Journal of Addiction & Prevention
Download PDF
Case Report
A Case Study on the Impact of COVID -19 and Social Capital on the Delivery of Medication - Assisted Peer Support
Kravetz ZJ1*, Prakash N1, Lahiri S1, Kunzelman J2, McConnell N2, Fernander A1 and Howard H3
1FAU Charles E. Schmidt College of Medicine, Florida, USA
2Rebel Recovery, Florida, USA
3FAU Phyllis & Harvey School of Social Work, Florida, USA
*Address for Correspondence
Kravetz ZJ, FAU Charles E. Schmidt College of Medicine, 777 Glades Road
BC - 71, Boca Raton, FL 33431, USA; E-mail: zkravetz2018@health.fau.edu
Submission: 25 January, 2022
Accepted: 28 June, 2022
Published: 04 July, 2022
Abstract
Introduction: The COVID - 19 pandemic has interfered with
innumerable services in different sectors of the healthcare industry,
including the opioid use disorder recovery community. This communitybased
empirical study explored the impact of the COVID-19 pandemic
and the mutually reinforcing variable of low social capital on the
distribution of medication - assisted peer support.
Methods: Six interviews with leaders of a combined medication
- assisted and peer support group were conducted to identify the
impact of COVID - 19 and low social capital on the substance use
disorder recovery community. Specifically, the recovery community
is incarcerated individuals receiving buprenorphine treatments and
individuals who have been released into the community. Using a
comparative analysis of these interview transcriptswe identified key
areas for procedural changes to reduce the impact of the COVID -
19 pandemic and low social capital on the delivery of medication -
assisted peer support.
Results: Two major themes were elucidated through interviews with
six peer support organization executives (PSOE) and recovery peer
support specialists (PSS): the effect of the COVID-19 pandemic on the
delivery of medication - assisted peer support services and the effect
of low social capital factors on the delivery of substance use recovery
resources. Secondary to these themes, services have dropped from
daily group activities to difficult-to-schedule weekly one-on-ones, and
constant barriers in communication with participants secondary to the
COVID-19 pandemic.
Discussion: Losing interpersonal relationships of medication -
assisted peer support has disproportionately affected those who
otherwise have none, resulting in a loss of accountability in recovery
efforts. By increasing the duration and frequency of meeting times and
hiring additional service leaders to take on these responsibilities, there
can be a restoration in the value of the program. Additional studies
are needed to further clarify the impact of COVID - 19 on the SUD
recovery community, the complications of low social capital on the
SUD recovery community, and strategies to help mitigate the impact
of COVID - 19 on these issues.
Conclusion: In the opioid recovery community, the distribution and
efficacy of medication - assisted peer support programs have been
severely reduced by COVID - 19 and social capital related factors -
and often a combination of the two. Through this case study, we have
identified targeted areas of improvement to optimize medication -
assisted peer support and other recovery resources.
Keywords
Opioid use recovery; COVID - 19; Medication - assisted peer
support; Opioids, Social capital, Case study
Introduction
In the United States, the past thirty years have seen an increase
in the use of prescription opioids that is commonly known as the
opioid epidemic. The 2019 National Survey on Drug Use and Health
indicates that8.3% of people, 12 years old or over, have used illicit
drugs in the past year. One approach to treating individuals with
an opioid use disorder is peer support services (PSS). Peer support
involves providing non-clinical assistance from individuals with similar conditions to patients who are recovering from conditions
such as opioid addiction, alcohol addiction, and certain mental health
illnesses. Some programs combine these peer support services with
medication - assisted treatment to help promote “whole - person”
recovery in individuals with substance use disorder. Medication
assisted treatment (MAT), is the combination of opioid agonist
treatment (i.e., methadone) or partial agonist (buprenorphine) with
counseling and other forms of therapy for the treatment of opioid
use disorder. The combination of PSS and MAT is referred to as
“Medication - assisted peer support” [1-3].
Certain programs focus on administering peer support and clinical
treatment to individuals recovering from substance use disorder who
are incarcerated [4]. These programs address the impact of economic
restraints on substance use disorder, breaking cycles of problematic
opioid use, and criminal justice system involvement. Peer support
programs are also imperative for previously incarcerated individuals
who are released from prison as they have a high risk of post - release
opioid - related overdose mortality [5,6].
Social capital framework:
Social capital is a concept that focuses on social relationships
between people that include a variety of factors such as community
networks, civil engagement, and personal connections [7,8].
Community programs that provide recovery support services to
individuals suffering from opioid use disorder (OUD) rely heavily on
social capital. Social capital factors such as a lack of social capital (i.e.,
lack of access to stable income, education, and housing) and lack of
access to civic resources (i.e., community centers and libraries) may
lead to higher rates of opioid - related deaths [9]. Researchers found
that countries with the lowest amounts of social capital tend to have
the highest overdose rates [7].In addition to the lack of access to social capital resources, there
are mass incarcerations of individuals for drug crimes that further
reduce the social capital of individuals with substance use disorder.
Mass incarcerations limit access to social capital resources such as
peer support, educational opportunities, and community resources [7]. In Abbott et al. (2019), researchers found that social capital in
the form of peer networks was important for the promotion of well
- being. Furthermore, researchers found that social capital plays an
important role in the recovery process, which is described using the
concept of “social recovery” [5]. In addition, barriers to social capital
and ultimately “social recovery” negatively impact the recovery
process [6].
Access to programs that provide clinical and peer support
recovery services are also subjected to barriers posed from racism
or bias. Minority communities are disproportionately affected by
substance use disorder and require clinical and peer support recovery
services. And yet, they are also subjected to barriers posed from
discrimination due to race or bias. Researchers found that physician
bias, coupled with inherent healthcare system biases led to obstacles
for minority groups in accessing healthcare providers that offer
medication - assisted opioid recovery.
COVID - 19 has created new challenges for the opioid recovery
community through disrupting many social networks (i.e., in - person
recovery programs) that are central to building social capital. Benton
et al., (2020) details that social capital is valuable and there needs to be
creative methods to support social networks during the COVID - 19
pandemic [10]. This study indicates that there is a new set of concerns
that focus on the current COVID - 19 pandemic in terms of social
capital and ultimately the recovery community.
The COVID - 19 pandemic has strained financial and clinical
resources for healthcare institutions throughout the United States
[1]. One aspect of the healthcare industry impacted by COVID - 19
is the delivery of opioid recovery resources. Specifically, the delivery
of both clinical treatment and peer support services are vulnerable
to the impact of COVID - 19 [11-13]. However, the impact of
COVID - 19 on the delivery of combined clinical treatment and peer
support services to individuals who are incarcerated has not been
fully elucidated. This study explores the impact of COVID - 19 on
the combined medication - assisted and peer support using a social
capital lens to better understand the relationship between the opioid
epidemic, treatment, and recovery.
Methods
The IRB institution from a Southern metropolitan university
reviewed the study and deemed it exempt. Six peer support
organization executives (PSOE) and recovery peer support specialists
(PSS) from a community-based organization with knowledge of
combined medication - assisted peer support were selected for
interviews. We conducted interviews virtually due to the COVID - 19
pandemic.
Since its inception, this recovery - community organization
has provided service provider navigation, linkages with treatment
providers and community resources, advocacy, harm reduction
training, recovery planning, and support groups. This organization
delivers 15,000 hours of recovery support services and 12,264 hours
of outreach annually and serves 1100 individuals experiencing SUD
in the local county each year. Services are tailored to support longterm,
sustained recovery and self-sufficiency; the average length of
participant engagement is 123 days. The staff includes 17 certified
peer specialists, along with 2 full - time Case Management Personnel and two executives. They have also partnered with the county to offer
peer support services in the local jail, coordinated with stakeholders to
provide housing for unsheltered persons residing in an encampment
in a local park, and established a partnership with the Department
of Children and Families to provide services for adults with child
welfare and dependency court cases.
The inclusion criteria included organization leaders who were
involved in implementing the program, such as the CEO of the
recovery program and the clinical director who oversee the medication
- assisted peer support service. To gain insight on the daily operations
of the prison recovery program we included interviews from four
peer leaders who were involved in delivery of medication - assisted
peer support. Peer leaders not involved with the medication - assisted
peer support division of the recovery program were not included.
The research team has an ongoing university-community
partnership with the recovery community organization (RCO) one
area of equal interest is a forthcoming evaluation of the medication
- assisted peer support program. The data collection procedures
consisted of six interviews ranging in length from 30 - minutes to
1 - hour using the CISCO video software WebEx. Participants agreed
to an informed consent and answered six questions listed in below.
We digitally recorded the interviews, and audio files were safely saved
on a password protected computer. Following the interviews, we
uploaded the audio files to the audio - transcription service REV.com.
We then transferred the transcripts to the analysis program NVivo.
Interview questions used to collect data from peer - support
organization executives and peer leaders.
➢ How has delivery of medication - assisted peer services
changed due to the recent COVID - 19 pandemic?
➢ What challenges have you faced in delivering peer services to
participants during the COVID - 19 pandemic?
➢ What changes have you noticed in medication - assisted peer
services participant engagement and satisfaction during the
COVID - 19 pandemic?
➢ What feedback have you received from participants about
delivery of peer services during the COVID - 19 pandemic?
➢ Do you have examples of successful strategies that improved
delivery of peer services during the COVID - 19 pandemic?
➢ How do you navigate delivering peer services to participants
who are different from you?
Upon completion of the interviews, we used constant comparative
analysis methods to analyze the results and develop concepts and
themes via coding information from transcribed interviews (Glaser
et al. 2017). The interview transcripts were uploaded to the NVivo
analytical software and additional coding was performed to generate
themes. After data saturation using a social capital framework,
themes were decided upon after discussion with PSOEs and PSSs. To
promote credibility, we worked closely with the CEO and operations
manager of the peer support organization who provided further
insight to the development of these themes. After member checking,
the community stakeholder agreed that the themes represented
common concerns found in the majority of cases.
Given the questions that still remain as to what exactly
constitutes good qualitative work; several guidelines for writing and
disseminating qualitative manuscripts were followed [11].
Results
Participant Characteristics:
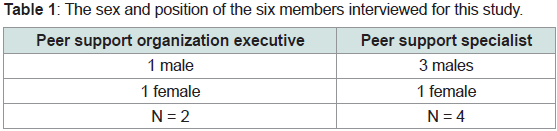
There were N=6 peer support organization executives (PSOE)
and peer support specialists (PSS) who met the inclusion criteria
for participation in the interviews. All peer support specialists were
certified to work in the peer support field and actively work for a
community - based peer support organization in the Southern United
States. Table 1 identifies the interview participants based on position
and gender identification.Themes:
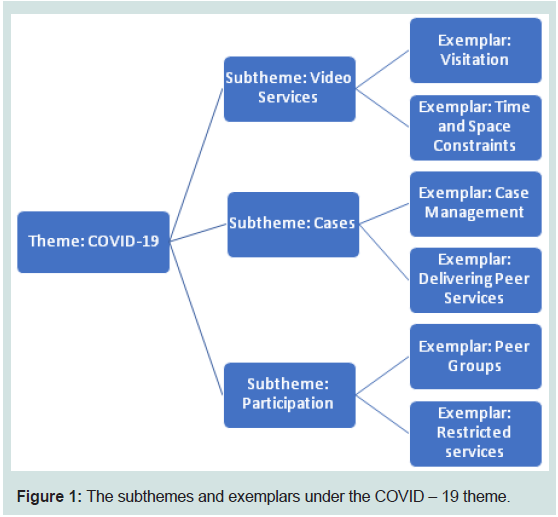
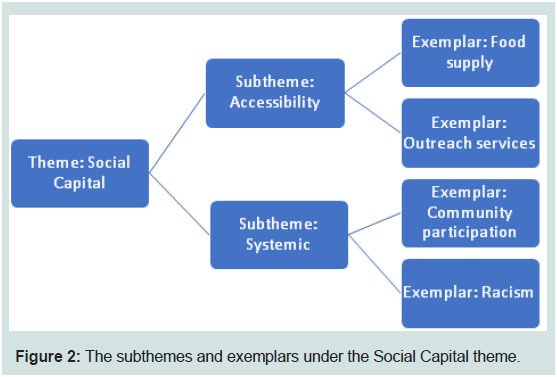
Two major themes were elucidated through interviews with
PSOE’s and PSS’s (considered major if identified in at least half of
the interviews):
➢ The effect of the COVID-19 pandemic on the delivery of
medication - assisted peer support services and
➢ The effect of low social capital factors on the delivery of
substance use recovery resources.These themes are represented in Figure 1 and 2, below, along
with specific issues (subthemes) related to these themes impeding
access to necessary services.
Theme 1: The effect of the COVID-19 pandemic on the delivery
of medication - assisted peer support services.
In reference to the COVID-19 pandemic, we identified video
services, cases, and participation as critical subthemes that represented
barriers to medication - assisted peer support.
Video Services:
Within the subtheme of video services, visitation (n=5) and time
& space constraints (n=3) were mentioned by interviewees as issues
reducing access to interpersonal relationships necessary for keeping
program participants motivated and accountable. A PSOE stated
that:“The program participants did not always play nice, everybody
does not communicate well, we were getting mixed messages on
how we could still see them, how we could talk to them, can we have
video conference and what that looks like for delivering services.”This
constant miscommunication with program participants was
compounded by higher-ups telling service leaders that they were:
“…only able to conduct direct services periodically through a video
telecommunications center.” (as stated by a PSS).A PSS mentioned that specifically in the prison dorms, there is
only one video visitation room, a limitation related to COVID-19.
This has, according to a PSOE, caused “A huge shift, that we’re not
able to make the same impact with individuals using substances over
the phone or video call that we would be in person because there are
certain intricacies about when you’re speaking to them that just don’t
translate well over video or other lines of digital communication.”
The new video services format, secondary to COVID-19, has
caused time and space constraints that, although do not sound like a
huge hindrance, create an extra barrier to interpersonal relationships
at the core of peer support. A PSS stated that: “It’s a whole thing to
the set up a fifteen-minute visitation when I can normally just drive to
the prison and go see who I want to see.”A PSOE mentioned a more
severe, yet not uncommon, case: “It took probably six to eight weeks
before we could actually set up a video conference with the guys.”
Cases:
The second subtheme encompasses issues with case management
and the delivery of peer services, secondary to COVID-19 case
changes. When comparing organizational cohesiveness prior to and
during the current pandemic, a PSS stated: “Just staying connected as
an agency and letting our case managers and our supervisors know
what was going on, made it a lot easier for everyone to be on the same page to continue to provide services.”Now that case management
is being done completely remotely, there is disjointedness within
the organization, which has led to vital information regarding
participants’ recovery progress go unnoticed, causing a reduction
in needed services being distributed to those who need them
immediately [15].A PSOE stated the following that highlights the shift from live
meetings with providers to the distance - based format, which has
caused an overextension of service leaders’ duties outside of the norm:
“We had our case managing entity hold calls with all the providers
that are in this network every week. Having these calls in place where
everybody was that gets paid by the managing entity here; we were all
on calls at 8:30 every morning on Monday, Wednesday and Friday”
[17-19].
Prior to the pandemic, peer services themselves were delivered in
a variety of different ways, including “outreach work from going into
the local communities, all the respite facilities” (according to a PSS).
This scope has now been severely limited. This again has changed the
efficacy and crux of the program itself. An additional PSS stated that:
“Obviously, when I received peer services, before I became a peer
counselor, I was able to make better connections with folks face to
face, person to person; you’re able to read body language better, and
all in all just build trust a little bit easier” [20,21].
Participation:
The final subtheme elucidated by interviewees (n=3) is a
reduction in participation from program participants themselves,
within peer groups and the other restricted services. Loss of the
central interpersonal relationships provided by medication - assisted
peer support due to difficulty scheduling visits, reduced visitation
time, and one-on-one meetings (rather than daily face-to-face group
work based on The Wellness Recovery Action Plan) has caused
participants to devalue the program itself. A PSS mentions: “I’ve had
one individual a couple months ago that didn’t want to continue
participating in peer services upon release from the program because
he wanted to know what he could get from our organization.”An additional PSS juxtaposes the highly involved curriculum
before and during the current pandemic: “We went from doing
several groups a day collectively and doing several one-on-ones,
keeping constant updates, down to only being able to meet with a
participant via telecommunications maybe once a week for 10 to 15
minutes at a time.”In the same vein, a PSS says: “Delivering services
in the medication - assisted peer support program, it almost became
nonexistent, because we went from doing several groups a day to
none at all” [22,24].
Theme 2: The effect of low social capital factors on the delivery of
substance use recovery resources.
In reference to low social capital, we identified accessibility and
systemic issues as barriers to medication - assisted peer support.
Accessibility Issues:
Participants (n=5) mentioned accessibility to resources as a
barrier to the delivery of medication - assisted peer support. A PSOE
mentions the interruption of the 60-day program (which involves
buprenorphine treatment, peer group activities, and self- reflection): “Frustration with not being able to access to services or for folks who
want to sign up, frustration having their services cut, essentially in the
middle of what’s supposed to be a 60-day program.”Many participants, incarcerated individuals specifically, are
affected by a restriction in program resources. A PSOE mentioned:
“That was a huge shift, but specifically with the medication - assisted
peer support program is that incarcerated individuals are not given
access to phones and computers that would even allow for the delivery
of tele health services in any form” [25].
Issues with access are not localized to program services, however.
Interviewees mentioned general reduced access to food supply as
a barrier faced by those with low social capital. A PSS shared the
following: “People I’ve worked with have always struggled with
obtaining food stamps and following through certain obligations that
they need to, to get these services.” This shifts the program participant’s
focus from recovery efforts to basic survival, further limiting access to
peer support due to participant’s inability to attend meetings. This
compounded with the loss of interpersonal relationships central to
the program itself greatly reduces willingness to participate.
Outreach services have also been severely reduced secondary to
the COVID-19 pandemic, and disproportionately affect those with
low social capital. In reference to the reduction of services themselves,
A PSS mentioned the following: “I don’t know if it’s just because no
contact or we haven’t been able to perform as many outreach services
as of late, but I’ve noticed at least on my end, that there’s been a pretty
significant drop off of participants coming through and signing up for
services.” In reference to how this affects those with low social capital,
A PSOE mentions the difficulty in providing resources to individuals
who are homeless during the COVID-19 pandemic: “It’s harder to get
somebody into housing, because COVID has diverted a lot of housing
money towards individuals who work part time and have been laid
off. We are utilizing a lot of resources, to take care of ensuring that
rent protections are put in, when they’re laid off through no fault
of their own, which means that less individuals are accessing those
things who don’t have jobs.”
Systemic Issues:
Interviewees (n=3) mentioned systemic barriers that further
impede the delivery of medication - assisted peer support. Community
spread of COVID-19 within prisons, compounded with the lack of
telehealth resources for peer support and other recovery services
cause a positive feedback loop for individuals with low social capital
who are becoming more and more disadvantaged in their journey
to recovery. A PSOE states:“Individuals are being arrested for petty
crimes, small time drug possession, that are still being introduced into
the jail and are being exposed to COVID through community spread,
and they’re trying to isolate it as best as possible when realistically
had they adopted a lot of these tactics that we’re using, with the rest
of our community participants much farther back instead of trying
to intentionally bar access for inmates from telehealth services, they
could have potentially prevented an outbreak from even happening
because there would be less contact.”This compounded with race inequities puts minorities at a
higher disadvantage when it comes to accessing recovery services. A
PSOE stated the following:“They explicitly impact black and brown communities at a higher rate than they do white communities because
incarceration and the crimes that are listed on the exemption list, we
know that black and brown people are charged or arrested for those
crimes at a higher rate than white people despite data showing an
equal rate of committing of crimes across white people to black and
brown people.”
In addition, interviewees mentioned that community participation
is imperative for keeping individuals involved in medication - assisted
peer support. Without this collaboration, individuals are not being
motivated or held accountable for their recovery efforts. A PSOE
mentioned the following:“It’s more difficult to stay in contact with
individuals who are suffering from opioid use disorder if they’re not
being referred back into the community program, which is where
most of the navigation of care would take place upon release.”
Discussion
Two main themes, the effect of COVID-19 and the effect of
low social capital, were found to greatly impede the delivery of
medication - assisted peer support services and substance abuse
recovery resources. Within these issues, specific subthemes were
identified that uphold these barriers: time and space constraints,
reduced efficacy in communication and case management, almost
complete loss of interpersonal activities, reduced outreach services
to those disproportionately affected by COVID-19 and low social
capital, and, in the case of prison inmates, restriction of necessary
resources altogether. These results are consistent with other findings
in literature that highlight the impact of COVID - 19 on the separate
delivery of medication - assisted treatment and peer support [13].
There is little fidelity in delivering adequate services in “15-minute
sessions,” especially via video systems. One area of improvement
is increasing frequency and duration of these meetings, resuming
the building of interpersonal relationships and support systems for
program participants. This may require hiring of additional service
leaders to accommodate their rising responsibilities since the
COVID-19 pandemic began. Increasing frequency of meetings can
also improve the case management issues identified; specifically: more
frequent meetings between service leaders and program participants
can increase the amount of case-relevant information being relayed
to case managers and supervisors who can make important decisions
regarding a participants’ care.
Interviews conducted with peer service leaders indicate the
necessity of initiatives that address the lack of face - to - face
interaction and outreach services that occur secondary to the COVID
- 19 pandemic. The Wellness Recovery Action Plan (WRAP), a
personalized and structured wellness process, was implemented as a
substitute for live interaction with peer leaders and has been shown
to have positive outcomes for recovery participants [6]. Service
outreach has been greatly reduced secondary to COVID-19, and
this disproportionately affects individuals with low social capital (ex.
incarcerated or previously incarcerated individuals and individuals
experiencing homelessness). Recent studies have shown that the
creation of solutions for these individuals would increase program
enrollment, reduce the chance of relapse or overdose, and reduce
the possibility of these individuals, who are also at a higher risk of
being arrested for petty drug-related crimes, from entering prison systems where there is a risk for community COVID-19 infection
and lack of telehealth services and other recovery services [8]. The
crux of medication - assisted peer support services is its creation of
interpersonal connections for those who otherwise have none. With
the services that foster these connections currently running at a small
fraction of what once was, participants from lower socioeconomic
backgrounds are struggling to see the point of continuing in the
program, especially when other more pressing issues, like accessing
food, shelter, and safety are at the current forefront of their day-to-day
[25-27]. Further studies can elucidate the effect a lack of interpersonal
connections has on individuals of minority groups.
Limitations
The results of this case study are limited by the structure of the
study, sample size, and potential for bias. The interview structure of
this study allows the risk for error bias based on interview questions
and interviewee response. The relatively small sample size (N=6)
is a limitation for making generalized conclusions. However, this
small sample size is typical of case studies, especially those studies
of new ideas, and may be transferable to other community recovery
organizations (Bacchetti et al., 2011). Accounting for these limitations,
important conclusions are identified from the results of this study.
Conclusion
During the COVID - 19 pandemic, obstacles have arisen
throughout the healthcare field. One specific demographic that
has been negatively affected is the opioid recovery community. In
the opioid recovery community, the distribution and efficacy of
medication - assisted peer support programs have been severely
reduced by COVID - 19 and social capital related factors - and often
a combination of the two. This empirical study has led us to identify
targeted areas of improvement to optimize medication - assisted peer
support and other recovery resources. Further studies are necessary
to create specific solutions and to identify additional areas of these
recovery programs that are being negatively affected. These can in
turn lead to the improvement of medication - assisted peer support,
aiding those battling substance abuse and helping to reduce relapses
and drug - related injuries during this pandemic. Ideally, these
targeted improvements would result in far-reaching and lasting
improvements in the system that would benefit the substance use
recovery community beyond the COVID - 19 era.