Journal of Addiction & Prevention
Download PDF
Research Article
Prevalence of Cigarette Smoking and its Associated Factors among Parents at Misrak Bedawacho District, Southern Ethiopia
Terefe Markos Lodebo1*, Kifle Woldemichael Hajito1, Tsegaye Tewelde Gebrehiwot1 and Tariku Bokile Achicha2
- 1Department of Epidemiology, Institute of Health, Jimma University, Jimma, Ethiopia, Africa
- 2Department of Public Health, College of Medicine and health sciences, Madawalabu University, Bale Robe, Ethiopia, Africa
*Address for Correspondence: Terefe Markos Lodebo, Principal investigator, Department of Epidemiology, Institute of Health, Jimma University, Jimma, Ethiopia, Africa, Tel: 0910024501; E-mail: teremark997@gmail.com
Citation: Lodebo TM, Hajito KW, Gebrehiwot TT, Achicha TB. Prevalence of Cigarette Smoking and its Associated Factors among Parents at Misrak Bedawacho District, Southern Ethiopia. J Addiction Prevention. 2017;5(1): 9.
Copyright: © 2017 Lodebo TM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 5, Issue: 1
Submission: 07 March, 2017 | Accepted: 12 April, 2017 | Published: 20 April, 2017
Keywords:
Cigarette smoking; Parents; Prevalence
Abstract
Background: Cigarette smoking poses a huge challenge worldwide. More specifically, parental smoking had an influence on smoking practice of the young generations. There is limited data on the smoking habits of parents in developing countries. The aim of the study was assessed of prevalence of cigarette smoking and associated factors among parents in Misrak Bedawacho district, Southern Ethiopia.
Methods: A community based Cross sectional study was conducted from March 15 to April 15, 2016. Multi stage sampling technique was used to select 640 study participants. Data was collected using a pretested structured interviewer administered questionnaire. It was entered in to Epi-data and analyzed using SPSS. In addition, of descriptive statistics for describing data and multivariate logistic regression analyses was used to identify associated factors.
Results: Six hundred forty parents participated in the study yielding response rate of 100%. The current smoking prevalence was 23.6% (95% CI: 20.5, 27.3). Males were more likely to smoke compared to females (AOR = 2.6, 95% CI: 1.5, 5). Age group (20 - 39)(AOR = 19; 95% CI: 9.1, 39) and 15 - 19 (AOR = 3.7, 95% CI: 1.4, 10) were more likely to smoke compared to the age groups (40 – 59 years). Formerly married parents were more likely to smoke compared to currently married parents (AOR = 1.6, 95% CI: 1.2 - 2.8). Illiterate (AOR = 5; 95% CI: 1.5; 16.8) and high school complete (AOR = 3, 95% CI: 1.4, 10.4) were more likely to smoke compared to college and above category. Daily laborers were more likely to smoke compared to farmers (AOR = 3.8, 95% CI: 1.7, 9), Participants categorized as Poorest (AOR = 4.3, 95% CI: 1.43, 17.6) and poorer (AOR = 3.1, 95% CI: 1.13, 12.6) were more likely to smoke compared to richest category. Participants categorized as little knowledge category were more likely to smoke compared to highly knowledgeable (AOR = 5, 95% CI: 1.06 - 25). Khat chewer were more likely to smoke compared to those who were not khat not chewer (AOR = 2.2; 95% CI: 1.2, 4). Those, who having smoking peer (AOR = 2, 95% CI: 1.2, 3.5) were more likely to smoke compared to those do not have smoking peers.
Conclusion: This study found that a prevalence of current cigarette smoking among parents in the Misrak Bedawacho district is high. Furthermore, this study reveals that parental current cigarette smoking is strongly associated with illiteracy, low socioeconomic status, daily labour, having little knowledge, khat chewing practice and having peers smoking. Generally, these factors should be considered for further prevention of smoking practice. Therefore, concerned bodies should inform the health consequences of tobacco use.
Abbreviations
AOR: Adjusted Odds Ratio; CDC: Communicable Disease Control; CI: Confidence Interval; CVD: Cardio-Vascular Disease; CHD: Congestive Heart Failure; DHS: Demographic Health Survey; EDHS: Ethiopian Health Survey; EPHA: Ethiopian Public Health Association; ETS: Exposure to Tobacco Smoke; FCTC: Frame Work Convention for Tobacco Control; GATS: Global Adult Tobacco Survey; NCD: Non-Communicable Disease; OR: Odds Ratio; SSA: Sub-Saharan African Countries; SHS: Secondhand Smoking; SNNPR: South Nations Nationalities Peoples Region; SPSS: Statistical Package for Social Science; USA: United States of America; WHO: World Health Organization
Background
Cigarette smoking refers to the practice of inhalation of the gases and hydrocarbon vapors generated by slowly burning tobacco in cigarettes [1]. Smoked forms of tobacco include various kinds of cigarettes, cigars and pipes. In some countries of the world other forms like pipe smoking, chewing and sniffing are highly practiced. But, cigarette smoking, particularly manufactured cigarettes, is by far the main form of tobacco smoked globally [2]. In fact, in addition to commercial type of cigarette, hand-rolled cigarettes are more common in rural areas and used by older people [3]. The smoke which comes from cigarettes contains more than 7000 chemicals, including nicotine with hazardous adverse effects on almost every organ in the body of smokers as well as of nonsmokers exposed to second hand smoke (SHS) [4]. According to the WHO, almost 63% of all deaths are caused by NCDs, for which tobacco use is one of the greatest risk factor [5].
Tobacco use is a major public health concern and one of the strongest lifestyle behaviors associated with the risk of cardiovascular disease (CVDs). It is anticipated that by 2030, over 8 million people will die annually due to tobacco smoking related health problems, of which 80% will occur in low and middle income countries [6]. Besides the direct costs of treating tobacco-related diseases, economic productivity is lost due to preventable illness and premature deaths among users. Additionally, unnecessary expenditures to purchase tobacco also contribute to household poverty and malnutrition, particularly within resource limited settings [7]. Despite its negative effects, the number of smokers is increasing, there are over one billion smokers worldwide and about a third of the world’s population, aged 15 years above, were smokers [2,8]. Studies from abroad revealed that the magnitude of smoking among parents was in the range of 29.8% to 33.6% of maternal smoking and 37.9% to 45.2% of paternal smoking [9,10].
Currently, tobacco use in Africa is increasing like Latin America and Asia [11]. Ethiopia is one of the countries in Sub-Saharan Africa shares the burden of tobacco epidemics [12]. Parental smoking practice needs attention, because families are especially vulnerable to SHS at home. However, this issue has not been addressed yet among parents in Ethiopia. Beyond health effects that are caused by cigarette smoking among themselves and to others; it increases the risk of house fires, diversion of income, likelihood of children’s tobacco addiction [13]. Despite such a great impact of parental smoking, previous studies in the country gave due emphasis for cigarette smoking on specific age groups such as students, youths, town. While, magnitude of parental smoking or associated factors in the community setting among parents in Ethiopia as well as in the study was not well studied. This study aimed to assess the magnitude of cigarette smoking and associated factors among parents in the community.
Methods
Study setting
The study was carried out in Misrak Bedawacho district in Hadiya zone, Southern Ethiopia. The study site is 335 kilometers away from the capital city of Ethiopia, Addis Ababa. According to 2013 census, the district has a total population of 213,846 and 43,642 households. The district has six urban and thirty three rural Kebeles (the smallest administrative unit in Ethiopia) (Figure 1).
Study design
Community based cross sectional study was employed.
Participants: A sample of 640 parents at least having one child and residing in more than six months from Misrak Bedawacho district, Southern Ethiopia.
Inclusion criteria: Permanent Parents in the selected Keble’s.
If no parents in the family folder, head of household was included.
Exclusion criteria: Mentally and chronically ill and unable to speak parents were excluded.
Adults/household heads who did not experience child bearing or child caring.
Individuals who had stayed for less than six months.
Sampling procedure: Sample size was calculated using single population proportion formula by considering 50% proportion of Parental cigarette smoking, 95% confidence interval, 5% margin of error and 1.5 design effect and by adding 10% of non-response rate a total of 640 parents was required. Parents were selected by using multistage sampling techniques from urban and rural Kebeles. At the first stage by using simple random sampling: two and ten Kebeles were selected from urban and rural Kebeles respectively. Then after, at second stage households were selected. Totally twelve Kebeles having 12,839 households (parents) were identified from the family folder at the Health Post of each respective selected Kebele. The lists of households in each selected Kebeles were identified. The total sample size of 640 was distributed for selected Kebeles proportionally. Then after, by using Simple Random Sampling the final samples were taken (Figure 2).
Measurement: Data was collected using a pre-tested semi-structured interviewer administered questionnaire. Also, twelve Health professionals (6 Bachelor degrees and 6 diplomas) were selected for Data collection and two supervisors were assigned. The lists of final sample including the names of Kebele, identification number and random number were prepared for each Kebeles and given to supervisors and data collectors. Only one parent was chosen by lottery method for interview if both parents are available at the time of interview. If both parents were absent for a temporary period, repeated visit was undertaken. One day training was given for data collectors. Next, the questionnaire was pre-tested on 5% of the sample (32 parents) before the actual data collection days in unselected Kebeles in the district (Jaarso kutube, shone 04).
A Smoking questionnaire was adapted from GATS questionnaires and also, other literatures were used to assess factors associated with smoking [14]. It is a standardized international questionnaire with carefully chosen questions to assess tobacco use and also enable comparison of data across settings.
The current smoking status was measured through asking respondents “have you smoked part or all of a cigarette every day or any day within 30 days preceding the study, those parents answering ‘Yes’ to the question are classified as current smoker and those parents answering ‘No’ classified as a current non-smoker for further analysis [15].
Knowledge of health effects of cigarette smoking
The level of knowledge about the effects of smoking was measured using six core questions [14]. Each of them has three responses (Yes, No and don’t know). Each correct answer for the smoking-related health effects were represented by ‘Yes’ and other two options classified as incorrect answer (No, don’t know). “Based on what you know or believe, does smoking tobacco cause serious illness? Does cigarette smoking cause lung cancer, heart disease? Does Smoking affect children’s health? Does Smoking harm smokers and non-smokers? Do Smoking increases health expenditure?” Correct responses were given a score 1 and incorrect responses as 0. The six items was summed to form the knowledge index with values ranging from 0 to 6. The knowledge index was re-coded for analysis by categorizing the values to make an aerated knowledge index with values ranging from 0 to 1 = 1 as little knowledge, 2 to 3 = 2 as some knowledge, 4 to 6 = 3 as good/high knowledge.
Family smoking status: The respondents answering ‘Yes’ to the question ‘did your father/mother smoke in your lifetime?’ were considered to have had a family smoking history in their life time.
Peer smoking status: The respondents answering ‘Yes’ to the question ‘Does your close friend/relatives smoke?’ were considered as to currently having a smoking best friend/relatives [16].
The wealth index was constructed by using principal component analysis done with variables extracted from EDHS 2011. The sample was then divided into quintiles from one (lowest) to five (highest). A single asset index was developed for the whole sample; indices were not prepared for urban and rural populations separately. Accordingly, first quintile (poorest), second quintile (poorer), third quintile (middle), fourth quintile (rich) and fifth quintile (richest) was calculated [17].
Data Processing and Analysis
Data was entered using Epi data version 3.1 and exported to IBM SPSS version 20.0 for analysis. After cleaning data for inconsistencies and missing values, descriptive analysis was done such as percentages, frequency distributions and mean and measures of dispersion (SD) was used for describing data. For further analysis smoking status recoded in to 1 for Current smokers and 0 for Current Non-smokers (Former smokers and Never smokers). Binary Logistic regression analysis was used to identify factors associated with current smoking. All variables associated with current cigarette smoking in the Binary logistic regression with a p-value ≤ 0.25 were entered together into a multivariable logistic regression by using the backward method. The degree of association between independent and dependent variables was assessed using odds ratio with 95% confidence interval. P-value < 0.05 was considered as statistically significant. Multicollinearity was checked. The Hosmer - Lemeshow goodness-of-fit statistic was used and the model had a p-value > 0.05 which proved the model was good.
Ethical Consideration
Ethical clearance was obtained from the Institutional Review Board (IRB) of Jimma University College of health sciences. Permission letter was obtained from the Misrak Bedawacho district after the objectives of the study was explained. Verbal consent was sought from selected participants to confirm willingness to participate in the study before the interview. Privacy and confidentiality was ensured throughout the process of the study. The study participants were ensured that refusal to consent or withdrawal from the study would not alter or put at risk their access to health care.
Results
Socio-demographic characteristics
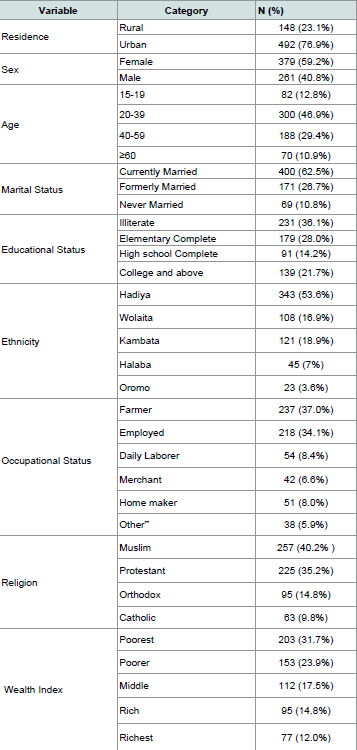
A total of 640 parents were interviewed for the study, all were involved in the study yielding a response rate of 100%. This due to training of data collectors, strict supervision and repeated visits of closed houses. The mean age of the study participants in this study was 38.80 (SD + 12.1) years. A majority of parents 300 (46.9%) were 20 - 39 years old. About 82 (12.8%) of the participants were 15 - 19 years old. By their marital status, four hundred (62.5%) were married and 69 (10.7%) were single. About educational status of the parents, 231 (36.1%) were illiterate and 139 (21.7%) were college and above. Four hundred ninety two (76.9%) of the respondents were from rural areas. The Majority of respondents 237 (37.0%) were farmers and 163 (25.5%) were government employees. Regarding Wealth index poorest group accounted for 203 (31.7%) and highest group accounts 77 (12%) (Table 1).
Table 1: Socio-demographic characteristics of the study participants in Misrak Bedawacho district, Southern Ethiopia, March 15 to April 15, 2016 (n = 640).
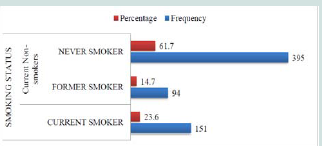
Cigarette Smoking status
Among study Participants, near to one fourth of them were current cigarette smokers and 94(14.7%) were former smokers and the never smoker accounts for 395 (61.7%) (Figure 3)
Figure 3: Smoking status among parents in Misrak Bedawacho district, Southern Ethiopia, March 15 to April 15, 2016 (n = 640).
Factors influencing current smoking practice
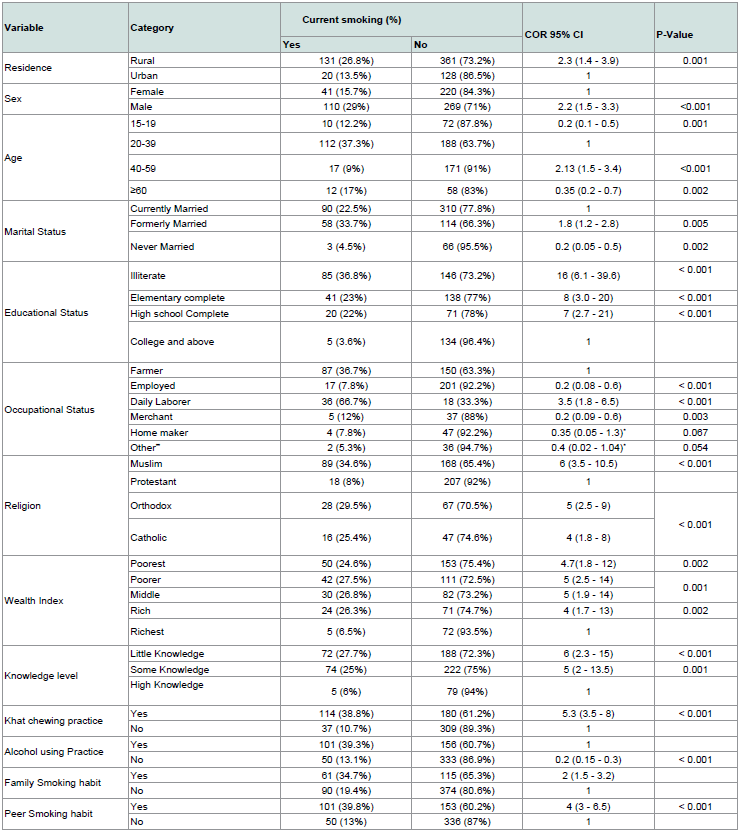
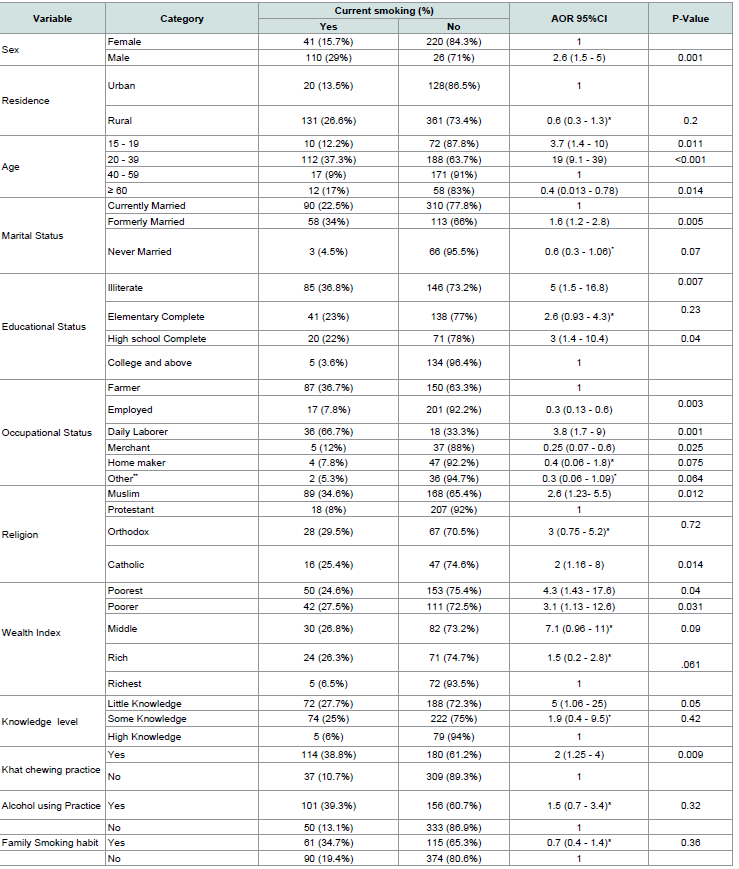
Factors influencing current smoking in binary logistic regression: Current cigarette smoking assessed for its association among its selected variables/factors. Accordingly, the result indicated that residence of parents was positively associated with current smoking (COR = 2.3; 95% CI: 1.4, 3.9) meaning that the odds of smoking among rural parents were two-fold increase compared to urban parents. Similarly, smoking among males two-fold times more likely compared to females (COR = 2.2; 95% CI: 1.3, 3.3) (Table 2).
Table 2: Binary logistic regression analysis to show factors associated with cigarette smoking among parents in Misrak Bedawacho disrict, Southern Ethiopia, March15 to April 15, 2016.
Factors influencing current smoking in multivariate logistic regression: Accordingly, the variables like sex, age, educational status, marital status, occupation, religion, wealth index, khat chewing practice and peer/friends’ smoking status were significantly associated with current cigarette smoking at p-value < 0.05.
In this study the result showed that parents whose ages were between 20 - 39 years 19 times more likely to smoke than those parents between 40 - 59 (AOR = 19, 95% CI: 9.1, 39) and above 60 years 60% times less likely to smoke (AOR = 0.4; 95% CI: 0.013, 0.78). Similarly, age groups 15 - 19 were 3.7 times more likely to smoke than 40 - 59 age groups (AOR = 3.7, 95% CI: 1.4, 10). In this study the finding revealed that male were 2.6 times more likely to smoke than females (AOR = 2.6; 95% CI: 1.5, 5). The result showed that parents whose marital status were formerly married were 1.6 times more likely to smoke than currently married parents (AOR = 1.6; 95% CI: 1.2, 2.8). Parents whose religion was Muslim and Catholic were 2.6 times more likely smoke than whose parents, which were protestants (AOR = 2.6; 95% CI: 1.23, 5.5). In line with this, parent who were catholic two times more likely smoke than protestants (AOR = 2, 95% CI: 1.16, 8) (Table 3).
Discussion
The main objective of this study was to determine the prevalence of cigarette smoking and associated factors among parents. Accordingly, this study revealed that the prevalence of current smoking was 23.6%. Similarly illiterates, having low knowledge, poorest economically, daily laborers, male, middle age category, formerly married (divorced and widowed), khat chewing practice and peer smoking were strong predictors of current cigarette smoking among parents. The magnitude of cigarette smoking is on a rise despite the fact that numerous scientific studies had reported a morbidity and mortality associated with it.
The findings of this study showed that the overall self-reported prevalence of cigarette smoking was 23.6% (95% CI: 20.5, 27.3) with 17.2% (95% CI: 14.3, 20.1) for males and 6.4% (95% CI: 4.5, 8.3) for females. This high magnitude might be due to availability of hand rolled cigarettes and tobacco growers in the area.
The finding from this study was consistent with the study done in 23.9% Halaba, 28% Eastern Ethiopia, 27.1% Malawi, 28.5% Madagascar, 23.19% Bangladesh [15,18-21]. This finding result was much higher than a national study done in Ethiopia 3.1% (8.1%) in males and 0.8% in females), Butajira 4.4% (11.8% male and 0.8% female), Gilgel Gibe research field center Jimma (9.4%) [17,22,23]. But lower than study conducted in Jimma town (35.5%), Amhara region (57%), 31.8% China and national study conducted in Madagascar (48.9% in males and 10.3% in females) [24-26]. This discrepancy could be due to difference in study setting, socio cultural differences, level of study (national and Woreda level), time of the study and the way of outcome measurement.
In fact, the cigarette smoking prevalence in the current study population is much higher than the national average of 4.4% [27]. Interestingly, it is nearly consistent or comparable to reports from countries such as Kenya 22.9%, Tanzania 21%, and Tunisia 30.4% [28].
Previous studies in the countries as well as abroad indicated that the prevalence of smoking was higher in rural area than urban areas [15,17,26]. Specifically, this study revealed that the prevalence of cigarette smoking in urban 3.1% and in rural 20.5% but, residence was not significant in this study.
In this study the result indicated that males had higher odds to use tobacco as compared to females. Similarly, most studies in Ethiopia and other African countries have shown that cigarette smoking is associated with male gender [17,1824]. In Ethiopia, cigarette smoking in females is condemned by the community and results in stigma and discrimination. Furthermore, familial relationships, including care and family related activities may protect females from involving in tobacco use.
It was also found that respondents with lowest wealth index/poorest and second/poorest wealth index were more likely to smoke and respondents with higher wealth index were least likely to smoke.This study identified that the poorest/poorer groups of the population were more likely to smoke cigarettes as compared to the richest quintile group. This finding is consistent with studies [17,21,27].Why poor or poorest people smoke is attributed to lack of awareness about the adverse effects of smoking or the stresses of poverty causing individuals to take up smoking as a coping mechanism and availability of locally prepared cigarettes [29].
Educational status was a strong predictor of cigarette smoking. In this study illiterate or uneducated parents were more likely smoking habit than educated parents. This consistent with other studies reported nationally and internationally [15,17,22,26,30]. This association between smoking and lack of education has been reported in other studies in Pakistan, Bangladesh, and India [31]. This might be due to lack of awareness about the health effects of tobacco products.
In this study, the result showed that Compared to the age group (20 - 39 years), odds ratios were lower in almost all age groups. This study is consistent with studies done middle income countries but, inconsistent with previous studies elsewhere reported that an oddity of cigarette smoking was found to increase among older age groups [17,18,21,22,32].
The discrepancies due to study setting, culture, level of exposure to substances, since they are less likely to engage in income generating activities, so this forced them dependency on family to buy cigarettes. But the onset of the earning age group is found to smoke more. The increase in prevalence among them might have indication about their job stress or family stress. Unless effective tobacco control measures are soon strengthened, the future disease burden in Ethiopia will probably be influenced by the high level of smoking in young male adults in the age group 20 - 39 years. Therefore, targeting cessation in these age groups would be extremely important as a component of overall policy initiatives for reducing tobacco use prevalence [22,33]. Also, the result of this finding indicated that youngest age group (15 - 19) has been found to smoke tobacco. This is in line with other studies [17,18]. Similarly, this study found a lower prevalence of smoking nearly 1.3% among those aged 60 years and above, which is consistent with reports from other Asian countries [34,35]. This may be due to the reason that older people have less pressure and more time to accept health information and medical advice and confront smoking-related diseases, thus increasing the health consciousness following physical decline with age. Also, in this finding the middle age groups or working age were more likely engaged in smoking. Tobacco use-related deaths tend to occur during the most productive middle-age years; therefore, impacting the economy of the entire nation. This suggests a potential target group for future tobacco control campaigns.
There was a statistically significant difference in tobacco use across different religious groups. Islamic religion followers were sixfold more likely to smoke cigarettes compared to protestant faith followers. This finding mirrors a number of studies conducted in Ethiopia and abroad [17,21,26,27,36,37]. So that these Islamic communities resided in these areas cultivates tobacco plants and prepare for local markets and exposed to these cigarettes. This could also be the reason why this study found that those Islamic religion followers have had higher odds of using cigarettes. Similarly, catholic religion followers were two times more likely smoke than protestant faith followers. This is consistent with other reports [17].
Separated or divorced adults were more likely to be smokers than married ones. This finding is consistent with those reported by others [26,38,39]. This can be explained by marriage protection theories, because married people have greater economic, social, and psychological support, while separated or divorced people have emotional distress that may lead them to become smokers for comfort. The odds of tobacco use among formerly married individuals were higher as compared to never married individuals. This study consistent with other study [17]. This could be due to the fact that formerly married individuals might use tobacco to relieve their stress or loneliness. On the other hand, divorce could be one of the social consequences of tobacco use. Tobacco use might cause conflict among couples and result in divorce.
In this study the result indicated that occupation type was associated with cigarette smoking. The odds of smoking fivefold increase among day labor workers than those who are employed parents and this finding was also reported in European and Asian populations [17,21,26,27,32,40,41]. A possible explanation is that labor workers have a lower socioeconomic status, more physical pressure, and psychosocial and emotional problems. Daily labor workers with a low level of education and income had a lower level of socioeconomic status. This group of people had financial stress and unhealthy lifestyles, and they lacked health care.
In this study the result showed that the odds of smoking were higher among parents with little knowledge categories. This is consistent with studies [2,22,42]. An inverse relationship was observed for level of knowledge and cigarette use; as the level of knowledge increased, the odds of tobacco use decreased. This due to awareness of health effects, organizations may influence smoker in order not to smoke within their organization. Also, there was relatively low level of knowledge about the health effects of smoking among respondents; their awareness about the health effects of cigarette smoking was deficient. Thus, it necessitates well designed intervention in order to minimize the overall effects of the current practice especially onto the new generation.
This study also found that the khat chewing practice was twofold increases the odds of current cigarette smoking among parents. This is consistent with other studies [15,43]. Since most khat chewers use cigarette to enhance their level of excitement, the proportion of smokers observed among khat chewers were high. Even though smokers studied were parents, certainly their current action will contribute for future increment of the youth’s smoker at community, school and universities in the area. Since the existence of motivating factors such as the presence of smoker, peer smoking or family member at home was found strong predictor variables for high prevalence of cigarette smoking.
Having a smoking close friend was strongly associated with participants’ own smoking. The development of nicotine dependence and smoking habit is linked to social influence of family and friends. Accordingly In this study the result indicated that the odds of smoking among parents who had smoking friends or families two times more likely than the counterpart. Other studies done also reports the same findings [31,44]. The smoking behavior of a close friend is significantly associated with participants’ own smoking behavior in adulthood. The impact of this association is much greater than the impact of smoking family members. This should be taken into consideration in attempts to prevent smoking initiation or continuation.
Limitation and Strength of the Study
Nevertheless, as the study has employed, self-reporting as a proxy measure for the study of smoking status, it is liable to self-report bias which can underestimate the prevalence of the smoking under study. Underreporting could happen due to social desirability bias. The finding of this result should be interpreted in light of these limitations. Despite these limitations, however, this study has enormous public health implications and strengths. The major strengths of our study include; high response rate, the coverage of men and women, and the coverage of both rural and urban areas. Since, a standardized questionnaire employed that enabled to compare to other studies conducted in similar settings. Some of the social influences on smoking were studied in this population. Population based nature of the study alongside with the use of random selection of study participants are the strengths of this study.
Conclusion and Recommendations
In conclusion, this study found that considerably high prevalence of self-reported current cigarette smoking among parents in the Misrak Bedawacho district. Furthermore, this study reveals that cigarette smoking is strongly associated with illiteracy, male, low socioeconomic status (poorer and poorest), age group 15 - 19 and 20 - 39, daily labour working, formerly married, having little knowledge, khat chewing practice and having peer smoking. Giving it as a public health priority, WHO FCTC should be strengthened. In addition, a nationwide campaign is needed to educate parents about the health risks of smoking cigarette. Setting out strategy to control locally prepared hand rolled cigarettes in the markets and focusing on tobacco growers in the community. Low education could be a proxy to low awareness and consumer information on tobacco products. As Public health practitioners we should inform the adverse health consequences of tobacco use.
Ethics and Consent
Ethical clearance was obtained from the Ethical Review Committee (ERC) of Jimma University College of health sciences. Permission letter was obtained from the Misrak Bedawacho district after the objectives of the study was explained. Verbal consent was sought from selected participants to confirm willingness to participate in the study before the interview. Privacy and confidentiality was ensured throughout the process of the study. The study participants were ensured that refusal to consent or withdrawal from the study would not alter or put at risk their access to health care.
Acknowledgement
We would like to acknowledge College of Medicine and Health Sciences of Jimma University for giving grant for this study. We gratefully acknowledge study participants who enthusiastically participated in this study for their time and patience during data collection.
References
- Mosby (2013) Mosby’s medical dictionary (9th edn). Elsevier Health Sciences, pp. 1984.
- Giovino GA, Mirza SA, Samet JM, Gupta PC, Jarvis MJ, et al. (2012) Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet 380: 668-679.
- Cargnin MC, Echer IC, Ottobelli C, Cezar-Vaz MR, Mantovani VM (2015) Prevalence and factors associated with smoking among tobacco growers in southern Brazil. Rev Bras Enferm 68: 518-523.
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health (2014) The health consequences of smoking-50 years of progress: a report of the surgeon general. Centers for Disease Control and Prevention, Atlanta (GA), USA.
- World Health Organization (2014) World Health Statistics, Geneva, Switzerland.
- World Health Organization (2013) World No Tobacco Day. Geneva, Switzerland.
- World Health Organization (2013) Why tobacco is a public health priority? Geneva, Switzerland.
- Appelman, Y, van Rijn BB, Ten Haaf ME, Boersma E, Peters SA (2015) Sex differences in cardiovascular risk factors and disease prevention. Atherosclerosis 241: 211-218.
- Maloney E, Hutchinson D, Burns L, Mattick R (2010) Prevalence of and characteristics associated with persistent smoking among Australian mothers and fathers: findings from the longitudinal Study of Australian Children (LSAC). J Fam Stud 16: 165-175.
- Tautolo el-S, Schluter PJ, Taylor S (2011) Prevalence and concordance of smoking among mothers and fathers within the Pacific Islands families study. Pac Health Dialog 17: 136-146.
- Nigussie T, Gobena T, Mossie A (2013) Association between khat chewing and gastrointestinal disorders: a cross sectional study. Ethiop J Health Sci 23: 123-130.
- World Health Organization (2011) Non-communicable diseases country profiles 2011, WHO global report, Geneva, Switzerland, pp. 209.
- Winickoff JP, Berkowitz AB, Brooks K, Tanski SE, Geller A, et al. (2005) State-of-the-art interventions for office-based parental tobacco control. Pediatrics 115: 750-760.
- Global Adult Tobacco Survey Collaborative Group (2010) Global Adult Tobacco Survey (GATS): core questionnaire with optional questions, version 2.0. Centers for Disease Control and Prevention, Atlanta, USA.
- Ketema T, Alemayehu E, Ambelu A (2015) Exploration of pattern of use of khat and tobacco among residents of Halaba Kulito town, southern Ethiopia. J Biol Chem Res 32: 374-386.
- Saari AJ, Kentala J, and Mattila KJ (2014) The smoking habit of a close friend or family member-how deep is the impact? A cross-sectional study. BMJ Open 4: e003218.
- Lakew Y, Haile D (2015) Tobacco use and associated factors among adults in Ethiopia: further analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Public Health 15: 487.
- Reda AA, Kotz D, Biadgilign S (2013) Adult tobacco use practice and its correlates in eastern Ethiopia: a cross-sectional study. Harm Reduct J 10: 28.
- Mahfouz MS, Alsanosy RM, Gaffar AM, Makeen A (2014) Tobacco use among university students of Jazan region: gender differences and associated factors. Biomed Res Int 2014: 279231.
- Sreeramareddy CT, Pradhan PM, Sin S (2014) Prevalence, distribution, and social determinants of tobacco use in 30 sub-Saharan African countries. BMC Med 12: 243.
- Sultana P, Akter S, Rahman MM, Alam MS (2015) Prevalence and predictors of current tobacco smoking in Bangladesh. J Biostat Biom Appl 1: 102.
- Palipudi KM, Gupta PC, Sinha DN, Andes LJ, Asma S, et al. (2012) Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS One 7: e33466.
- Alemseged F, Haileamlak A, Tegegn A, Tessema F, Woldemichael K, et al. (2012) Risk factors for chronic non-communicable diseases at gilgel gibe field research center, southwest Ethiopia: population based study. Ethiop J Health Sci 22: 19-28.
- Jima SB, Tefera TB, Ahmed MB (2015) Prevalence of tobacco consumption, alcohol, khat (Catha edulis) use and high blood pressure among adults in Jimma town, southwest Ethiopia. Sci J Public Health 3: 650-654.
- Tegegne AS (2014) Assessing public awareness about the health effects of nicotine and cigarettes using negative binomial regression. Sci J Appl Math Stat 2: 60-65.
- Li Z, Yao Y, Han W, Yu Y, Liu Y, et al. (2015) Smoking prevalence and associated factors as well as attitudesand perceptions towards tobacco control in northeast China. Int J Environ Res Public Health 12: 8606-8618.
- Mwenda SN, Wanjoya AK, Waititu AG (2015) Analysis of tobacco smoking patterns in Kenya using the multinomial logit model. Am J Theor Appl Stat 4: 89-98.
- Pampel F (2008) Tobacco use in sub-Sahara Africa: estimates from the demographic health surveys. Soc Sci Med 66: 1772-1783.
- Hanifi SM, Mahmood SS, Bhuiya A (2011) Smoking has declined but not for all: findings from a study in a rural area of Bangladesh. Asia Pac J Public Health 23: 662-671.
- Hosseinpoor AR, Parker LA, Tursan d'Espaignet E, Chatterji S (2012) Socioeconomic inequality in smoking in low-income and middle-income countries: results from the World Health Survey. PLoS One 7: e42843.
- Alam AY, Iqbal A, Mohamud KB, Laporte RE, Ahmed A, et al. (2008) Investigating socio-economic-demographic determinants of tobacco use in Rawalpindi, Pakistan. BMC Public Health 8: 50.
- Schoenmaker N, Hermanides J, Davey G (2005) Prevalence and predictors of smoking in Butajira town, Ethiopia. Ethiop J Health Dev 19: 182-187.
- Norberg M, Lundqvist G, Nilsson M, Gilljam H, Weinehall L (2011) Changing patterns of tobacco use in a middle-aged population: the role of snus, gender, age, and education. Glob Health Action 4.
- Suzuki K, Sato M, Tanaka T, Kondo N, Yamagata Z (2010) Recent trends in the prevalence of and factors associated with maternal smoking during pregnancy in Japan. J Obstet Gynaecol Res 36: 745-750.
- Sreeramareddy CT, Ramakrishnareddy N, Harsha Kumar H, Sathian B, Arokiasamy JT (2011) Prevalence, distribution and correlates of tobacco smoking and chewing in Nepal: a secondary data analysis of Nepal Demographic and Health Survey-2006. Subst Abuse Treat Prev Policy 6: 33.
- Doku D, Darteh EK, Kumi-Kyereme A (2013) Socioeconomic inequalities in cigarette smoking among men: evidence from the 2003 and 2008 Ghana demographic and health surveys. Arch Public Health 71: 9.
- Garrusi B, Nakhaee N (2012) Religion and smoking: a review of recent literature. Int J Psychiatry Med 43: 279-292.
- Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M (2012) Socioeconomic status and smoking: a review. Ann N Y Acad Sci 1248: 107-123.
- Nejjari C, Benjelloun MC, Berraho M, El Rhazi K, Tachfouti N, et al. (2009) Prevalence and demographic factors of smoking in Morocco. Int J Public Health 54: 447-451.
- Cai L, Wu X, Goyal A, Han Y, Cui W, et al. (2012) Patterns and socioeconomic influences of tobacco exposure in tobacco cultivating rural areas of Yunnan Province. BMC Public Health 12: 842.
- Idris BI, Giskes K, Borrell C, Benach J, Costa G, et al. (2007) Higher smoking prevalence in urban compared to non-urban areas: time trends in six European countries. Health Place 13: 702-712.
- Rahman MS, Mondal MN, Islam MR, Rahman MM, Hoque MN, et al. (2015) Determinant factors of tobacco use among ever-married men in Bangladesh. Drug Healthc Patient Saf 7: 77-85.
- Kumar R, Salve H, Misra P (2014) Determinants of tobacco use and perception, attitude about an antitobacco act in rural Haryana, North India. Int J Med Public Health 4: 367-370.
- Reda AA, Moges A, Yazew B, Biadgilign S (2012) Determinants of cigarette smoking among school adolescents in eastern Ethiopia: a cross-sectional study. Harm Reduct J 9: 39.