Journal of Addiction & Prevention
Download PDF
Review Article
Inpatient Addiction Medicine Consultation on Readmission Rates and Length of Stay
Amer Raheemullah*, Huiqiong Deng, Lief E. Fenno and Anna Lembke
Department of Psychiatry and Behavioral Sciences, Stanford University,
Stanford, CA 94305, USA
*Address for Correspondence:
Raheemullah A, Department of Psychiatry and Behavioral Sciences, Stanford
University, Stanford, CA 94305, USA; E-mail: raheem@stanford.edu
Submission: 06 April, 2022
Accepted: 03 May, 2022
Published: 06 May, 2022
Copyright: © 2022 Raheemullah A, et al. This is an open access article
distributed under the Creative Commons Attribution License, which
permits unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited.
Abstract
Background: Patients with substance use disorders (SUDs) make
up nearly one-third (29.1%) of hospitalized patients in the United
States. They also have double the 30-day readmission and emergency
department visit rates compared to those without SUDs. The Centers
for Medicare and Medicaid Services has penalized hospitals $3 billion
for higher 30-day readmission rates. Addiction medicine consultation
has been shown to reduce 30-day readmission. However, their impact
on Hospital length of stay remains largely unknown.
Methods: We compared admissions of repeat utilizer patients at
Stanford Hospital with an ICD-10 diagnosis of a SUD and compared the
30-day readmission rate and length of stay in patients with and without
an addiction medicine consult.
Results: The 30-day readmission rate and average LOS was 10.4%
and 6.11 days for those that received a consult compared to 25.3%
and 6.16 days in those that did not. Medicaid and Medicare patients
made up 70.3% and 19.0% of the population, and addiction medicine
consultation was found to be associated with a 61.4% and 69.5%
reduction in 30-day readmission rate, respectively.
Conclusion: In patients with SUD who have a history of repeated
hospital utilization, admissions that received an addiction medicine
consult are associated with a decrease in 30-day readmission rate
with no increase in length of stay compared to admissions that do not
receive an addiction medicine consult.
Keywords
Addiction consult service; 30-day readmission rate; Length
of stay; Inpatient addiction medicine
Introduction
Patients with substance use disorder (SUD) make up nearly onethird
(29.1%) of hospitalized patients in the United States (Smith et al.,
2015). They also have double the 30-day readmission and emergency
department visit rates compared to those without SUDs (Walley et al.,
2012). For Medicaid patients, alcohol-related disorders rank 3rd in
all-cause 30-day readmission rate, while substance-related disorders
rank 9th (Hines et al., 2014). Ninety-day readmission rates in SUD
Medicaid beneficiaries approach one in two patients at 48.3% (Reif
et al., 2017).
The 30-day readmission rate is an increasingly important
variable since the Centers for Medicare and Medicaid Services (CMS)
established the Hospital Readmissions Reduction Program (HRRP).
This program was designed to reduce readmissions by financially
penalizing hospitals with high 30-day readmission rates in Medicare
patients with certain conditions, and it has already penalized hospitals
billions of dollars (Wadhera et al., 2020). There is concern other
payers will follow suit and some policymakers have pushed for the
HRRP to be expanded to cover all conditions.
Similarly, hospital length of stay (LOS) is another top metric
closely monitored by health care systems in order to improve hospital
efficiency, costs, and quality of care. LOS can be prolonged by
frequently consulting specialists in the hospital, and this can increase
complexity and costs in patient care (Stevens et al., 2020). Although hospital-based addiction medicine consultation has been shown to
reduce 30-day readmission rates (Wakeman et al., 2020), their impact
on LOS remains largely unknown. We conducted a retrospective
descriptive analysis of SUD patients seen by the addiction medicine
consult service at an academic hospital to understand how consultation
influenced hospital length of stay and 30-day readmission rates.
Hospitalized patients seen in consultation by dedicated addiction
medicine consult services receive specialty addiction medicine
management including but not limited to pharmacotherapy,
psychotherapy, and linkage to treatment programs for SUDs. This
type of consultation has been shown to increase the number of days of
abstinence in the first month after hospital discharge, reduce addiction
severity, improve engagement with addiction treatment, and decrease
mortality (Wakeman et al., 2017; Englander et al., 2019). Stanford
Hospital launched an inpatient addiction medicine consult service
in fall of 2018. Prior to launching the full-time service, addiction
medicine consultation was provided from outpatient providers on an
ad-hoc basis to attempt to address the needs of hospitalized patients
with SUDs. This ad-hoc service soon grew from 1-2 consults a week
to 1-2 consults a day, and eventually grew large enough to justify a
dedicated inpatient addiction medicine service. The success of the
service in the first year was key to its continued growth. As such, this
study focused on the impact of the service in its first year of operation.
Methods and Findings
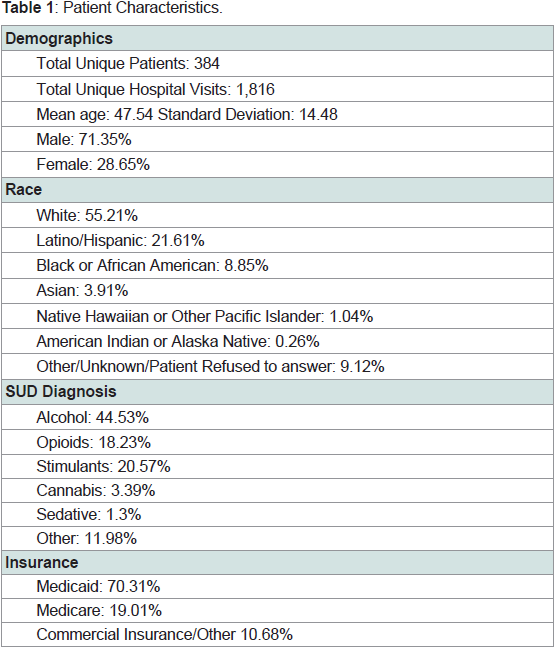
We analyzed admissions of repeat utilizers at Stanford Hospital
with an ICD-10 diagnosis of a SUD who had their first addiction
medicine consult from December 1, 2018 through December 1, 2019
(Table 1). To assess the effect of consultation on repeat readmissions,
our analysis focused on repeat utilizers (used the hospital 2 or more
times before their first consult). In this population, we compared the
30-day readmission rate and average length of stay in patients with
and without an addiction medicine consult during the year following
their first consult. We also conducted a subgroup analysis in the
Medicare and Medicaid population.
Per our hospital protocol, patients with six hospital visits in a
six month period are considered high utilizers and are assigned a complex care manager to focus on reducing readmissions. Since this
confounding intervention was designed to reduce readmissions, we
removed high utilizers from our analysis. This study was approved by
the Stanford University Institutional Review Board.
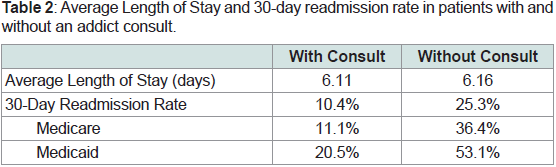
In the repeat utilizer population described, 73.4% of hospital
admissions contained a consult. The 30-day readmission rate was
10.4% for those that received a consult compared to 25.3% in those
that did not (Table 2). The average LOS was 6.11 days in those with a
consult compared to 6.16 days in those without.
Table 2: Average Length of Stay and 30-day readmission rate in patients with and
without an addict consult.
In the Medicare population, 58.8% of hospital admissions
received a consult and the 30-day readmission rate was 11.1% in
those that received a consult compared to 36.4% in those that did not.
In the Medicaid population, 65.8% of hospital admissions received
a consult, and the 30-day readmission rate was 20.5% in those that
received a consult compared to 53.1% in those that did not.
Discussion
Addiction medicine consult service interventions include
pharmacotherapy and psychotherapy. They occur alongside the
medical care received for a patient’s primary admitting diagnosis and
within the time constraints of acute hospital care. This study suggests
that addiction medicine consultation reduces 30-day readmission rates without increasing hospital length of stay. The slight decrease in
LOS associated with an addiction medicine consult may be attributed
to interventions routinely used to help manage behavioral issues,
taper pain medications, treat withdrawal, coordinate safe treatmentoriented
discharge plans, and thus expedite discharge.
Considering CMS’s focus on reducing high readmission rates,
this study also adds to the literature by looking specifically at the
Medicaid and Medicare population, which made up 70.3% and 19.0%
of the population, and showed consultation was associated with a
61.4% and 69.5% reduction in 30-day readmission rate, respectively.
There are limitations of our study. We only included readmissions
to our hospital. Data from a single institution limits generalizability.
It is also possible that the patients were readmitted to other hospitals,
which were not included in the current analysis. Secondly, without
randomization it is not possible to ascertain whether the observed
reduction in readmission rates were due to addiction medicine consult
service intervention as opposed to other factors, such as additional
care from repeated admissions. Thirdly, the 30-day readmission
rate is not the only measure of hospital utilization, and increases in
readmission rates at this time point can precede long-term decreases
in overall hospital utilization. Future studies are needed to examine
90-day readmission rates or other measures. Fourthly, it is not
clear what components of addiction medicine consult services are
most effective. Future research should parse out what aspects of an
addiction medicine consult service lead to better outcomes, as well
as whether the added cost of an addiction medicine consultation is
outweighed by reduced 30-day readmission rates that do not increase
length of stay.
Conclusion
In patients with SUD who have a history of repeated hospital
utilization, admissions that receive an addiction medicine consult
are associated with a decrease in 30-day readmission rate with no
increase in length of stay compared to admissions that do not receive
an addiction medicine consult.