Journal of Addiction & Prevention
Download PDF
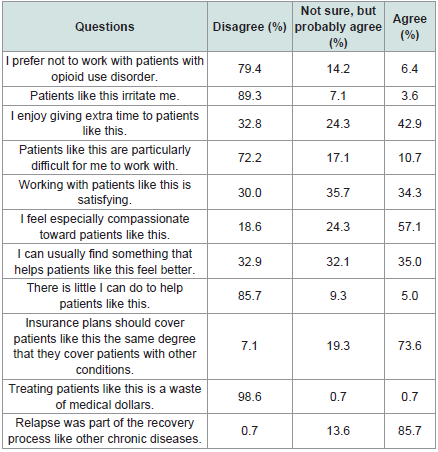
As shown in [Table 2] , in the pre-training survey, most participants were willing to take care of patients with OUD. They also felt that it was rewarding and satisfying to work with this specific population and agreed that OUD is analogous to other chronic diseases. Most participants agreed that health insurance plans should cover OUD treatment similar to treatment of other medical conditions.
Research Article
Impact of Virtual X-waiver Training on Perceptions of Barriers and Facilitators to Medications for opioid Use Disorder
Turner WH1, Burgan K1, Walter LA2, Hearld L3 and Li L4*
1Division of Infectious Diseases, University of Alabama at Birmingham,
Birmingham, AL USA
2Department of Emergency Medicine, University of Alabama at Birmingham, Birmingham, AL USA
3Department of Health Services Administration, University of Alabama at Birmingham, Birmingham, AL USA
4Department of Psychiatry and Behavioral Neurobiology, University of Alabama at Birmingham, AL USA
2Department of Emergency Medicine, University of Alabama at Birmingham, Birmingham, AL USA
3Department of Health Services Administration, University of Alabama at Birmingham, Birmingham, AL USA
4Department of Psychiatry and Behavioral Neurobiology, University of Alabama at Birmingham, AL USA
*Address for Correspondence: Li Li, Department of Psychiatry and Behavioral Neurobiology. University of Alabama at Birmingham, USA E-mail Id: liyli@uabmc.edu
Submission: 10 August, 2023
Accepted: 12 September, 2023
Published: 15 September, 2023
Accepted: 12 September, 2023
Published: 15 September, 2023
Copyright: © 2023 Turner WH, et al. This is an open-access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Keywords: X-Waiver Training; Virtual; Buprenorphine; Barriers; Facilitators
Abstract
Background: DATA 2000 X-waiver training has existed for over
20 years, however, less than 10% of eligible practitioners have been
waivered. The purpose of this study was to understand practitioners’
perceptions of X-waiver training and to assess the feasibility of virtual
X-waiver training.
Methods: Three separate virtual X-waiver training courses were
provided from December 2020 through September 2021. Pre- and post-training
surveys were developed to understand practitioners’ attitudes
toward patients with opioid use disorder (OUD) and to evaluate the
effect of the training. All participants were invited to complete surveys
anonymously via Qualtrics.
Results: Among 168 participants, 140 and 133 completed pre- and
post-training surveys, respectively. Analysis of the pre-training survey
data showed that 80% of practitioners were willing to treat patients with
OUD. Post-training responses documented significant improvements
in diagnosing OUD and recognizing opioid withdrawal symptoms.
Similarly, post-training results showed 96% of respondents noted
improved confidence in their capacity to prescribe buprenorphine.
Approximately 69% of respondents in the pre-training survey were not
aware of local community resources to refer patients for substance
use treatment; this was reduced to 34% in post-training responses. Postsurvey
qualitative data revealed that participants thought the virtual
training was efficient, however, suggested more in-person interaction
and lecture-based discussion. In addition, respondents continued
to report persistent barriers to implementation of buprenorphine
prescribing.
Conclusion: This study demonstrated the feasibility of delivering
X-waiver training virtually. In addition, X-waiver training improved
practitioners’ knowledge and comfort in identifying and managing
OUD although persistent barriers to buprenorphine prescribing remain
despite training.
Introduction
Nationally, approximately 80% of patients with opioid use disorder
(OUD) do not receive recommended medications for opioid use
disorder (MOUD).[1] Despite evidence that patients receiving MOUD
are more likely to remain engaged in treatment and less likely to use
illicit opioids,[2,3] widespread adoption of this approach has lagged.
[4,5] This implementation gap is stark in Alabama where, according
to the Substance Abuse and Mental Health Services Administration
(SAMHSA) database and publicly available data on the number
of physicians in Alabama, approximately 15% of physicians statewide
had undergone Drug Addiction Treatment Act (DATA) 2000
X-waiver training as of January 1, 2021.[1,6] Given the number of
patients with OUD in Alabama, each waived provider is expected to
serve over 500 patients, which is far beyond the cap established by
the federal regulations before the Drug Enforcement Administration’s
new regulation was announced in January 2023.[7] Furthermore,
many waived providers do not actively prescribe buprenorphine for
their patients with OUD due to a variety of reasons, including but
not limited to, stigma associated with this patient population and
lack of training and expertise.[8-10] Thus, it is not surprising that in
Jefferson County, the most populous county in Alabama, less than
20% of eligible patients receive evidence-based MOUD.[7] Taking this
into account, educating practitioners, assisting waivered practitioners
in delivering MOUD, and expanding MOUD training to include nonaddiction
medicine physicians is urgently needed to increase capacity
to treat patients with OUD in Alabama.
To address the overwhelming need, the University of Alabama at
Birmingham (UAB) was awarded a grant through the Foundation for
Opioid Response Efforts to provide X-waiver training to practitioners
primarily at UAB Hospital and Cahaba Medical Care Foundation
using a multidisciplinary approach. UAB Hospital is the largest
medical center in the Southeast region, and Cahaba Medical Care
Foundation is a Federal Qualified Health Clinic (FQHC), also located
in Jefferson County, Alabama, serving over 20,000 patients annually.
The educational objectives were: (1) to understand the practitioners’
willingness, attitudes, and perceptions regarding the treatment of
patients with OUD, and capacity to provide MOUD; (2) to evaluate the
impact of X- waiver training on practitioners’ knowledge and comfort
related to OUD and MOUD; (3) to determine any barriers impeding
buprenorphine prescribing; and (4) to identify opportunities to make
improvements in X-waiver training that would lead to increased
treatment of OUD.
The overall aim of the training was to increase access to MOUD
through education and telehealth. To evaluate these educational
objectives, pre- and post-training surveys were developed to
understand practitioners’ perceptions on DATA X-waiver training
and buprenorphine prescribing, as well as to identify potential
barriers to opportunities in improving the quality of trainings and
expanding MOUD access.
Methods
Study design:
The study was approved by the Institutional Review Board at the
UAB. X-waiver training was advertised via departmental emails at
UAB Hospital and Cahaba Medical Care Foundation. All interested
health care providers at UAB Hospital and Cahaba Medical Care
Foundation were encouraged to attend. X-waiver training consisted
of four hours of synchronous virtual training, followed by four hours
of online Providers Clinical Support System (PCSS) asynchronous
modules for physicians and physicians in training or sixteen hours for
advanced practice providers. The four hours of virtual training were
provided by physicians at UAB Hospital who were certified by the
PCSS. Training materials were provided by the PCSS and approved
by the American Academy of Addiction Psychiatry. Three separate
virtual X-waiver trainings were provided from December 2020
through September 2021.Survey Development and Data Collection:
Two staged participant surveys were developed by the authors
using Qualtrics, an online survey platform, to evaluate practitioners’
perceptions, to measure the effect of the virtual training, as well as
to receive general feedback on the educational objectives stated
above. Both pre- and post- training surveys were disseminated to
participants via email through an anonymous link or QR code. The
pre-training survey was administered one to two weeks ahead of the
virtual X-Waiver training event. Participants were asked to complete
the post-training survey within one week after the virtual training.
Quantitative and qualitative data were collected simultaneously for
data analysis. While both pre- and post-training surveys included
questions to assess the demographics of participants, no personal
identifying information was otherwise obtained. No incentive was
offered to respondents.The pre-training survey included 28 items assessing practitioners’
knowledge and experience of OUD and MOUD. We included
questions in the pre-training survey to understand participants’
attitudes, willingness to work with, and perceived stigma towards
patients with OUD. They were also asked about their understanding
of the OUD disease course. The pre-training survey collected
objective data, including the number of patients previously treated
with buprenorphine and the clinical capacity of practitioners to treat
patients with buprenorphine.
The post-training survey included 24 items and was developed
to determine the feasibility of providing buprenorphine treatment
upon completing virtual X-waiver training. The primary outcomes
related to feasibility were assessed by the same seven questions
in both pre- and post- training surveys, which was assessed as
improved knowledge and comfort with regards to the recognition of
opioid withdrawal symptoms, the diagnosis of patients with OUD,
and the pharmacology of buprenorphine, including induction,
contraindications to, clinical indications for, and side effects.
Secondary outcomes included improved awareness of community
resources for substance use treatment, broader consideration of nonaddiction
clinical environments as appropriate medical venues to
engage and treat patients with OUD using buprenorphine.
Qualitative data via free text open-ended questions were also
collected in both pre-and post-training surveys. On the pre-training
survey, participants were asked “What barriers have you encountered
or do you anticipate with regard to assessing and treating patients
with OUD using buprenorphine or naltrexone”. On the post-training
survey, participants were asked about: (1) the most beneficial aspect of
the training; (2) the least beneficial aspect of this training; and (3) what
could have made the training better. Open-ended survey responses
were analyzed using thematic analysis by one coder. Adopting an
inductive approach, the coder became familiar with the responses for
each open-ended question and then developed a preliminary coding
scheme per question to seek out emergent patterns and concepts.
Following initial analysis, the codes were further refined and sorted
into appropriate categories of related themes and findings. This
process involved analyzing the existing codes to find similarities and
group them into categories based on common properties.
Quantitative and qualitative data from three separate virtual
training courses were collected independently and integrated
during data analysis. Statistical analyses were performed using SPSS
version 26 (IBM). Descriptive data are presented as frequencies and
percentages unless otherwise specified. The Pearson chi-square test
was utilized for comparing categorical responses from pre- and posttraining
surveys, with a significance level set at p<0.05. Qualitative
data analysis was performed to characterize training effectiveness,
suggestions for improvement, and barriers to implementing
buprenorphine provision.
Results
Characteristics of participants:
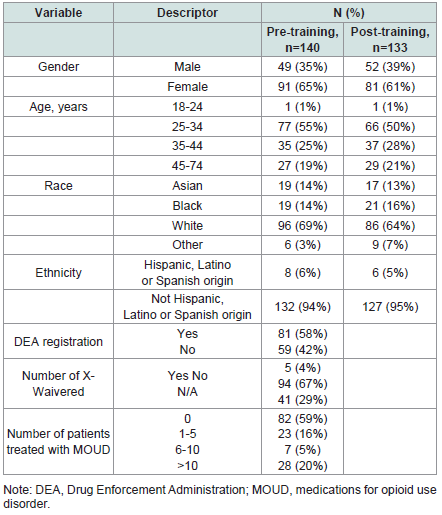
One hundred sixty-eight participants engaged in the three
virtual training courses. Demographics of participants are presented
in [Table 1] . Response rates were 83% (n=140) and 79% (n=133) forpre- and post-training surveys, respectively. Physicians (58%),
including residents (PGY1-PGY5) (42%) and attending physicians
(16%), represented the majority of participants who completed the
pre-training survey. Advanced practitioners (26%), including nurse
practitioners and physician assistants, also participated. Post-training
survey respondents were physicians in training (42%), attending
physicians (14%), and advanced practitioners (28%). There were
more female than male responses in both the pre- and post-training
surveys. Furthermore, over two-thirds of both sample populations
were in the 25-34 and 35-44 years-old age groups. Most participants
self-identified as white and non-Hispanic.
Quantitative analysis in pre- and post-training surveys:
Attitudes and stigma assessment in pre-training survey.As shown in [Table 2] , in the pre-training survey, most participants were willing to take care of patients with OUD. They also felt that it was rewarding and satisfying to work with this specific population and agreed that OUD is analogous to other chronic diseases. Most participants agreed that health insurance plans should cover OUD treatment similar to treatment of other medical conditions.
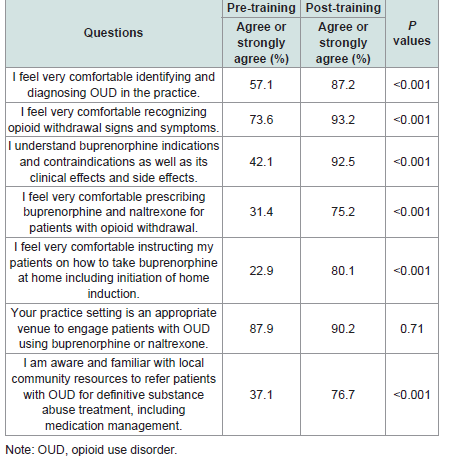
Effect of X-waiver training in addressing barriers to prescribe
buprenorphine. In the pre-training survey, more than half (57%)
of participants indicated they were comfortable identifying and
diagnosing OUD in their practice; however, this increased further
to 87% post-training [Table 3] . Similar results were demonstrated in
participants feeling comfortable recognizing opioid withdrawal signs
and symptoms, with 74% feeling comfortable pre-training compared
to 93% post-training. In the pre-training survey, only 42% reported
understanding buprenorphine indications and contraindications, and
31% expressed comfort prescribing buprenorphine to manage patients
with opioid withdrawal symptoms. There was a significant increase
(93%) in understanding the induction, contraindications, clinical
indications, and side effects of buprenorphine post-training. Comfort
levels also significantly increased with 75% reporting improved
confidence with regards to prescribing buprenorphine to manage
opioid withdrawal symptoms post-training. Similar results were seen
in the percentage of participants’ reporting comfort with instructing
patients on how to take buprenorphine at home, increasing from 23%
pre-training to 80% post-training.
Among the participants who completed both pre- and posttraining
surveys, the majority believed that their clinics were
appropriate places to engage patients with OUD using buprenorphine
or naltrexone and this did not change significantly as a result of the
training (88% vs. 90%, p=.71). Familiarity with local community
resources was significantly lacking (37%) prior to training with
providers unaware or unfamiliar with local referral options for
definitive substance abuse treatment, including MOUD. In the posttraining
survey, familiarity increased to 77%.
Qualitative analysis:
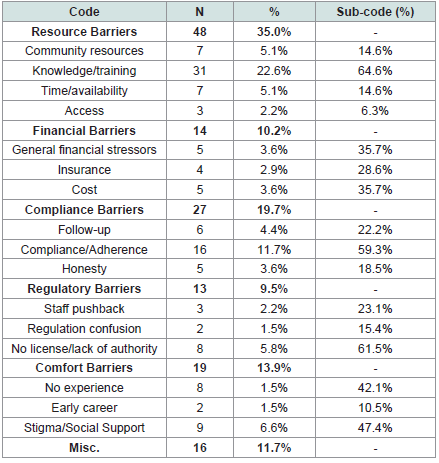
Pre-training
Our analysis identified five main themes regarding participants’
perceptions of barriers to providing OUD treatment in their clinic:
resources, financial, compliance, regulatory, and comfort barriers
[Table 4] . Several of these themes were interconnected and were
comprised of sub-codes to better understand and filter the data.Resource barriers were identified as responses reporting a general
lack of necessary resources, either in clinic or in the community, to
provide and maintain OUD treatment. Participants mostly reported
on a lack of knowledge, training, or confidence in prescribing
buprenorphine, as well as a lack of time and availability and lack of
access to treatment for patients. Similarly, many participants also
reported barriers related to comfort, either for the patient or the
provider. These participants noted that a lack of experience and being
early in their career provided significant personal challenges in terms
of barriers to care for their clinic; however, many noted that the lack of
social support services and perceived stigma provided more extensive
barriers in their practice.
Financial barriers included general financial stressors for patients,
specifically in terms of cost to the patient or lack of insurance coverage.
Regulatory barriers included general staff pushback to treating
addiction patients, confusion around government authorizations and
restrictions, and not having personal authority or licensure in their
clinic to provide such treatment.
Notably, many respondents reported adherence to treatment as
a primary barrier to care for this patient population. Participants
noted that lack of or confusion around follow-up procedures, a lack
of adherence to treatment regimen, and patient transparency around
addiction were top barriers to providing treatment.
Miscellaneous barriers included unique responses that did not fit
within the existing coding scheme. These responses addressed barriers
such as complexities surrounding comorbidities in this population,
referring to other clinics, working within the court system, and lack of
established relationships with patients.
Post-training:
Five main themes emerged when participants were asked about
the most beneficial aspects of the training: case studies, treatment,
topic relevance, type of information covered, and presentation style
and format.The overwhelming majority of participants (40.8%) commended
the presenters and appreciated the interactive nature of the training
course. Participants noted that having comprehensive slides, as well
as frontline physicians with firsthand experience in treating this
population, as being the most beneficial component of this training.
Several participants noted that “the presenters were great,” “well
rounded,” “engaged,” and “invested” which contributed to the delivery
of the training. Many participants (22.4%) also noted that they found
the case studies to be the most beneficial portion of the training, as it
enables them to apply material covered in the course and think through
real-world scenarios. One participant wrote “going over the case
studies made the learning more meaningful and allowed application
of learned material,” with another noting that the interactive examples
“helped provide perspective.” Similarly, many participants (22.4%)
found the information on MOUD and OUD treatment in the
training to be greatly beneficial and relevant. Key areas participants
mentioned as the most useful included understanding withdrawal
symptoms, information on prescribing suboxone, how to best instruct
patients on taking their medications, and general dosing guidance for
MOUD. Lastly, some respondents (7.2%) noted specific information
as being the most beneficial, such as understanding the connection
of dual diagnosis, inclusion of non-judgmental terminology, and
the process of becoming x-waivered, while others (7.2%) provided
general statements on the training being “interesting”, “high yield”,
and “relevant to [their] patient population”. Such statements included
“The whole thing was helpful. I appreciated the background/history
information and the practical how-to information,” and “the whole
training was beneficial.”
When asked about the least beneficial aspect of the training,
four main themes emerged, including: presentation style and format,
length of training, additional instructions, and topics/information
provided. While many had reported they found the presentation style
and format to be engaging and beneficial, when asked “what could
have made this session better,” many participants (50%) reported that
they did not like the current format. Key areas participants noted as
needing improvement included providing even more case studies and
interactive elements or making the training on demand. However,
some respondents recommended moving the training to all inperson
rather than virtual to enhance engagement. Similarly, many
participants reported issues with the length of the training. While the
majority found the training to be too long and would have appreciated
it being broken up over several days or having more breaks, two
participants reported they would have liked the training to be longer
to provide more information and time for interactive elements.
While participants previously praised the content covered, when
asked how to improve the training, many (17.4%) responded with
specific topics they would like to see covered in future sessions.
Notably, participants seemed interested in information on postsurgical
pain management for patients with OUD, addressing and
overcoming stigma, understanding more unique aspects to care,
and more information on local resources available. Lastly, some
participants (8.1%) reported that they would appreciate more
instruction or direction prior to class, either in terms of pre-course
work to help with comprehension during the training, or by providing
more reminders about training requirements.
Discussion
This study demonstrates that virtual delivery of X-waiver training
course is feasible and has the capacity to improve practitioner’s
knowledge, comfort level, and attitudes as they relate to OUD
treatment.
Changes to practitioners’ perceptions:
Buprenorphine can be prescribed by both physicians and
advanced practice providers who have X-waiver numbers before
January of 2023. However, practitioners generally lack the training
in assessing substance use disorders, including OUD, and related
treatment options. In 2019, there were only 3,000 certified addiction
specialists in the United States.[11] The lack of addiction training
begins at the level of undergraduate and medical school education
and proceeds through residency and fellowship with only 66 of the
nation’s 187 accredited medical schools offering addiction medicine
fellowships in 2019.[12-17] Increased opioid-related overdose death
and addiction provider deficit may spur more eligible practitioners
to seek training and treat OUD.[18]Consistent with this, results
from our pre-training survey found moderate to strong attitudes
and enthusiasm to learn about OUD and treat patients with OUD
among respondents. Our post-training survey results also indicate
that virtual X-waiver training can improve practitioners’ ability to
understand buprenorphine’s pharmacology, which is imperative to
treating patients with OUD. Results from the comparative analysis
of the pre-and post-training surveys showed participants increased
their knowledge related to identifying and treating patients with OUD
as well. This increase in knowledge is reflected in provider’s comfort
in engaging patients with OUD, which is a positive step toward
combating the opioid epidemic. [19,20] Therefore, our findings
underscore the positive impact that X-waiver training can have on
practitioners’ knowledge of OUD and their ability to treat it.Although the Department of Health and Human Services
announced in April 2021 that it would allow eligible practitioners
to apply for X-waiver numbers without formal X-waiver training,
many practitioners still feel they are not equipped with appropriate
knowledge, and thus not comfortable enough, to properly engage
in treating patients with OUD.[21,22]Acknowledging and filling
in this gap in knowledge through X-waiver training course plays a
critical role in expanding access to MOUD.[23-24] Feedback from
our participants also found the need for practitioners to practice their
knowledge and improve confidence with prescribing buprenorphine.
Thus, a structured learning environment, including a mixture of
training modules and practice, is critical to prepare practitioners
to assess and treat patients with OUD. Similarly, the majority of
participants expressed the need for further training in the posttraining
survey, echoing sentiments reported in previous research.
[25] Continued interest from practitioners for more training on
MOUD emphasizes the need among practitioners for more education
and mentoring.
Barriers in prescribing buprenorphine:
Historical barriers for prescribing MOUD have included
practitioner stigma, insufficient training, education, and experience,
as well as lack of specialized support, inadequate or burdensome
reimbursement, and burdensome regulatory procedures.[26-29] In the current study, participants echoed many of these cited
barriers. Additional barriers included lack of comfort prescribing
buprenorphine, negative perception of patient interest or ability to
comply with medication requirements, practitioners’ relationship
with patients (e.g., limited rapport), limited time to assess patients,
and lack of awareness of community resources and referral partners.
While stigma and mitigating its influence on practitioners remains
a public health priority to expand access to care for patients with
OUD,[28,30] our study demonstrated practitioners’ willingness to
treat patients with OUD. Further, a majority of participants considered
it “rewarding and satisfying” to treat patients with OUD, a sentiment
that may be reflective of a trend toward decreased stigmatization of
OUD.Another persistently cited barrier amongst participants was the
cost of MOUD, which may impact patient adherence to treatment and
increase the risk of reuse or overdose. This cost impact is even broader
in a Medicaid non-expansion state, including Alabama.[31] As a
result, the National Institute on Drug Abuse has emphasized the need
for further research on how to approach payment reimbursement
for MOUD.[32] Moreover, further practitioner training can expand
access to MOUD by addressing barriers and misconceptions, and in
return increase much-needed care for patients.[33] While the training
directly addressed many reported pre-training survey barriers, some
barriers persist, such as awareness of available community resources,
which highlights an opportunity for future engagement and further
targeted training.
Factors facilitating training:
Qualitative responses indicated that experienced trainers
specialized in addiction medicine are ideal facilitators. Participant
feedback found that the presentations, which were conducted by the
physicians currently practicing addiction medicine, were informative
via the demonstration of “real-world experience”. Similarly,
participants found the case studies utilized throughout the training to
be important in better understanding the decisions and situations they
may face when providing care to patients with OUD. Furthermore,
few participants noted they preferred in-person over a virtual format
for future trainings. This may suggest a preference amongst providers
for virtual training; however, further exploration is needed to support
this. Given participant interest in available resources and referral
options, developing locally informed training alongside addiction
medicine specialists may be an effective route for ensuring future
interest and engagement. These findings, and further investigation
into preferred training formats, may prove useful in designing and
implementing future X-waiver and other addiction-related trainings.Study strengths and limitations:
Due to the COVID pandemic, we adjusted the training modality
from in-person to virtual to enable practitioners the flexibility of
attending from any place and eliminate additional time commitments
such as travel time. Although virtual training is feasible, our posttraining
survey results showed that practitioners preferred more
case-based discussion and more interaction with trainers, which
may be more suited for in-person training. A previously documented
challenge for practitioners is the time commitment associated with
X-waiver training. Prior research found that it was perceived as
too burdensome for practitioners to fit X-waiver training into their
already busy schedules.34 To address this concern, we provided three
virtual training courses that allowed practitioners to complete their
training hours in more than one training module. Thus, being flexible
for practitioners to complete required training hours at their own pace
could be an option to increase the number of waivered practitioners
and expand access to MOUD.Our study has several limitations. First, our study is a crosssectional
design with surveys limited to pre-training and posttraining
within 1-2 weeks, and therefore, cannot predict long-term
impacts of virtual X-waiver training. For this, longitudinal data on
the perceptions of practitioners post- training would be beneficial in
understanding the role of X-waiver training in addressing barriers
associated with OUD management and MOUD access. Second, our
respondents are practitioners who signed up for this training and thus
may represent a biased sample regarding the degree of interest in OUD
management, which might have influenced our results. Lastly, our
study had a relatively small sample of participants which prevented us
from considering conditional relationships that would have allowed
us to identify common and unique preferences by subgroups (e.g.,
physicians vs. advanced practice providers). These findings may be
further limited by having only one coder analyze the open-ended
responses in pre- and post-training surveys.
Conclusion
Our study shows that virtual X-waiver training is feasible and
contributes new understanding of the barriers and facilitators to
X-waiver training and buprenorphine prescribing. Our findings
emphasize the capacity of X-waiver training to address some barriers,
especially practitioners’ knowledge gap and comfort level. Future
interventions aimed at improving access to MOUD may need to focus
on being flexible with training modality, affordability, and community
resource awareness and referral partners.
Acknowledgments
This research was supported by an award from the Foundation
for Opioid Response Efforts to L.L. We would like to show our
appreciation to participants in our virtual X-waiver training courses,
and respondents who completed pre- and post-training surveys.
Disclosure:
The authors report no conflicts of interest