rash onset[15,16]. We have seen in this study that early start of antiviral medicine reduces the incidence of PHN even in the patients above age of 60 yrs.
Though vaccination with live attenuated VZV can prevent or reduce the incidence of HZ and PHN, but it is contraindicated in pregnant women and immunocompromised individuals and not yet widely used in developing country.
Conclusion
The result of this study is very encouraging. Out of 100 HZpatients only two patients noticed severe neuralgic pain even afterone month of treatment which continued over 6 months. Thistreatment is equally useful in children below the age of 10 and alsoin immunocompromised persons as there are no known side effectsof these medicines. Thus this method of treatment may prevent postherpetic neuralgia.
The real mechanism of action of these homeopathic medicines isvery difficult to explain and so far there is no definite explanation ofthe mechanism of action of these medicines, but these results aftertreatment proved that it works well. Thus possible attempts should bemade in future studies to find out the mechanism. This preliminaryreport may help the suffering humanity at large.
Acknowledgements
I hereby acknowledge the President, Ramakrishna Mission forgiving me permission to publish this paper. I also thank all doctorsand paramedical staff of our Medical Unit for helpful suggestions
References
- Gauthier A, Breuer J, Carrington D, Martin M, Rémy V (2009) Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect 137: 38-47.
- Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, et al. (2007) A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 82: 1341-1349.
- Arvin A (2005) Aging, immunity, and the varicella-zoster virus. N Engl J Med 352: 2266-2267.
- Thyregod HG, Rowbotham MC, Peters M, Possehn J, Berro M, et al. (2007) Natural history of pain following herpes zoster. Pain 128: 148-156.
- Yawn BP, Gilden D (2013) The global epidemiology of herpes zoster. Neurology 81: 928-930.
- Schmader KE, Studenski S (1989) Are current therapies useful for the prevention of postherpetic neuralgia? A critical analysis of the literature. J Gen Intern Med 4: 83-89.
- Burgoon CF, Burgoon JS, Baldridge GD (1957) The natural history of herpes zoster. JAMA 164: 265-269.
- DE Moragas JM, Kierland RR (1957) The outcome of patients with herpes zoster. AMA Arch Derm 75: 193-196.
- Chernev I, Dado D (2013) Segmental zoster abdominal paresis (zoster pseudohernia): a review of the literature. PM R 5: 786-790.
- Dworkin RH, Gnann JW Jr, Oaklander AL, Raja SN, Schmader KE, et al. (2008) Diagnosis and assessment of pain associated with herpes zoster and postherpetic neuralgia. J Pain 9(1 Suppl 1): S37-S44.
- Arani RB, Soong SJ, Weiss HL, Wood MJ, Fiddian PA, et al. (2001) Phase specific analysis of herpes zoster associated pain data: a new statistical approach. Stat Med 20: 2429-2439.
- Coen PG, Scott F, Leedham-Green M, Nia T, Jamil A, et al. (2006) Predicting and preventing post-herpetic neuralgia: are current risk factors useful in clinical practice? Eur J Pain 10: 695-700.
- Shafran SD, Tyring SK, Ashton R, Decroix J, Forszpaniak C, et al. (2004) Once, twice, or three times daily famciclovir compared with aciclovir for the oral treatment of herpes zoster in immunocompetent adults: a randomized, multicenter, double-blind clinical trial. J Clin Virol 29: 248-253.
- Shen MC, Lin HH, Lee SS, Chen YS, Chiang PC, et al. (2004) Double-blind, randomized, acyclovir-controlled, parallel-group trial comparing the safety and efficacy of famciclovir and acyclovir in patients with uncomplicated herpes zoster. J Microbiol Immunol Infect 37: 75-81.
- Sampathkumar P, Drage LA, Martin DP (2009) Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc 84: 274-280.
- Espy MJ, Teo R, Ross TK, Svien KA, Wold AD, et al. (2000) Diagnosis of varicella-zoster virus infections in the clinical laboratory by LightCycler PCR. J Clin Microbiol 38: 3187-3189.