Journal of Cardiobiology
Download PDF
Research Article
*Address for Correspondence: Nazmi Krasniqi, Head, Division of Cardiology & Electrophysiology, Department of Medicine, GZO - Zurich Regional Health Centre, Spitalstrasse 66, CH-8620 Wetzikon, Switzerland, Tel: +41 44 934 23 52, E-mail: nazmi.krasniqi@gzo.ch
Citation: Markendorf S, Eriksson U, Kovacs B, Krasniqi N. CRT-P Implantation and Consecutive AV-node Ablation as Rescue Therapy for Refractory Atrial Fibrillation: A Single Center Experience. J Cardiobiol. 2016; 4(1): 5.
Copyright © 2016 Markendorf S et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Cardiobiology | ISSN: 2332-3671 | Volume: 4, Issue: 1
Submission: 20 August, 2016 | Accepted: 16 September, 2016 | Published: 23 September, 2016
CRT-P Implantation and Consecutive AV-node Ablation as Rescue Therapy for Refractory Atrial Fibrillation: A Single Center Experience
Susanne Markendorf1, Urs Eriksson2, Boldizsar Kovacs1 and Nazmi Krasniqi3*
- 1Division of Cardiology, GZO - Zurich Regional Health Centre, Spitalstrasse 66, CH-8620 Wetzikon, Switzerland
- 2Head, Division of Internal Medicine, GZO - Zurich Regional Health Centre, Spitalstrasse 66, CH-8620 Wetzikon, Switzerland
- 3Division of Cardiology & Electrophysiology, Department of Medicine, GZO - Zurich Regional Health Centre, Spitalstrasse 66, CH-8620 Wetzikon, Switzerland
*Address for Correspondence: Nazmi Krasniqi, Head, Division of Cardiology & Electrophysiology, Department of Medicine, GZO - Zurich Regional Health Centre, Spitalstrasse 66, CH-8620 Wetzikon, Switzerland, Tel: +41 44 934 23 52, E-mail: nazmi.krasniqi@gzo.ch
Citation: Markendorf S, Eriksson U, Kovacs B, Krasniqi N. CRT-P Implantation and Consecutive AV-node Ablation as Rescue Therapy for Refractory Atrial Fibrillation: A Single Center Experience. J Cardiobiol. 2016; 4(1): 5.
Copyright © 2016 Markendorf S et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Cardiobiology | ISSN: 2332-3671 | Volume: 4, Issue: 1
Submission: 20 August, 2016 | Accepted: 16 September, 2016 | Published: 23 September, 2016
Abstract
Aims: Cardiac resynchronization therapy (CRT-P) and atrioventricular node (AVN) ablation are a recommended treatment option for patients with atrial fibrillation (AF) refractory to medical treatment or pulmonary vein isolation. Its impact on cardiac function and patient outcome in patients with narrow QRS complex and LVEF > 35%, however, remains controversial. The aim of our study was to analyse the impact of CRT-P implantation and AVN ablation on NYHA class, left ejection fraction, EHRA score and left atrial diameter in high symptomatic patients with permanent or paroxysmal AF with narrow QRS complex and LVEF > 35%.Methods: A database of 24 consecutive patients with permanent AF who underwent AVN ablation after CRT-P implantation was analyzed retrospectively. All patients suffered from symptomatic permanent or paroxysmal AF refractory to medical rhythm and rate control or pulmonary vein ablation. Coronary and valvular heart disease was excluded in all patients. Follow up examinations were scheduled on regular intervals after 3 months up 4 years after AVN ablation. Left ventricular ejection fraction (LVEF), left atrial diameter (LAD), NYHA class, EHRA score and pro-BNP-level before procedures were compared to corresponding data on follow-up.
Results: LVEF increased from 45.17 ± 10.95% to 53.63 ± 8.33% after CRT-P implantation and AVN ablation, NYHA class decreased 2.33 ± 0.64 to 1.21 ± 0.42, EHRA score decreased from 3.00 ± 0.51 to 1.13 ± 0.34. LAD decreased from 52.04 ± 3.39 mm to 48.96 ± 3.98 mm and pro- BNP decreased from 1257.38 ± 966.40 pg/ml to 579.04 ± 347.69 pg/ml. All changes were significant (p < 0.001).
Conclusion: In this retrospective single-centre analysis, we provide striking evidence for significant functional improvement und symptomatic benefit in patients with symptomatic and refractory atrial fibrillation with narrow QRS complex and LVEF > 35% after CRT-P implantation and AVN-ablation procedures.
Keywords:
CRT-P; Symptomatic atrial fibrillation; AV-node ablationIntroduction
The 2013 ESC guidelines on cardiac resynchronization and cardiac pacing assess rate permanent cardiac resynchronization therapy (CRT-P) with consecutive atrioventricular node (AVN) ablation a class IIa recommendation (Level B) for patients with symptomatic permanent atrial fibrillation (AF), despite medical treatment and pulmonary vein isolation [1]. Several trials compared effects of right, left and biventricular pacing on left ventricular ejection fraction (LVEF), NYHA class, left atrial remodeling in patients withatrial fibrillation or patients after AVN ablation due to refractory atrial fibrillation [2,3]. It has been found that right ventricular pacing results in significant increase of left atrial size and worsening of left ventricular contractility in patients with AF after AVN ablation. The effect of biventricular pacing in these patients, on the other hand, remains controversial. The heart rate control achieved with AV-junction ablation improved quality of life and exercise capacity with all modes of pacing in patients with severely symptomatic atrial fibrillation [4]. In contrast, some studies found biventricular pacing superior to right or left single-ventricular pacing regarding LVEF improvement or NYHA class changes in patients with permanent atrial fibrillation [5].Biventricular pacing is a well-accepted therapy for patients with chronic severe heart failure (LVEF < 35%), QRS > 120 ms and NYHA class III or IV. Many prospective studies [6,7] showed improvement of LVEF and NYHA class after CRT implantation in heart failure patients. Its efficacy in patients with atrial fibrillation and heart failure, however, is limited due to reduced percentages of biventricular pacing. In fact, it has been described that only those heart failure patients with AF, who underwent AVN ablation, showed sustained long-term improvements in cardiac contractility [8] and favorable outcome [9]. A meta-analysis [10] revealed improved outcome in AF patients with CRT implantation and insufficient biventricular pacing that underwent AVN ablation compared to those who did not. Importantly, however, AVN ablation did not result in additional functional improvement, such as LVEF, NYHA functional class or quality of life. More over, complete atrioventricular block, either spontaneous or induced, did not reduce mortality in a cohort of 155 CRT patients with permanent atrial fibrillation. The effect of CRT-P implantation and AVN-Ablation in patients with therapy refractory, symptomatic atrial fibrillation with LVEF > 35% and narrow QRS complex remains unclear. In this study, we evaluated the benefit of CRT-P implantation and consecutive AVN ablation in these patients in a real-world setting.
Methods
Population and baseline characteristicsConsecutive patients with symptomatic paroxysmal or permanent AF, and inefficient medical rhythm and rate control or unsuccessful pulmonary vein isolation underwent CRT-P implantation and AVnode ablation at our tertiary care centre between 2010 and 2016 and were enrolled in our database. For retrospective analysis, inclusion criteria were defined as age > 18 years, and symptomatic AF with normal or below normal LVEF (> 35%) prior to the intervention. Exclusion criteria were age < 18 years, asymptomatic atrial fibrillation with efficient rate control (< 100/min), EHRA score/NYHA class 1, symptomatic coronary and ischemic heart disease, valvular heart disease (i.e. severe aortic or mitral valve affections), or structural heart diseases. 24 patients qualified for the analysis. Baseline characteristics were age, sex, follow-up time after AVN ablation, eGFR before AVN ablation, QRS-duration before CRT-P implantation, the presence of coronary heart disease, the presence of AV-block, differentiation of permanent or paroxysmal AF and medical treatment. Patients were routinely assessed for NYHA class and EHRA score before and after the interventions on regular follow-up evaluation. Pro-BNPlevel before and after the intervention was checked on each followup examination as well as the echocardiographic parameters LVEF and left atrial diameter (LAD). CRT-P Settings such as pacing mode, ventricular pacing- and sensing location, as well as upper and lower rate limits were listed as well. Biventricular pacing was standard setting in all our patients. Percentage of biventricular pacing was recorded prior and after AVN ablation. The study complies with the Declaration of Helsinki. The local ethics committee approved the trial (KEK project ID 2016-00073) and written informed consent of all subjects has been obtained.
Device implantation and programming
Right ventricular leads were positioned at the distal or mid right ventricular septum. Atrial leads were implanted in all patients with paroxysmal atrial fibrillation. LV electrodes were placed through the coronary sinus. Immediately after AVN ablation CRT-P devices were programmed in all patients in VVIR mode at 80 bpm for 4 weeks. Then CRT-P devices were programmed at the discretion of the responsible attending physician.
Echocardiography
All patients underwent echocardiography before CRT-P implantation and on follow-up the first time 2 months after AVN ablation. Transthoracic echocardiography was performed according to the guidelines of the American heart association and executed with Siemens Acuson SC2000, Z6Ms transducer [11]. Echocardiography included standard short, and long axis views, as well as apical three, four and two chamber views. Standard examinations also included M-Mode tracings of long axis views, and tissue Doppler analysis. ECG triggered standard loops from all examinations were stored digitally. LVEF was assessed using Simpson’s biplane analysis and systolic LAD was assessed on M-mode analysis tracings from long axis views.
Statistical analysis
Analyses were done with descriptive statistic using IBM SPSS Statistics (Version 21. Armonk, NY). Categorical variables are expressed as percentages, quantitative variables as mean ± SD. Paired T-test and Wilcoxon test were used to compare numeric variables before and after the AV-node ablation, to show the difference between these variables and get its significance. As this is a retrospective trial, the level of statistical significance was defined as a 2-sided p-value less than 0.05.
Results
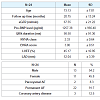
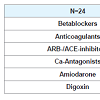
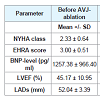
24 patients, 13 men and 11 women were analysed. Mean age was 73.13 ± 7.01 years and median follow up time after AV-nodeablation was 20.75 ± 13.24 months. A complete list of the baseline characteristics is shown in Table 1. 22 patients had permanent atrial fibrillation, 2 patients had paroxysmal atrial fibrillation. Before CRT-P implantation and AVN ablation the mean NYHA class was 2.33 ± 0.64 and EHRA score was 3.00 ± 0.51 (Table 1). The preintervention holter monitoring showed a minimum heart rate of 68 ± 32 bpm, mean heart rate of 84 ± 18 bpm, maximum heart rate 152 ± 36 bpm. The mean ejection fraction was 45.17 ± 10.95% and the mean LADs was 52.04 ± 3.39 mm (Table 1). All patients had medical treatment for atrial fibrillation at the time of CRT-P Implantation and AVN ablation. A list of the different drugs is shown in Table 2. All patients underwent successful CRT-P Implantation and 6 weeks thereafter AVN ablation. The LV-leads were implanted in all patients via coronary sinus in the posterolateral site. Immediately after AVN ablation lower rate limits of CRT-P devices was set at 80 bpm for 1 month and all patients got biventricular pacing. After the AVN ablation the programmed pacing mode was in 2 patients VVI-CLS, 11 patients VVIR and 11 patients DDIR. Mean base rate was 60.83 ± 7.76 bpm, mean programmed maximal heart rate was 129.17 ± 2.41 bpm.NYHA class improved from 2.33 ± 0.64 to 1.21 ± 0.42 (p < 0.001). EHRA score decreased from 3.00 ± 0.51 to 1.13 ± 0.34 (p < 0.001) after the intervention (Table 3 and Figure 1). LVEF increased significantly from 45.17 ± 10.95% to 53.63 ± 8.33% (p < 0.001) (Table 3 and Figure 2).
Left atrial diameter (LAD) decreased from 52.04 ± 3.39 mm to 48.96 ± 3.98 mm (p < 0.001) after intervention (Figure 2) and BNPlevel decreased as well significantly from 1257.38 ± 966.40 to 579.04 ±347.69 after AVN ablation (p < 0.001)(Figure 3).
Discussion
The main finding of our study is that the heart rate control via AVN ablation and cardiac resynchronization leads to a significant decrease of NYHA class and EHRA score and a significant improvement of LVEF in patients with therapy refractory symptomatic atrial fibrillation with a narrow QRS and with LVEF > 35. Moreover, we found a significant decrease of LADs of -3.08 ± 2.47 mm and a significant decrease of pro-BNP levels on follow-up (-678.33 ± 731.43 pg/ml). In contrast to other trials, with conflicting results [3,6,8], all our 24 patients clearly improved. As confirmed before, our study strengthened the findings of previous trials such as Brignone et al., Puggioni et al, etc. regarding LVEF improvement and reduction of LAD-size after CRT-P implantation and AVN-ablation in patients with atrial fibrillation. In patients suffering from symptomatic therapy refractory atrial fibrillation with mildly reduced LVEF remains the question how to treat these patients? The 2013 ESC guidelines on cardiac resynchronization and cardiac pacing assess rate permanent cardiac resynchronization therapy (CRT-P) with consecutive atrioventricular node (AVN) ablation a class IIa recommendation (Level B) for these patients. This is because the quality of evidence is moderate [1].In our analyses we showed a significant symptomatic and functional benefit of CRT implantation and AVN ablation in patients with symptomatic therapy refractory atrial fibrillation with below normal LVEF (> 35%) and narrow QRS complex in a real world setting.
As permanent or paroxysmal AF results in dilation of the left atrium and therewith favours again AF [12], every reduction of the LAD is considered to be of clinical seen importance [2]. A symptomatic permanent or paroxysmal AF has shown to induce clinically left ventricular remodelling with dysfunction and cardiomyopathy [13]. This seems to be reversible after AVN ablation, with improved quality of life and LVEF as well [14,15].
There are data about the effect of AV-node ablation and RV pacing in improvement of quality of life in patients with symptomatic AF [3]. This trial did not show any benefit of RV-pacing and AVnode ablation regarding LVEF in patients with atrial fibrillation. It seems likely that the main reason for the positive effect on quality of life via RV-based pacing after AVN ablation in patients with AF is the regularization of heart rate achieved with AV-junction ablation [3]. Another study showed a significant improvement of quality of life in patients with atrial fibrillation and biventricular pacing as well as in patients with RV-pacing after AVN ablation. But only in patients with biventricular pacing could be demonstrated a significant improvement of LVEF [3]. In our study we were able to show a significant decrease of NYHA class and EHRA score as well as improvement of LVEF through biventricular pacing and AVN ablation in patients with therapy refractory, symptomatic atrial fibrillation. There are controversial results regarding reduction of long term mortality in patients with permanent atrial fibrillation treated with cardiac resynchronization therapy [6,9]. The most important findings of these trials were the independent predictors of mortality such as NYHA class IV, glomerular filtration rate and LVEF. The improvement of LVEF and NYHA class could have an impact regarding long term mortality in patients with therapy refractory atrial fibrillation. In our study we could show an improvement of NYHA class and LVEF. Importantly, in our study the mean LVEF was 45.17% ± 10.95%. Comparing to other trials the mean LVEF inour study was slightly higher. However the improvement of LVEF after CRT-P implantation and AVN ablation was significant (8.46 ± 7.89%, p < 0.001).
Although a small sample size of patients with therapy refractory, symptomatic atrial fibrillation with a narrow QRS and LVEF >35% included in our study, we could show a significant functional improvement and a clinical benefit response in these patients treated with CRT-P and AVN ablation. Due to the results of our study and to the findings of other similar studies the CRT-P implantation and AVN ablation seems to be an effective therapy also for patients with therapy refractory, symptomatic atrial fibrillation with mildly reduced left ventricular ejection fraction and narrow QRS-complex.
This is a single-centre, observational, study with a small population size. This limits the strength of the findings. A large, randomized study is needed to confirm the observations of our trial.
References
- European Society of Cardiology (ESC), European Heart Rhythm Association (EHRA), Brignole M, Auricchio A, Baron-Esquivas G, et al. (2013) 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 15: 1070-1118.
- Puggioni E, Brignole M, Gammage M, Soldati E, Bongiorni MG, et al. (2004) Acute comparative effect of right and left ventricular pacing in patients with permanent atrial fibrillation. J Am Coll Cardiol 43: 234-238.
- Orlov MV, Gardin JM, Slawsky M, Bess RL, Cohen G, et al. (2010) Biventricular pacing improves cardiac function and prevents further left atrial remodeling in patients with symptomatic atrial fibrillation after atrioventricular node ablation. Am Heart J 159: 264-270.
- Brignole M, Gammage M, Puggioni E, Alboni P, Raviele A, et al. (2005) Comparative assessment of right, left, and biventricular pacing in patients with permanent atrial fibrillation. Eur Heart J 26: 712-22.
- Orlov MV, Gardin JM, Slawsky M, Bess RL, Cohen G, et al. (2010) Biventricular pacing improves cardiac function and prevents further left atrial remodeling in patients with symptomatic atrial fibrillation after atrioventricular node ablation. Am Heart J 159: 264-270.
- Tolosana JM, Trucco E, Khatib M, Doltra A, Borras R, et al. (2013) Complete atrioventricular block does not reduce long-term mortality in patients with permanent atrial fibrillation treated with cardiac resynchronization therapy. Eur J Heart Fail 15: 1412-1418.
- Schwartzman D, Housel D, Bazaz R, Jain S, Saba S, et al. (2015) A pilot study to assess benefit of atrial rhythm control after cardiac resynchronization therapy and atrioventricular node ablation. Pacing Clin Electrophysiol 38: 275-281.
- Gasparini M, Auricchio A, Regoli F, Fantoni C, Kawabata M, et al. (2006) Four-year efficacy of cardiac resynchronization therapy on exercise tolerance and disease progression: the importance of performing atrioventricular junction ablation in patients with atrial fibrillation. J Am Coll Cardiol 48: 734-743.
- Gasparini M, Auricchio A, Metra M, Regoli F, Fantoni C, et al. (2008) Long-term survival in patients undergoing cardiac resynchronization therapy: the importance of performing atrio-ventricular junction ablation in patients with permanent atrial fibrillation. Eur Heart J 29: 1644-1652.
- Yin J, Hu H, Wang Y, Xue M, Li X, et al. (2014) Effects of atrioventricular nodal ablation on permanent atrial fibrillation patients with cardiac resynchronization therapy: a systematic review and meta-analysis. Clin Cardiol 37: 707-715.
- Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, et al. (2003) ACC/AHA/ASE 2003 Guideline Update for the Clinical Application of Echocardiography: Summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation 108: 1146-1162.
- Olshansky B, Heller EN, Mitchell LB, Chandler M, Slater W, et al. (2005) Are transthoracic echocardiographic parameters associated with atrial fibrillation recurrence or stroke? Results from the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. J Am Coll Cardiol 45: 2026-2033.
- Vegh EM, Sood N, Singh JP (2013) The role of ablation of the atrioventricular junction in patients with heart failure and atrial fibrillation. Heart Fail Clin 9: 489-499.
- Kay GN, Ellenbogen KA, Giudici M, Redfield MM, Jenkins LS, et al. (1998 ) The Ablate and Pace Trial: a prospective study of catheter ablation of the AV conduction system and permanent pacemaker implantation for treatment of atrial fibrillation. APT Investigators. J Interv Card Electrophysiol 2: 121-135.
- Wood MA, Brown-Mahoney C, Kay GN, Ellenbogen KA (2000) Clinical outcomes after ablation and pacing therapy for atrial fibrillation : a meta-analysis. Circulation 101:1138-1144.