Journal of Addiction & Prevention
Download PDF
Research Article
*Address for Correspondence: Jakob Linnet, Research Clinic on Gambling Disorders, Aarhus University Hospital, Nørrebrogade 44, Building 30, DK-8000 Aarhus C, Denmark, USA, E-mail: jakolinn@rm.dk
Citation: Linnet J, Pedersen AS. Waiting Time Increases Risk of Attrition in Gambling Disorder Treatment. J Addiction Prevention. 2014;2(2): 4.
Copyright © 2014 Linnet J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 2, Issue: 2
Submission: 01 December 2014 | Accepted: 19 December 2014 | Published: 22 December 2014
Waiting Time Increases Risk of Attrition in Gambling Disorder Treatment
Jakob Linnet1-3* and Anders Sune Pedersen1,2
- 1Research Clinic on Gambling Disorders, Aarhus University Hospital, Denmark
- 2Center of Functionally Integrative Neuroscience, Aarhus University, Denmark
- 3Division on Addiction, Cambridge Health Alliance, Cambridge,MA, USA
*Address for Correspondence: Jakob Linnet, Research Clinic on Gambling Disorders, Aarhus University Hospital, Nørrebrogade 44, Building 30, DK-8000 Aarhus C, Denmark, USA, E-mail: jakolinn@rm.dk
Citation: Linnet J, Pedersen AS. Waiting Time Increases Risk of Attrition in Gambling Disorder Treatment. J Addiction Prevention. 2014;2(2): 4.
Copyright © 2014 Linnet J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 2, Issue: 2
Submission: 01 December 2014 | Accepted: 19 December 2014 | Published: 22 December 2014
Abstract
Attrition is a well known problem in psychotherapeutic treatment. Patients with addiction have high attrition rates, and it is therefore important to identify factors that can improve completion rates in addiction. Here, we investigated the influence of waiting time as a predictor of treatment completion in gambling disorder. We compared 48 gambling disorder sufferers with a 56% completion rate (21 non-completers and 27 completers). Binomial logistic regression analysis showed that waiting time from initial contact to the first session with a therapist was a significant predictor of risk of attrition: longer waiting times were associated with increased risk of attrition. Age, gender, or comorbidity was not associated with an increased risk of attrition. These data suggest that gambling disorder sufferers benefit from fast access to treatment, and that longer waiting time increases the risk of attrition.Keywords:
Gambling disorder; Treatment; Addiction; Attrition; Waiting time; ComorbidityIntroduction
Attrition is a well known problem in psychotherapeutic treatment [1]. Patients suffering from substance use disorder [2,3] and gambling disorder [4-7], have high attrition rates ranging from approximately 30-50%. Therefore, it is important to identify factors that might be associated with attrition and retention in the treatment of addiction. Candidate factors for attrition in addiction include: comorbidity, demographics, contact with therapist, and waiting time for treatment. Araujo et al. [2] found that comorbidity of anxiety and depression in substance use disorder was not associated with treatment retention or attrition in a group of 148 patients in an inpatient substance abuse detoxification program. Ross et al. [8] reported similar findings using the Symptom Check List-90-R (SCL90-R) in a group of 308 male and 106 female patients with moderate-to-severe substance abuse problems. Condelli et al. [9] found that two factors predicted treatment retention in a group of 753 substance use disorder patients: (1) the interviewers’ predictions of whether clients would stay long enough in the program to benefit from treatment; and (2) whether patients had spent most of their time with large groups of people, as opposed to small groups or alone, before the onset of the disorder. Finally, Albrecht et al. [3] found that immediate entry into treatment was significantly associated with completion in a group of 10,661 pregnant women being admitted to substance abuse treatment. However, other studies find that waiting time is not associated with retention in treatment of substance use disorder [10]. To date only little attention has been paid to factors contributing to attrition and retention in gambling disorder treatment. Identification of factors contributing to attrition rates may have important implications for clinical practice and development of treatment methods. In this study we investigated the role of waiting time and comorbidity as possible predictors of attrition in gambling disorder treatment.Methods and Materials
ParticipantsThe cohort consisted of 48 gambling disorder sufferers with a 56% completion rate (21 non-completers and 27 completers). Patients were recruited through the Research Clinic on Gambling Disorders (RCGD) and the Danish Gambling Disorder Treatment Network (a nationwide Danish treatment collaboration). The inclusion criteria for patient referral were: 18-75 years of age; problems with controlling gambling; symptoms that are disruptive to the person’s life and have persisted for at least two weeks; and sufficient proficiency in Danish. The exclusion criteria were: current or past psychotic, bipolar disorder or other severe psychiatric disorder; current suicidal risk; current moderate or severe alcohol or substance use disorder; diminished cognitive functions; and pregnancy.
Diagnosis and Comorbidity
Patients were assessed by clinical psychologists using the Structured Clinical Interview for DSM-IV (SCID-I) [11] and the Structured Clinical Interview for Pathological Gambling (SCI-PG) [12], which are diagnostic assessment tools for Axis-I disorders (e.g.,gambling disorder, affective disorders, psychotic disorders, anxiety disorders, and substance use disorders). The SCID-I and SCI-PG for DSM-IV are the most recent SCID versions.
Treatment
Patients were treated using an evidence based treatment protocol developed by the Research Clinic on Gambling Disorders from Robert Ladouceur’s method, which is one of the best documented treatment methods of gambling disorder [4,6,7,13-16]. The method consists of 12 weekly sessions of Cognitive-Behavioral Therapy (CBT), which covers: motivation; behavioral modification in high risk gambling situations; identification and reorganization of cognitive biases and erroneous perceptions; and relapse prevention. Patients received individual treatment, and were evaluated on craving and gambling control.
Statistical analysis
We used Welch’s t-test to test for group differences on age, gender, comorbidity, craving, gambling control, days waiting for treatment, number of treatment sessions, and days in treatment. We used a binomial logistic regression model for treatment completion using waiting time as the sole explanatory variable. The predictive power of the model was computed using leave-one-out cross-validation. In terms of data completeness, we note that two completers and six non-completers had missing data on gambling control, while one completer and six non-completers had missing data on craving.
Results
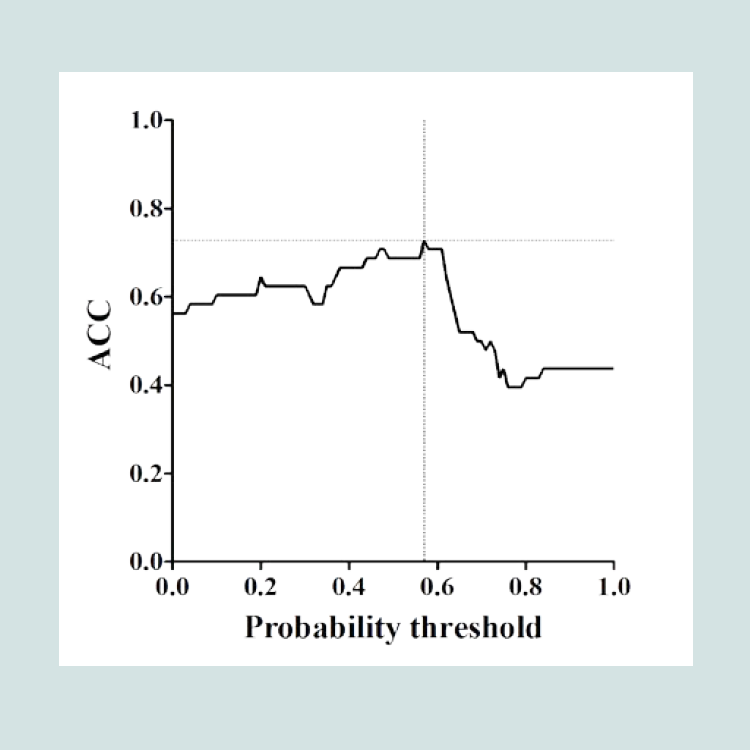
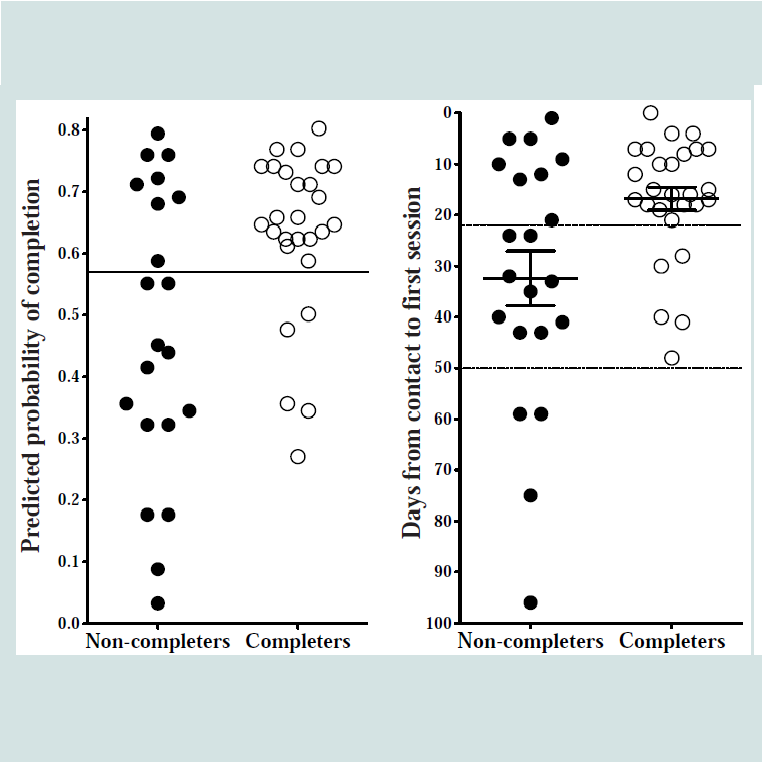
Table 1 shows that patients completing treatment waited significantly fewer days for treatment, t(27.05) = -2.66, p ≤ 0.01, and had significantly more days in treatment, t(41.22) = 2.62, p ≤ 0.01, and treatment sessions, t(44.13) = 5.45, p ≤ 0.001, compared to noncompleters. The two groups did not differ in age, gender distribution and presence of comorbidity.The binomial logistic regression analysis showed that the waiting time from initial contact to the first session with a therapist significantly predicted treatment completion (z = -2.44, p < 0.02); longer waiting times were associated with increased risk of noncompletion. In contrast, comorbidity did not significantly predict completion rates. The model had an optimal level of classification of 72.9% at the probability threshold of 0.57 (see Figure 1).Figure 2A shows the distribution of completers and noncompleters in the model. Patients above the solid line are predicted to complete treatment, while patients below the solid line are predicted to be non-completers. The model’s sensitivity was 73.3% (22 of 30 predicted completers above the solid line were accurately classified), and a specificity of 72.2% (13 of 18 predicted non-completers below the solid line were accurately classified). The overall classification accuracy is 72.9% (35 of 48). Figure 2B shows that patients who spoke with a therapist within 22 days had a 73.3% completion rate (above the dashed line), while waiting more than 50 days to speak with a therapist reduced the completion rate to 0% (below the dotted line).
Figure 2: Predicted probability of completion and days waiting for treatment in completers and non-completers.
A. Classification accuracy of predicted treatment completion. The maximum classification accuracy between completers (white circles) and non-completers (black circles) is obtained at the probability threshold of 0.57 - indicated by the horizontal solid line. The model predicts that patients above the line complete treatment, while patients below the line do not complete treatment. The y-axis shows the models predicted probability of completion.
B. Days waiting for treatment. Patients who are predicted to complete treatment wait less than 22 days for treatment (above dashed line). The y-axis shows the number of days waiting for treatment. Mean and Standard Error Mean (SEM) for the waiting time are shown for completers and noncompleters.
Discussion
Waiting time was found to be a significant predictor of gambling disorder treatment completion. Gambling disorder sufferers, who completed treatment, waited significantly fewer days for starting treatment than gambling disorder sufferers, who did not complete treatment. Gambling disorder sufferers who started treatment within 22 days (n = 30 of 48) had a 73.3% completion rate, compared to an overall 56% completion rate. Gambling disorder sufferers who waited more than 50 days (n = 4 of 48) for treatment had a 0% completion rate. These data suggest that gambling disorder sufferers benefit from fast access to treatment, which is associated with an improved completion rate. In contrast, longer waiting times are associated with increased risk of attrition.The overall attrition rate of 56% reported here, is similar to attrition rates reported in other studies of gambling disorder treatment. For instance, Sylvain et al. [4] found that 29 out of 40 patients (73%) completed treatment, while 11 (27%) dropped out; Ladouceur et al. [6] found that 35 (53%) out of 66 patients completed treatment, while 31 (47%) dropped out; and Ladouceur et al. [7] found that 61 (69%) out of 89 patients completed treatment, while 28 (31%) dropped out. Attrition rates in gambling disorder thus seem to vary from approximately 30-50%. None of these studies investigated factors associated with attrition rates, which is understandable, because they focused on the effect of gambling disorder treatment. However, it underscores the facts that only little attention has been paid to factors contributing to attrition, and the need to investigate factors of attrition in order to improve treatment retention and completion.
Our data indicate that waiting time is a significant factor in attrition, while symptom severity of gambling and comorbidity did not predict completion rates. The implication of this finding is that patients who wait longer for treatment are at risk for not completing treatment, which in turn makes it conceivable that the risk of attrition might be reduced by the waiting time for starting treatment. This may be done by, for instance, increasing treatment personnel, or reallocating resources toward faster intake assessment and visitation for treatment.
The present study was carried out in a naturalistic treatment setting, where all patients were thoroughly screened through inclusion and exclusion criteria and diagnostically assessed for gambling disorder and comorbidity. The group division was a natural consequence of patients completing or not completing treatment, and the results are therefore highly relevant for clinical practice. Therefore, it was not necessary to randomize patients.
Non-completion was not a result of patients seeking treatment elsewhere while waiting for treatment, since patients had at least one session with a therapist (patients in treatment rarely seek help elsewhere). However, a limitation in the data is that they did not include patients who were never in contact with a therapist (patients needed at least one session to be included).
Another limitation was, that it was not possible to evaluate treatment effect, since most patients in the non-completion group did not complete post treatment measures. Therefore, treatment completion was only evaluated based on intake measures. Thirdly, several factors may have affected longer waiting time for patients, e.g., periods with higher influx of patients (e.g., around major sports events or holidays) or the responsiveness of patients. In addition, some patients can be difficult to get in contact with, thereby resulting in delay in booking appointments and hence delay the start of treatment. Therefore, further research should investigate possible factors for delay in entering treatment. Fourth, other factors, such as symptom severity of gambling disorder or comorbidity might affect treatment outcome, and further research should investigate those factors as well. Fifth, the selection criteria in our sample might differ from other studies of gambling disorder and substance use disorder. The present treatment setting is an outpatient treatment center. Therefore, only patients with mild to moderate symptom severity are included in the treatment. It is possible that completion rates in patients with more severe comorbidity (e.g., severe depression, psychotic disorders or severe comorbid substance use disorder) are less affected by waiting time, and more affected by severity of comorbid psychopathology. Finally, while our cohort was of comparable size with previous studies of gambling disorder, the sample size was smaller than that of previous studies in substance use disorder. Therefore, the findings should be replicated in a larger sample.
In conclusion our data suggest that waiting time for starting treatment is a risk factor of attrition in gambling disorder treatment, and that appropriate measures to reducing waiting time, can improve patient retention and completion rates, and thereby treatment efficiency. These findings are relevant for clinical practice and for improving treatment methods in gambling disorder.
Acknowledgement
This study was supported by funding from the Ministry of Health grant number 1001326, 121023 and 1301936; by a research grant from bwin. Party services; and by a research designated donation from Better Collective A/S. The authors declare that they have no competing financial interests.References
- Bergin AE, Garfield SL (1994) Handbook of psychotherapy and behavior change NY Wiley.
- Araujo L, P Goldberg, Eyma J, Madhusoodanan S, DD Buff, et al. (1996) The effect of anxiety and depression on completion/withdrawal status in patients admitted to substance abuse detoxification program. J Subst Abuse Treat 13: 61-66.
- Albrecht J, Lindsay B, Terplan M (2011) Effect of waiting time on substance abuse treatment completion in pregnant women. J Subst Abuse Treat 41: 71-77.
- Sylvain C, Ladouceur R, Boisvert JM (1997) Cognitive and behavioral treatment of pathological gambling: a controlled study. J Consult Clin Psychol 65: 727-732.
- Stinchfield R, Winters KC (2001) Outcome of Minnesota's gambling treatment programs. J Gambl Stud 17: 217-245.
- Ladouceur R, Sylvain C, Boutin C, Lachance S, Doucet C, et al. (2001) Cognitive treatment of pathological gambling. J Nerv Ment Dis 189: 774-780.
- Ladouceur R, Lachance S, Fournier PM (2009) Is control a viable goal in the treatment of pathological gambling? Behav Res Ther 47: 189-197.
- Ross HE, Cutler M, Sklar SM (1997) Retention in substance abuse treatment. Role of psychiatric symptom severity. Am J Addict 6: 293-303.
- Condelli WS, De Leon G (1993) Fixed and dynamic predictors of client retention in therapeutic communities. J Subst Abuse Treat 10: 11-16.
- Addenbrooke WM, Rathod NH (1990) Relationship between waiting time and retention in treatment amongst substance abusers. Drug Alcohol Depend 26: 255-264.
- First M, R Spitzer, M GibbonW (1995) Structured clinical interview for the DSM-IV Axix I disorders (SCID I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute.
- Grant JE, Steinberg MA, Kim SW, Rounsaville BJ, Potenza MN (2004) Preliminary validity and reliability testing of a structured clinical interview for pathological gambling. Psychiatry Res 128: 79-88.
- Tavares H, Zilberman ML, el-Guebaly N (2003) Are there cognitive and behavioural approaches specific to the treatment of pathological gambling? Can J Psychiatry 48: 22-27.
- Ladouceur R (2005) Controlled gambling for pathological gamblers. J Gambl Stud 21: 49-59.
- Ladouceur R, Lachance S (2007) Overcoming Pathological Gambling: Therapist Guide. Treatments That Work, ed. DH Barlow Oxford: Oxford University Press.
- Ladouceur R, Lachance S (2007) Overcoming Your Pathological Gambling: Workbook. Treatments That Work, ed. DH Barlow Oxford: Oxford University Press.