Journal of Clinical and Investigative Dermatology
Download PDF
Research Article
*Address for Correspondence: Shang I Brian Jiang, MD, Department of Dermatology, University of California, San Diego, CA, USA, Tel: 858-657-8322; E-mail: bjiang@ucsd.edu
Citation: Loh TY, Rubin AG, Jiang SI. A Survey of Timeframe Variations for the Management of Early Stage Melanoma among Dermatology Residency and Procedural Dermatology Fellowship Training Programs in the United States. J Clin Investigat Dermatol. 2016;4(2): 4.
Copyright © 2016 Loh TY, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Investigative Dermatology | ISSN: 2373-1044 | Volume: 4, Issue: 2
Submission: 18 April, 2016| Accepted: 30 June, 2016 | Published: 04 July, 2016
Reviewed & Approved by: Dr. Taihao Quan, Department of Dermatology, University of Michigan, USA
On the other hand, for stage 1A tumors, two weeks was the most common recommended time period (43.8% of all programs, n=28), followed by four weeks (28.1%, n=18), one week (10.9%, n=7), three weeks (4.7%, n=3), and 1-3 days (1.6%, n=1). However, when GD and PD responses were analyzed separately, we found that the most common treatment timeframe recommended by GD program directors was two weeks (55.3%, n=21), while the time period used by most PD programs was four weeks (34.8%, n=8). However, this did not reach statistical significance.
A Survey of Timeframe Variations for the Management of Early Stage Melanoma among Dermatology Residency and Procedural Dermatology Fellowship Training Programs in the United States
Tiffany Y Loh1, Ashley G Rubin2 and Shang I Brian Jiang3*
- 1University of California, San Diego School of Medicine, CA, USA
- 2Carlsbad and Vista Dermatology, Vista, California, USA
- 3Department of Dermatology, University of California, San Diego, CA, USA
*Address for Correspondence: Shang I Brian Jiang, MD, Department of Dermatology, University of California, San Diego, CA, USA, Tel: 858-657-8322; E-mail: bjiang@ucsd.edu
Citation: Loh TY, Rubin AG, Jiang SI. A Survey of Timeframe Variations for the Management of Early Stage Melanoma among Dermatology Residency and Procedural Dermatology Fellowship Training Programs in the United States. J Clin Investigat Dermatol. 2016;4(2): 4.
Copyright © 2016 Loh TY, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Investigative Dermatology | ISSN: 2373-1044 | Volume: 4, Issue: 2
Submission: 18 April, 2016| Accepted: 30 June, 2016 | Published: 04 July, 2016
Reviewed & Approved by: Dr. Taihao Quan, Department of Dermatology, University of Michigan, USA
Abstract
Background: Early excision of melanomas while tumors are still superficial stage 0 or 1A) is critical. No recent studies have established a maximum recommended time period between diagnosis andexcision of these tumors. Thus, it is helpful to learn about typical timeframes recommended by general dermatology (GD) and procedural dermatology (PD) teaching rograms in the United States (US).Objective: To evaluate patterns in treatment timeframes recommended and employed by American GD and PD programs for stage 0 and 1A melanomas.
Methods: Anonymous online survey (SurveyMonkeyTM) distributed to all GD and PD program directors in the US.
Results: 180 programs were surveyed. 59.4% (n=38) of the 64 respondents were GD, while 35.9% (n=23) were PD. For stage 0 melanomas, four weeks after diagnosis was the most common recommended treatment timeframe (43.8%, n=28), followed by two weeks (31.3%, n=20). For stage 1A tumors, two weeks was most commonly recommended (43.8%, n=28), followed by four weeks (28.1%, n=18).
Conclusions: Most respondents recommended treating stage 0 and 1A melanomas within two or four weeks of diagnosis. The most common recommendation for stage 0 tumors was within four weeks, while two weeks was preferred for stage 1A tumors.
Keywords
Melanoma; Excision; Timeframe; Dermatology residency; Procedural dermatology fellowship; Dermatologic surgeryIntroduction
Cutaneous melanoma is the most aggressive form of skin cancer, with a high mortality rate if not treated in a timely manner [1]. Although melanomas are far less common than other cutaneous carcinomas, such as basal cell carcinomas (BCC) or squamous cell carcinomas (SCC), melanomas account for the majority of deaths from skin cancer [2-4]. It is estimated that in 2015 there will be 9,940 deaths from melanoma, and 74,000 new cases of this malignancy [5]. Therefore, careful attention to established risk factors, especially in individuals prone to melanoma development, is important for detecting malignant lesions in their early stages [6,7]. When detected early, melanoma is quite curable - the five-year survival rate of Stage 1A melanoma is 91-99% [8]. However, with increasing tumor stage, the survival rate drastically decreases to 65-73% for stage IIIA tumors and 16-22% for stage IV tumors [8]. Thus, early detection and treatment of these malignant neoplasms is crucial to improving the probability of survival.Procedures for detecting, staging, and treating melanomas have been well established [9,10]. Nevi that satisfy the wellknown mnemonic ABCDE for basic melanoma identification [11] (asymmetry, border irregularity, color variation, diameter > 6 mm,and tumor evolution) indicate suspicious lesions. This mnemonic may assist patients in identifying potentially harmful lesions and prompt them to present to a dermatologist to have these lesions evaluated by a trained eye. Melanoma tumors are staged according to depth of invasion, according to the Breslow depth, which has been shown to be an accurate indicator of prognosis and helpful guide in subsequent management [9,10-12]. According to guidelines from the National Comprehensive Cancer Network (NCCN), in situ tumors should be excised with surgical margins of 0.5-1.0 cm, ≤1.0 mm-thick lesions with 1.0 cm margins, and 1.01-2.0 mm-thick tumors with 1.0-2.0 cm margins (Table 1) [13].
Early excision while tumors remain superficial (i.e. in stage 0 or 1A) is critical, as these lesions have not yet invaded into deeper structures [9,10-12]. Ideally, these tumors should be excised as soon as the diagnosis of melanoma has been rendered, but due to variations in clinic availability and scheduling, immediate treatment is not always possible [14,15]. However, no recent studies have established a maximum recommended time period between diagnosis and excision of stage 0 (melanoma in situ) and 1A tumors, and there are currently no official guidelines set by the National Comprehensive Cancer Network (NCCN), American Academy of Dermatology (AAD), or other comparable organizations that specify a timeframe for treatment. Therefore, it may be helpful to explore the typical timeframes currently recommended between diagnosis and treatment of stage 0 and 1A melanomas by general dermatology (GD) and procedural dermatology (PD) teaching programs in the United States (U.S.). Thus, we conducted a nation-wide survey of GD and PD teaching programs in order to assess the most common excision timeframes used for treatment of stage 0 and 1A tumors in the U.S.
Methods
An anonymous online survey was created with SurveyMonkeyTM and distributed via email to directors of all GD and PD programs in the U.S. Email addresses were obtained through the American Medical Association’s FREIDA Online and San Francisco Match database.Data was analyzed via Independent T-test for continuous variables and Chi Square/Fisher’s exact test for binary variables in SPSS Version 22. The primary outcomes were the proportions of respondents from GD and PD teaching programs who recommended excision of stage 0 or 1A melanoma tumors within timeframes of 1-3 days, 1 week, 2 weeks, 3 weeks, or 4 weeks, as well as the percentage of respondents who reported being able to perform treatment within their recommended time period.
Results
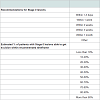
Of the 180 GD and PD program directors surveyed, 35.6% (n=64) responded. Of the 64 respondents, 62.3% (n=38) were from GD residencies, while 37.7% (n=23) were from PD fellowship programs.For stage 0 melanomas, four weeks after diagnosis was the most common recommended timeframe for treatment (43.8% of all programs, n=28), followed by two weeks (31.3%, n=20), one week (7.8%, n=5), three weeks (4.8%, n=4), and 1-3 days (1.6%, n=1). In addition, when analyzed separately, both GD and PD programs indicated that a four-week period after establishment of diagnosis was the most commonly suggested timeframe for excision of these tumors (Table 2).
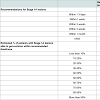
On the other hand, for stage 1A tumors, two weeks was the most common recommended time period (43.8% of all programs, n=28), followed by four weeks (28.1%, n=18), one week (10.9%, n=7), three weeks (4.7%, n=3), and 1-3 days (1.6%, n=1). However, when GD and PD responses were analyzed separately, we found that the most common treatment timeframe recommended by GD program directors was two weeks (55.3%, n=21), while the time period used by most PD programs was four weeks (34.8%, n=8). However, this did not reach statistical significance.
Most respondents reported being able to schedule greater than 90% of patients within their recommended timeframes (67.7%, n=42 for stage 0 tumors; 64.5%, n=40 for stage 1A tumors) (Table 3).
Discussion
Although melanoma only accounts for 5% of all skin cancers diagnosed in the U.S. [8], it is responsible for the majority of deaths from skin cancer [5,11,16-18]. One of the most crucial factors in improving the probability of survival is the detection of malignancy while the tumor is still superficial (i.e. in stage 0 or 1A) and has not yet invaded into underlying structures. With increasing tumor invasion, survival rates drop steeply [9]. Thus, it is imperative to detect and treat malignant lesions as early as possible.While guidelines for melanoma staging and excision margins have been well established [10,12], there have been no recent studies on recommended time periods between diagnosis of melanoma and actual excision of the tumor. Although immediate treatment is the best method for preventing tumor progression and disease recurrence, it is not always possible to excise the lesion upon diagnosis, and typically, there is a lag between detection of the tumor and surgical excision. Many studies have focused on factors that contribute to the delay of melanoma diagnosis-abilities of physicians to recognize malignant tumors, patients’ lack of awareness of suspicious skin lesions, and decreased motivation to present to clinic [6,19-21]. Additionally, the method of diagnosis is crucial - previous studies have indicated that excisional biopsy appears to be the most reliable way of detecting malignant lesions, in contrast to other techniques such as incisional, shave, or punch biopsies [22-24]. Selection of an inappropriate diagnostic modality due to lack of suspicion of a malignant tumor may also lead to a delay in melanoma diagnosis. Lott et al. found that about one in five Medicare beneficiaries experienced a delay in surgical treatment of melanoma of longer than 1.5 months, which was largely dependent on whether the tumor was biopsied by a dermatologist or non-dermatologist [25]. As these findings suggest that there may be coordination issues that can potentially shorten the delay in surgical treatment, it is important to evaluate the excision timelines followed by dermatology clinics. Furthermore, since no recent studies have reported the typical timeframe of tumor excision once a diagnosis has been made, and there are no established guidelines for specific excision timelines, it may be useful to be aware of the common timeframes employed by dermatologists in treating stage 0 and 1A melanoma lesions. To the best of our knowledge, there have also been no similar studies for basal cell and squamous cell carcinomas (BCCs, SCCs).
For stage 0 tumors, it appears that most GD and PD programs recommend excising tumors within a four-week period. In contrast, for stage IA tumors, while most PD programs still employed a four-week maximal time period for excision after establishment of a melanoma diagnosis, most GD training programs recommended excising these tumors sooner, within a two-week time period. However, this trend was not statistically significant. As our sample sizes are small for both groups, further studies involving larger survey pools are needed to further elucidate these results.
There are limitations to this study. First, only directors of GD and PD training programs were surveyed. Although program directors are generally cognizant of the practices of their colleagues and trainees and likely reported the treatment strategies most commonly utilized by their programs, it is possible that their responses do not accurately reflect the excision timeframes employed by the individual dermatologists and trainees within the program. In addition, only academic centers were surveyed, and the sample sizes for both GD and PD groups were small. Finally, information regarding melanoma recurrence and survival rates was not garnered in this survey. Future large multi-center studies that involve surveys of all trainees and faculty members in GD and PD programs, as well as information regarding outcomes and recurrences are warranted in order to further assess our preliminary findings.
Overall, this study shows the patterns of stage 0 and IA melanoma management in academic centers in the U.S. Since there are no recent studies or official guidelines outlining specific timeframes for excision of these lesions, it may be helpful to discover the most common treatment timelines that are currently employed by dermatologists across the nation. The preliminary findings from this study are important for establishing the foundation for future investigations concerning the management of early stage melanomas.
Acknowledgements
The Institutional Review Board (IRB) at the University of California, San Diego (UCSD) approved of the study protocol.References
- Miller AJ, Mihm MC Jr (2006) Melanoma. N Engl J Med 355: 51-65.
- Leiter U, Eigentler T, Garbe C (2014) Epidemiology of skin cancer. Adv Exp Med Biol 810: 120-140.
- Merrill RM (2011) Risk-adjusted melanoma skin cancer incidence rates in Whites (United States). Melanoma Res 21: 535-540.
- Bristow BN, Casil J, Sorvillo F, Basurto-Dávila R, Kuo T (2013) Melanoma-related mortality and productivity losses in the USA, 1990-2008. Melanoma Res 23: 331-335.
- NIH (2015) SEER stat fact sheets: melanoma of the skin. National Cancer Institute, Surveillance, Epidemiology, and End Results Program.
- Mayer JE, Swetter SM, Fu T, Geller AC (2014) Screening, early detection, education, and trends for melanoma: current status (2007-2013) and future directions: Part I. Epidemiology, high-risk groups, clinical strategies, and diagnostic technology. J Am Acad Dermatol 71: 599.
- Schmid-Wendtner MH, Baumert J, Stange J, Volkenandt M (2002) Delay in the diagnosis of cutaneous melanoma: an analysis of 233 patients. Melanoma Res 12: 389-394.
- Lawrence PF (2006) Surgical oncology: malignant diseases of the skin, the lymphatic’s, and soft tissue. In: Essentials of general surgery. Lippincott Williams & Wilkins, Baltimore, MD, USA.
- Osborne JE, Hutchinson PE (2001) Clinical correlates of breslow thickness of malignant melanoma. Br J Dermatol 144: 476-483.
- Bichakjian CK, Halpern AC, Johnson TM, Foote Hood A, Grichnik JM, et al. (2011) Guidelines of care for the management of primary cutaneous melanoma. American Acadmey of Dermatology. J Am Acad Dermatol 65: 1032-1047.
- AAD (2015) Melanoma: signs and symptoms. American Acadmey of Dermatology.
- NCCN (2014) Guidelines for treatment of cancer by site: melanoma. National Comprehensive Cancer Network.
- NCCN (2014) Guidelines for patients: melanom. National Comprehensive Cancer Network.
- Tomaszewski JJ, Handorf E, Corcoran AT, Wong YN, Mehrazin R, et al. (2014) Care transitions between hospitals are associated with treatment delay for patients with muscle invasive bladder cancer. J Urol 192: 1349-1354.
- Ahmed Z, Elmekkawy T, Bates S (2011) Developing an efficient scheduling template of a chemotherapy treatment unit: a case study. Australas Med J 4: 575-588.
- Donaldson MR, Coldiron BM (2011) No end in sight: the skin cancer epidemic continues. Semin Cutan Med Surg 30: 3-5.
- Cancer Epidemiol Biomarkers Prev 21: 1893-1901.
- Austin MT, Xing Y, Hayes-Jordan AA, Lally KP, Cormier JN (2013) Melanoma incidence rises for children and adolescents: an epidemiologic review of pediatric melanoma in the United States. J Pediatr Surg 48: 2207-2213.
- Brochez L, Verhaeghe E, Bleyen L, Naeyaert JM (2001) Time delays and related factors in the diagnosis of cutaneous melanoma. Eur J Cancer 37: 843-848.
- McKenna DB, Lee RJ, Prescott RJ, Doherty VR (2002) The time from diagnostic excision biopsy to wide local excision for primary cutaneous malignant melanoma may not affect patient survival. Br J Dermatol 147: 48-54.
- Silfen R, Amir A, Regev D, Hauben DJ (2002) Role of physicians and patients in the diagnostic delay of cutaneous malignant melanoma. Ann Plast Surg 49: 439-442.
- Lin MJ, Mar V, McLean C, Kelly JW (2014) An objective measure of growth rate using partial biopsy specimens of melanomas that were initially misdiagnosed. J Am Acad Dermatol 71: 691-697.
- Sharma KS, Lim P, Brotherston MT (2016) Excision versus incision biopsy in the management of malignant melanoma. J Dermatolog Treat 27: 88-90.
- Yamashita Y, Hashimoto I, Abe Y, Seike T, Okawa K, et al. (2014) Effect of biospy technique on the survival rate of malignant melanoma patients. Arch Plast Surg 41: 122-125.
- Lott JP, Narayan D, Soulos PR, Aminawung J, Gross CP (2015) Delay of surgery for melanoma among medicare beneficiaries. JAMA Dermatol 151: 731-741.