Journal of Addiction & Prevention
Download PDF
Research Article
*Corresponding author: Edmund Silins, National Drug and Alcohol Research Centre, University of New South Wales, Sydney, NSW, Australia, 2052, Tel: +61 2 9385 0333; Fax; +61 2 9385 0222; E-mail: e.silins@unsw.edu.au
Citation: Silins E, Bleeker AM, Simpson M, Dillon P, Copeland J. Does Peer-Delivered Information at Music Events Reduce Ecstasy and Methamphetamine Use at Three Month Follow-Up? Findings from a Quasi-Experiment across Three Study Sites. J Addiction Prevention. 2013;2(3): 8.
Copyright © 2013 Silins E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 1, Issue: 3
Submission: 17 October 2013 | Accepted: 25 November 2013 | Published: 27 November 2013
In the late 80s to early 90s, the popularity of ecstasy (MDMA; 3,4-methylenedioxymethamphetamine) began to increase and subsequently reports of ecstasy-related harm started to emerge [8,9]. Around this time, peer-led interventions specifically targeting ecstasy users were implemented in the United Kingdom (e.g., Crew 2000, Edinburgh) and later in Europe (e.g., Unity, Amsterdam), the United States (e.g., DanceSafe) and Australia (e.g., KIS, Sydney). Peer-led interventions are commonly seen as credible and cost effective ways to share information [10,11]. Studies of the influence of peer-led interventions have demonstrated that they can tap in to determinants of health such as knowledge, attitudes and selfesteem [12,20]. Additionally, peer-led interventions can provide information to those who are hard to reach through conventional methods [10]. Meta-analysis of 143 adolescent drug prevention programs indicated that peer-led interventions had positive health outcomes in knowledge, attitude, skills and behaviour [21]. Recent studies have also demonstrated substantial changes in knowledge and attitudes among those reached by the intervention [12,17,22,23]. Among injecting drug users, the success of numerous peer-led interventions is well documented [24,27]. Behavioural evaluations of peer-led HIV prevention for gay men have also been positive [28]. A systematic review of randomised clinical trials of peer-based interventions on health-related behaviours in adults found the evidence on their effectiveness was mixed [29]. The findings indicated that peer-based interventions facilitated important changes in health related behaviors such as physical activity, smoking, and condom use, but interventions aimed at increasing breastfeeding, medication adherence and women’s health screening did not produce significant changes [29].
The paucity of methodologically sound outcome evaluations has led to criticism of the effectiveness of peer-led interventions to change behaviours [2,30-33]. Therefore there is a need for more empirical research into their efficacy. Furthermore, few studies of peer-led interventions have specifically focused on ecstasy users. This group is far larger and differ markedly from other illicit drug users (e.g., injecting drug users) in age, education, employment and patterns of drug use [16,34] and therefore requires separate study.
At the time of the study, 8.9% of Australians had tried ecstasy and 3.5% reported recent (past year) use. Recent use was highest among 20-29 year olds (11.2%) with an increasing trend in use among 14-19 year old females [35]. The adverse health and psychological effects of ecstasy use include dehydration and hyperthermia related conditions, depression, memory problems, increased sexual risk-taking and impaired driving performance [36].
The broad aim of the study was to assess whether health messages can be effectively disseminated to ecstasy users at music events and do the messages impact on patterns of drug use. The specific hypotheses were that three months after the experimental group had received the peer led intervention using a unique ecstasy-related message: (1) the message would be recalled; and, (2) levels of ecstasy and methamphetamine use would be lower compared to the control group which did not receive the unique message. Ethical approval was granted by the Human Research Ethics Committee, University of New South Wales, Sydney, Australia.
Prior to study commencement, a total of 43 peer educators were recruited through established peer education organisations (e.g., KIS, Sydney). In addition to the organisations’ own training, peer educators received eight hours of drug and alcohol training specifically related to the study which included training about serotonin syndrome (i.e., symptoms, prevention). The training syllabus was delivered consistently in each location. On-going monitoring and supervision was provided. A process evaluation supported that peer educators had attained competency in drug knowledge and retained this six months after completing training.Eight to 12 specially trained peer educators and one to two researchers (in a supervisory role) attended each event. Peer educators wore special t-shirts which made them easily identifiable and worked from or near a dedicated stand. The stand was located inside the event, generally near areas where people congregated such as ‘chillout’ spaces and bars. People approached peer educators voluntarily. The study procedure involved: (1) a brief peer education session; (2) post-intervention interview; and, (3) three-month follow-up interview. The study procedure is illustrated in Figure 1 and described in detail below.
At experimental sites, in addition to usual drug-related information (provided as described above), peer educators promoted a unique ecstasy-related health message about serotonin syndrome. This message was not promoted at control sites. Serotonin syndrome is a life-threatening condition resulting from excessive stimulation of serotonergic receptors [37], such as that which can occur after excessive use of ecstasy and other stimulant drugs (e.g., methamphetamine) [38]. It is characterised by changes in body temperature, mental status and motor function. This message has never been used in Australian ecstasy-related harm reduction activities. It was important to use a unique message as participants who recalled it were highly likely to have received the information from peer educators and not from other sources. On the other hand, usual drug-related information (which is more general in nature) may have been received from sources such as the media, friends and internet, or was more likely to have been already known. Peer educators at experimental sites consistently delivered key information about serotonin syndrome (e.g., signs and symptoms) and how to prevent it (e.g., reducing use of ecstasy and methamphetamine, and reducing concomitant use). Additionally, pocket-size information pamphlets (available on request) and lanyards were printed with health messages about ways to prevent serotonin syndrome, and these were distributed. In each city, recruitment was completed at control sites before commencing at experimental sites to ensure only participants in the experimental group received the unique message.Immediately after the brief peer education session, individuals who wished to participate in the study were referred to other peer educators and asked screening questions. Inclusion criteria ensured participants were aged at least 18 years, had used ecstasy recently (at least once in the last 12 months), could provide contact information and had not participated in the study previously. Participation was voluntary and informed consent was obtained. Participants were not reimbursed for their time but went into a draw to win a personal music player. Immediately after participants were enrolled, faceto-face post-intervention interviews were administered by trained peer educators or completed under peer educator supervision. The ten minute, 30 item post-intervention questionnaire related to participant characteristics, information received from peer educators (e.g., what information did you receive from the peer educator you just spoke with? Have you heard this information anywhere before? How credible did you think this information was? Do you think the information received will change the way you use drugs?) and patterns of drug use (e.g., Have you recently used ecstasy/methamphetamine? In the last three months, how often have you used a combination of illegal drugs? Have you ever deliberately combine antidepressants/dexamphetamine with ecstasy?). A pre-intervention assessment was not included as this would have interfered with the normal ‘flow’ and delivery of peer education that is usual in this setting.The study used a two group (i.e., experimental/control) by two time-point (i.e., post-intervention/follow-up) design (Figure 1). To test for differences between independent groups (i.e., experimental and control groups), the Mann-Whitney U-test (a non-parametric equivalent of the t-test) was used for continuous skewed data, and the chi-square test for independence (Yates’ correction) was used for categorical data. To test for differences between related samples (i.e., post-intervention and follow-up groups), the Wilcoxon Signed Rank Test (a non-parametric alternative to the repeated measures t-test) was used for continuous skewed data, and the McNemar chi-square test for paired proportions was used for categorical data. Proportions and means were reported as relevant. Qualitative data was hand searched to identify themes. Analysis was conducted using SPSS for Windows, Version 15.0 (SPSS inc. 2005).
A total of 661 participants (n=278 Experimental, n=383 Control) were recruited. The experimental and control group were not significantly different in demographic or drug use characteristics except in relation to the recent use of ecstasy (Table 1). Several items related to specific patterns of drug use which are risk factors for serotonin syndrome. Among participants interviewed immediately post-intervention (n=513-580, depending on questionnaire item), approximately 14% (n=80) had ever used antidepressant drugs recreationally and about 8% (n=41) reported deliberately combining these drugs with ecstasy in their lifetime. Just under one-third (30%, n=168) had ever used methylphenidate (i.e., a psychostimulant often used for the treatment of attention-deficit/hyperactivity disorder) or dexamphetamine recreationally, and approximately 10% (n=50) reported deliberately combining these drugs with ecstasy in their lifetime.Intensive efforts to follow-up participants resulted in a followup rate of 54% among the experimental group and 52% among the control group. There were no significant differences in demographic characteristics and recent use of ecstasy and methamphetamine (at post-intervention) between participants followed-up and those lost to follow-up.Participants were interviewed immediately after engaging with peer educators (post-intervention) to assess their recall of the health messages delivered by peer educators. The most commonly recalled health message was about serotonin syndrome among the experimental group (64%), and about the importance of drinking enough water among the control group (35%) (Table 2). At three month follow-up, the two most commonly recalled health messages related to information about serotonin syndrome among the experimental group (46%), and the importance of drinking enough water among the control group (55%). Among the experimental group, 44% of participants who recalled information about serotonin syndrome at follow-up had previously recalled this information immediately post-intervention.
Participants at follow-up were also asked if they had heard the term ‘serotonin syndrome’ before, and where they had heard about it. The term serotonin syndrome was recalled by significantly more participants in the experimental (E) group than in the control (C) group (E:83%, C:53%, χ2=55.049, p< 0.01). When asked what they thought the term meant, responses related to the following main themes: ‘feelings of depression’ (E:1%, C:4%), ‘the wearing off of drugs’ (E:1%, C:5%), ‘feelings of happiness’ (E:4%. C:2%), ‘lack of serotonin’ (E:10%, C:24%), and ‘an excess of serotonin’ (E:46%, C:24%). Just over one-third (E:38%, C:41%) reported that they did not know. In keeping with a recognised definition for serotonin syndrome [37], responses which related to ‘an excess of serotonin’ were regarded as correct. The experimental group was significantly more likely than the control group to identify the term correctly (E:46%, C:24%, χ2=21.506, p< 0.01) and to report that they had heard it from peer educators at a dance party or music festival (E:85%, C:8%, χ2=122.718, p< 0.01).
Participants (n=661) scored the credibility of the information received on a five point scale from zero (not credible) to four (very credible). Generally, the information received was perceived as highly credible (mean score 3.6, SD 0.64). Participants thought the information would possibly (24%) or definitely (31%) change the way they use drugs. Typical responses related to reducing use, using in a safer way and greater consideration of the risks. About half (46%) reported that their patterns of drug use were not likely to change. Of the participants who recalled collecting pamphlets, a majority (55%) referred to the information later (i.e., when not intoxicated) and shared the information with others (68%). About one in five (17%) were prompted to seek out further information about drugs. Most (75%) would approach these peer educators again if they saw them at an event.
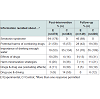
At three month follow-up, the mean days of ecstasy and methamphetamine use in the previous month and the recent use of methamphetamine significantly decreased in the experimental group and remained stable among the control group (Table 3). The recent use of ecstasy significantly decreased in both the experimental and control group. Further analysis revealed that the proportion which had decreased recent ecstasy use was not significantly different between the experimental and control group.
Most participants interviewed immediately post-intervention (E:60%, C:56%) and at follow-up (E:63%, C:62%) reported never or rarely using a combination of two or more drugs (possible response categories were never, rarely, sometimes, often and always). A minority reported often (E:11%, C:13%) or always (E:7%, C:6%) combining drugs. Overall, differences in polydrug use between the experimental and control group among participants interviewed post-intervention and follow-up were small and non-significant.
While it was encouraging that almost two-thirds of participants immediately post-intervention recalled the health message related to serotonin syndrome, this had subsequently decreased to just under half at three month follow-up. The simplicity of the message and peer educators’ confidence in message delivery are factors which may have influenced recall and correct identification of the term serotonin syndrome. This emphasises the need to use health messages which are simple to convey and comprehend, and reinforces the importance of providing high-quality peer educator training about the messages and delivery.
Interestingly, information about the importance of drinking enough water was widely recalled at follow-up but was not so commonly recalled immediately post-intervention. One explanation is that information received from other sources such as mainstream media, street press and the internet may have been confused with information received from peer educators. This is particularly likely as harm reduction messages targeting ecstasy users about water intake have been extensive, especially so since several widely publicised ecstasy-related deaths [39,40].
The information provided by peer educators was perceived as highly credible. The perceived credibility of the peer educator is important as it influences the persuasiveness of the message [41]. Therefore a more credible message is more likely to shift behavioural peer norms. About one-third of ecstasy users thought that the information provided would change the way they use drugs. Whether participants actually moderated their drug use as a result of the information provided by peer educators was difficult to determine, as discussed below. Nevertheless, this finding suggests that drug-related peer education can encourage reflection on patterns of drug use and contemplation of behaviour change. This left a substantial proportion that was not contemplating a change in drug using behavior. However, it can be peculated that there would have been light, intermittent users amongst them who were likely to perceive their drug use as non-problematic and, therefore, were not contemplating a behavior change at the time of the study.
It was encouraging that a majority of participants collected drug- and health-related information pamphlets from peer educators and referred to them at a later date. Pocket-sized resources of this kind are likely to be an effective way to reinforce the information provided by peer educators at events, particularly if the material is relevant and appealing to young people. Substantial proportions shared the information received with others, which demonstrates the potential flow-on effect of peer education. It was promising that the information received prompted people to proactively seek out further information (e.g., using the internet). KIS frequently report that ‘hits’ to their website, which provides alcohol and other drug information, increase after attending events (K. Devlin, personal communication). A large majority of ecstasy users would definitely approach the peer educators again if they saw them at an event which was an exceptionally encouraging finding.
Study findings suggest the peer led methodology used was effective in disseminating ecstasy-related health messages to citydwelling, twenty-something ecstasy users. However, caution must be used in generalizing findings to interventions which use other peerled methodologies and which target users of drugs other than ecstasy.Although changes in knowledge can be attributed to the peer led intervention with a degree of reliability, the same cannot necessarily be said for changes in patterns of drug use. It was encouraging that there was evidence of a decrease in involvement with ecstasy and methamphetamine three months after exposure to information from peer educators. While information provided by peer educators may partly account for the decrease in drug involvement, other explanations cannot be ruled out.
A positive outcome was that among the experimental group there was a significant decrease in the mean days use of ecstasy and methamphetamine and the recent use of methamphetamine, compared to the control group. Specific information about thepotential harms of ecstasy and methamphetamine use was part of the unique message promoted at experimental sites which may have contributed to this reduction.
A further positive outcome was the significant reduction in recent ecstasy use among the experimental and control group. Some information, such as the potential harms of ecstasy use, was part of usual drug-related information and part of the information provided on the unique message about serotonin syndrome which may account for lower levels of drug use in both groups. The result may, however, reflect regression toward the mean as recent ecstasy use post-intervention was relatively high, particularly in the experimental group.
It is also possible there may have been a seasonality effect ondrug use. This is likely to be more pronounced for the experimental group than the control group. Participants in the experimental group were recruited at music events held later in the ‘party’ season, and therefore, their level of drug involvement may have been lower than participants in the control group (who were recruited earlier in the ‘party’ season). While the reductions in drug involvement were promising, it is difficult to determine whether they were associated with the usual drug-related information received, the unique message about serotonin syndrome or other factors altogether.
The lifetime prevalence of patterns of drug use which are risk factors for serotonin syndrome was low but of concern. About one in thirteen participants had used antidepressant drugs with ecstasy – a potentially risky practice. Lifetime recreational use of methylphenidate or dexamphetamine was relatively common (30%), which is in keeping with other studies of ecstasy users in Australia [16].
Unfortunately, follow-up survey questions were not specific enough to identify changes in patterns of drug use which were risk factors for serotonin syndrome (e.g., combining antidepressant drugs with ecstasy). Furthermore, the prevalence of such patterns of use was generally very low among participants interviewed post-intervention, suggesting statistically significant differences would have been difficult to detect.
As with all studies, this study had several limitations. First, as the perceived expertise or credibility of the peer educator has been shown to enhance the effectiveness of peer education [41], such factors may have influenced outcomes among participants. All peer educators did, however, receive eight hours of training specifically related to the study which was delivered consistently in each city (in addition to their organisations’ own training). Furthermore, a process evaluation demonstrated their competency. Second, the follow-up rate of approximately 54% suggests that some caution should be applied when generalising findings to the wider population of ecstasy users, however, at post-intervention the demographic and drug use characteristics of those followed up were not significantly different to those lost to follow-up. Third, drug use was measured by self-report. While the reliability and validity of self-report of tobacco smoking behaviours among young adults have been called into question [42], studies among illicit drug users have shown that self-report is a reliable and valid measure of drug use [43]. Fourth, subjects had voluntarily interacted with peer educators, and therefore responses could represent those of ecstasy users who were more open to receiving information. Fifth, asking participants to recall the messages received by peer educators may have reinforced the messages and impacted on substance use. Sixth, surveys were conducted at events where alcohol and other drug use was likely which may have influenced responses. Participants were, however, interviewed during the early part of the event when intoxication was less likely.
Utilising a quasi-experimental design in a ‘real-life’ peer education setting, the study demonstrated that the methodology used was successful in disseminating information to ecstasy users. The information was recalled immediately post-intervention and after three months. While there was evidence of a decrease in drug involvement three months after the peer-led intervention, other explanations for the reduction cannot be ruled out. This paper indicates the complexities in teasing out the effects of peer-led interventions on patterns of drug use. The impact of peer-led interventions on drug use is, therefore, an area which needs to be addressed by additional, methodologically robust studies.
Findings highlight a number of important considerations for peerled education interventions. Fundamental to success is that the peerled peerled intervention is based on an established, evidence-based model (e.g., Unity, Amsterdam [44]). The health messages developed need to be unique, relevant and simple, and be supported with information flyers and merchandising which is popular with young people. To ensure proficiency, peer educators must receive high-quality training specifically related to the messages used. Additionally, providing only one or two drug-related health messages during a music event is likely to be much more effective than providing messages on a wide range of topics. Equally important is to conduct the intervention during the early part of the event, before participants become intoxicated. Lastly, securing access to appropriate dance events can be challenging, so peer education organisations which establish and maintain good relationships with the nightlife industry are more likely to succeed.
Funding was provided by the Australian Government Department of Health and Ageing, and the Australian Capital Territory Government Department of Health. The National Drug and Alcohol Research Centre at the University of NSW is supported by funding from the Australian Government.
Does Peer-Delivered Information at Music Events Reduce Ecstasy and Methamphetamine Use at Three Month Follow-Up? Findings from a Quasi-Experiment across Three Study Sites
Edmund Silins1*, Anne M Bleeker1, Melanie Simpson2, Paul Dillon2 and Jan Copeland2
- 1National Drug and Alcohol Research Centre, University of New South Wales, Sydney, NSW, 2052, Australia
- 2National Cannabis Information and Prevention Centre, University of New South Wales, Sydney, NSW, 2052, Australia
*Corresponding author: Edmund Silins, National Drug and Alcohol Research Centre, University of New South Wales, Sydney, NSW, Australia, 2052, Tel: +61 2 9385 0333; Fax; +61 2 9385 0222; E-mail: e.silins@unsw.edu.au
Citation: Silins E, Bleeker AM, Simpson M, Dillon P, Copeland J. Does Peer-Delivered Information at Music Events Reduce Ecstasy and Methamphetamine Use at Three Month Follow-Up? Findings from a Quasi-Experiment across Three Study Sites. J Addiction Prevention. 2013;2(3): 8.
Copyright © 2013 Silins E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 1, Issue: 3
Submission: 17 October 2013 | Accepted: 25 November 2013 | Published: 27 November 2013
Abstract
Background: Peer-led, ecstasy-related harm reduction efforts have become increasingly popular but their efficacy has rarely been rigorously evaluated.Methods: A quasi-experimental study design was utilised over three Australian study sites. The experimental group (n=278) received a unique ecstasy-related health message and usual drug-related information while the control group (n=383) received usual drug related information only. The hypotheses were that three months after the experimental group had received the peer led intervention using a unique ecstasy-related message: (1) the message would be recalled; and, (2) levels of ecstasy and methamphetamine use would be lower compared to the control group which did not receive the unique message.
Results: Participants recalled the unique message immediately post-intervention (T1, 64%) and after three months (T2, 46%). The information received was perceived as highly credible and encouraged reflection on patterns of drug use. Based on self-report, the mean days use of ecstasy (T1, 2.2; T2, 1.7; p< 0.01) and methamphetamine (T1, 1.3; T2, 0.3; p< 0.001) and the recent use of methamphetamine (T1, 51%; T2, 20%; p< 0.001) significantly decreased in the experimental group and remained stable in the control group. The recent use of ecstasy significantly decreased in both the experimental (T1, 82%; T2, 59%; p< 0.001) and control group (T1, 69%; T2, 56%; p< 0.01).
Conclusion: The peer education methodology used was an effective way to disseminate information to ecstasy users. Drug involvement decreased after the intervention but other explanations cannot be ruled out. The influence of peer-led interventions on drug use needs to be addressed by additional, methodologically robust studies. Findings highlight a number of important considerations for peer-led education interventions in relation to the use of an evidence based model, the development of health messages and peer educator training.
Keywords: Peer intervention; Young people and adolescents, Ecstasy (MDMA); Methamphetamine
Introduction
Peer-led interventions have become increasingly popular health promotion tools to reach young people. For several decades, peerled interventions that aim to reduce drug-related harm and improve sexual health have proliferated [1-3]. A principal reason is evidence of the strong influence of the peer group during adolescence. While an association with drug using peers is a strong predictor of adolescent drug use [4-6], the peer group can also have a restraining influence which can moderate risky behaviours such as drug use [7].In the late 80s to early 90s, the popularity of ecstasy (MDMA; 3,4-methylenedioxymethamphetamine) began to increase and subsequently reports of ecstasy-related harm started to emerge [8,9]. Around this time, peer-led interventions specifically targeting ecstasy users were implemented in the United Kingdom (e.g., Crew 2000, Edinburgh) and later in Europe (e.g., Unity, Amsterdam), the United States (e.g., DanceSafe) and Australia (e.g., KIS, Sydney). Peer-led interventions are commonly seen as credible and cost effective ways to share information [10,11]. Studies of the influence of peer-led interventions have demonstrated that they can tap in to determinants of health such as knowledge, attitudes and selfesteem [12,20]. Additionally, peer-led interventions can provide information to those who are hard to reach through conventional methods [10]. Meta-analysis of 143 adolescent drug prevention programs indicated that peer-led interventions had positive health outcomes in knowledge, attitude, skills and behaviour [21]. Recent studies have also demonstrated substantial changes in knowledge and attitudes among those reached by the intervention [12,17,22,23]. Among injecting drug users, the success of numerous peer-led interventions is well documented [24,27]. Behavioural evaluations of peer-led HIV prevention for gay men have also been positive [28]. A systematic review of randomised clinical trials of peer-based interventions on health-related behaviours in adults found the evidence on their effectiveness was mixed [29]. The findings indicated that peer-based interventions facilitated important changes in health related behaviors such as physical activity, smoking, and condom use, but interventions aimed at increasing breastfeeding, medication adherence and women’s health screening did not produce significant changes [29].
The paucity of methodologically sound outcome evaluations has led to criticism of the effectiveness of peer-led interventions to change behaviours [2,30-33]. Therefore there is a need for more empirical research into their efficacy. Furthermore, few studies of peer-led interventions have specifically focused on ecstasy users. This group is far larger and differ markedly from other illicit drug users (e.g., injecting drug users) in age, education, employment and patterns of drug use [16,34] and therefore requires separate study.
At the time of the study, 8.9% of Australians had tried ecstasy and 3.5% reported recent (past year) use. Recent use was highest among 20-29 year olds (11.2%) with an increasing trend in use among 14-19 year old females [35]. The adverse health and psychological effects of ecstasy use include dehydration and hyperthermia related conditions, depression, memory problems, increased sexual risk-taking and impaired driving performance [36].
The broad aim of the study was to assess whether health messages can be effectively disseminated to ecstasy users at music events and do the messages impact on patterns of drug use. The specific hypotheses were that three months after the experimental group had received the peer led intervention using a unique ecstasy-related message: (1) the message would be recalled; and, (2) levels of ecstasy and methamphetamine use would be lower compared to the control group which did not receive the unique message. Ethical approval was granted by the Human Research Ethics Committee, University of New South Wales, Sydney, Australia.
Method
Peer educators
Study sites
Data were collected between November 2006 and May 2007 at music festivals, dance events and nightclubs in three Australian cities (Sydney, Adelaide and Canberra). Events varied in size from 250 to over 30,000 attendees. Nine events were selected as control sites and nine were selected as experimental sites. Three control sites were chosen in each city and, where possible, were matched with experimental sites (Sydney, five sites; Adelaide, one site; Canberra, three sites) in relation to event size (e.g., number of attendees), music style (e.g., mainstream dance, 'techno’) and approximate age range of attendees. Additional experimental sites were selected in Sydney because of difficulty obtaining access to two appropriate sites in Adelaide.Procedure
Brief peer educator session
As people voluntarily approached the peer educators, peer educators engaged them in conversation. Often, peer educators asked people to complete a quiz as a way to start a conversation about drug use. Typically, the peer educator would provide usual drug-related information (e.g., the importance of drinking enough water, effects of drugs, potential harms of drug use and driving). The information was provided verbally, generally to everyone who approached the stand. Relevant pamphlets and other resources which supported the information provided by peer educators were freely available. The brief peer education session lasted approximately five to ten minutes.At experimental sites, in addition to usual drug-related information (provided as described above), peer educators promoted a unique ecstasy-related health message about serotonin syndrome. This message was not promoted at control sites. Serotonin syndrome is a life-threatening condition resulting from excessive stimulation of serotonergic receptors [37], such as that which can occur after excessive use of ecstasy and other stimulant drugs (e.g., methamphetamine) [38]. It is characterised by changes in body temperature, mental status and motor function. This message has never been used in Australian ecstasy-related harm reduction activities. It was important to use a unique message as participants who recalled it were highly likely to have received the information from peer educators and not from other sources. On the other hand, usual drug-related information (which is more general in nature) may have been received from sources such as the media, friends and internet, or was more likely to have been already known. Peer educators at experimental sites consistently delivered key information about serotonin syndrome (e.g., signs and symptoms) and how to prevent it (e.g., reducing use of ecstasy and methamphetamine, and reducing concomitant use). Additionally, pocket-size information pamphlets (available on request) and lanyards were printed with health messages about ways to prevent serotonin syndrome, and these were distributed. In each city, recruitment was completed at control sites before commencing at experimental sites to ensure only participants in the experimental group received the unique message.
Participant enrolment and post-intervention interview
Three-month follow-up interview
A 40 item follow-up interview was completed via telephone approximately three months later by independent research assistants. The follow-up questionnaire related to the peer education information received (e.g., What information did you receive from the peer educator at the event you attended about three months ago? What was the key message you took away?) and patterns of drug use.Statistical analyses
Results
Peer educator characteristics
Of the 43 peer educators, most were aged in their early twenties (mean age 22.1 years (SD 2.8, range 18-29 years)), female (70%) and born in Australia (81%). Just over one-third (37%) had completed year 12 and half (51%) had enrolled in or completed university.Participant characteristics
Follow-up
Information received from peer educators
Participants at follow-up were also asked if they had heard the term ‘serotonin syndrome’ before, and where they had heard about it. The term serotonin syndrome was recalled by significantly more participants in the experimental (E) group than in the control (C) group (E:83%, C:53%, χ2=55.049, p< 0.01). When asked what they thought the term meant, responses related to the following main themes: ‘feelings of depression’ (E:1%, C:4%), ‘the wearing off of drugs’ (E:1%, C:5%), ‘feelings of happiness’ (E:4%. C:2%), ‘lack of serotonin’ (E:10%, C:24%), and ‘an excess of serotonin’ (E:46%, C:24%). Just over one-third (E:38%, C:41%) reported that they did not know. In keeping with a recognised definition for serotonin syndrome [37], responses which related to ‘an excess of serotonin’ were regarded as correct. The experimental group was significantly more likely than the control group to identify the term correctly (E:46%, C:24%, χ2=21.506, p< 0.01) and to report that they had heard it from peer educators at a dance party or music festival (E:85%, C:8%, χ2=122.718, p< 0.01).
Participants (n=661) scored the credibility of the information received on a five point scale from zero (not credible) to four (very credible). Generally, the information received was perceived as highly credible (mean score 3.6, SD 0.64). Participants thought the information would possibly (24%) or definitely (31%) change the way they use drugs. Typical responses related to reducing use, using in a safer way and greater consideration of the risks. About half (46%) reported that their patterns of drug use were not likely to change. Of the participants who recalled collecting pamphlets, a majority (55%) referred to the information later (i.e., when not intoxicated) and shared the information with others (68%). About one in five (17%) were prompted to seek out further information about drugs. Most (75%) would approach these peer educators again if they saw them at an event.
Changes in patterns of drug use
In relation to ecstasy and methamphetamine, participants were asked about ever (lifetime) use, recent (past month) use and mean days use in the previous month.At post-intervention (among participants followed-up), there were no significant differences between the experimental and control group in relation to patterns of drug use except in relation to recent ecstasy use (82% versus 69%; χ2=-7.819, p< 0.01) and mean days ecstasy use (2.2 days versus 1.6 days; z=-2.576, p< 0.05), which were significantly higher in the experimental group.At three month follow-up, the mean days of ecstasy and methamphetamine use in the previous month and the recent use of methamphetamine significantly decreased in the experimental group and remained stable among the control group (Table 3). The recent use of ecstasy significantly decreased in both the experimental and control group. Further analysis revealed that the proportion which had decreased recent ecstasy use was not significantly different between the experimental and control group.
Most participants interviewed immediately post-intervention (E:60%, C:56%) and at follow-up (E:63%, C:62%) reported never or rarely using a combination of two or more drugs (possible response categories were never, rarely, sometimes, often and always). A minority reported often (E:11%, C:13%) or always (E:7%, C:6%) combining drugs. Overall, differences in polydrug use between the experimental and control group among participants interviewed post-intervention and follow-up were small and non-significant.
Discussion
This study evaluated the efficacy of peer-led information dissemination among a group of ecstasy users in Australia utilising a quasi-experimental study design. The peer education methodology used was effective in disseminating health and drug information. The unique ecstasy-related message was recalled immediately post-intervention and after three months. Additionally, aspects of drug involvement decreased at three month follow-up among the experimental and control group. While the information provided by peer educators may partly account for this, results must be considered in the light of other plausible explanations for the change in patterns of drug use.Information received from peer educators
Generally, the study provides convincing evidence that the peer education methodology used was effective in disseminating health and drug information. The unique message about ‘serotonin syndrome’ was clearly the most commonly recalled health message among the experimental group - immediately post-intervention and three months later. Furthermore, ecstasy users at experimental sites were more likely to have heard about the term serotonin syndrome, identify it correctly and have heard about it from a peer educator at a dance event than those at control sites. At experimental sites, the unique message was also much more commonly recalled than the usual information disseminated. Together, these findings demonstrate that health messages can be effectively disseminated by the peer education methodology used and that the messages can be recalled after three months.While it was encouraging that almost two-thirds of participants immediately post-intervention recalled the health message related to serotonin syndrome, this had subsequently decreased to just under half at three month follow-up. The simplicity of the message and peer educators’ confidence in message delivery are factors which may have influenced recall and correct identification of the term serotonin syndrome. This emphasises the need to use health messages which are simple to convey and comprehend, and reinforces the importance of providing high-quality peer educator training about the messages and delivery.
Interestingly, information about the importance of drinking enough water was widely recalled at follow-up but was not so commonly recalled immediately post-intervention. One explanation is that information received from other sources such as mainstream media, street press and the internet may have been confused with information received from peer educators. This is particularly likely as harm reduction messages targeting ecstasy users about water intake have been extensive, especially so since several widely publicised ecstasy-related deaths [39,40].
The information provided by peer educators was perceived as highly credible. The perceived credibility of the peer educator is important as it influences the persuasiveness of the message [41]. Therefore a more credible message is more likely to shift behavioural peer norms. About one-third of ecstasy users thought that the information provided would change the way they use drugs. Whether participants actually moderated their drug use as a result of the information provided by peer educators was difficult to determine, as discussed below. Nevertheless, this finding suggests that drug-related peer education can encourage reflection on patterns of drug use and contemplation of behaviour change. This left a substantial proportion that was not contemplating a change in drug using behavior. However, it can be peculated that there would have been light, intermittent users amongst them who were likely to perceive their drug use as non-problematic and, therefore, were not contemplating a behavior change at the time of the study.
It was encouraging that a majority of participants collected drug- and health-related information pamphlets from peer educators and referred to them at a later date. Pocket-sized resources of this kind are likely to be an effective way to reinforce the information provided by peer educators at events, particularly if the material is relevant and appealing to young people. Substantial proportions shared the information received with others, which demonstrates the potential flow-on effect of peer education. It was promising that the information received prompted people to proactively seek out further information (e.g., using the internet). KIS frequently report that ‘hits’ to their website, which provides alcohol and other drug information, increase after attending events (K. Devlin, personal communication). A large majority of ecstasy users would definitely approach the peer educators again if they saw them at an event which was an exceptionally encouraging finding.
Study findings suggest the peer led methodology used was effective in disseminating ecstasy-related health messages to citydwelling, twenty-something ecstasy users. However, caution must be used in generalizing findings to interventions which use other peerled methodologies and which target users of drugs other than ecstasy.
Patterns of drug use
A positive outcome was that among the experimental group there was a significant decrease in the mean days use of ecstasy and methamphetamine and the recent use of methamphetamine, compared to the control group. Specific information about thepotential harms of ecstasy and methamphetamine use was part of the unique message promoted at experimental sites which may have contributed to this reduction.
A further positive outcome was the significant reduction in recent ecstasy use among the experimental and control group. Some information, such as the potential harms of ecstasy use, was part of usual drug-related information and part of the information provided on the unique message about serotonin syndrome which may account for lower levels of drug use in both groups. The result may, however, reflect regression toward the mean as recent ecstasy use post-intervention was relatively high, particularly in the experimental group.
It is also possible there may have been a seasonality effect ondrug use. This is likely to be more pronounced for the experimental group than the control group. Participants in the experimental group were recruited at music events held later in the ‘party’ season, and therefore, their level of drug involvement may have been lower than participants in the control group (who were recruited earlier in the ‘party’ season). While the reductions in drug involvement were promising, it is difficult to determine whether they were associated with the usual drug-related information received, the unique message about serotonin syndrome or other factors altogether.
The lifetime prevalence of patterns of drug use which are risk factors for serotonin syndrome was low but of concern. About one in thirteen participants had used antidepressant drugs with ecstasy – a potentially risky practice. Lifetime recreational use of methylphenidate or dexamphetamine was relatively common (30%), which is in keeping with other studies of ecstasy users in Australia [16].
Unfortunately, follow-up survey questions were not specific enough to identify changes in patterns of drug use which were risk factors for serotonin syndrome (e.g., combining antidepressant drugs with ecstasy). Furthermore, the prevalence of such patterns of use was generally very low among participants interviewed post-intervention, suggesting statistically significant differences would have been difficult to detect.
Limitations
Conclusion
Findings highlight a number of important considerations for peerled education interventions. Fundamental to success is that the peerled peerled intervention is based on an established, evidence-based model (e.g., Unity, Amsterdam [44]). The health messages developed need to be unique, relevant and simple, and be supported with information flyers and merchandising which is popular with young people. To ensure proficiency, peer educators must receive high-quality training specifically related to the messages used. Additionally, providing only one or two drug-related health messages during a music event is likely to be much more effective than providing messages on a wide range of topics. Equally important is to conduct the intervention during the early part of the event, before participants become intoxicated. Lastly, securing access to appropriate dance events can be challenging, so peer education organisations which establish and maintain good relationships with the nightlife industry are more likely to succeed.
Acknowledgements
References
- Bament D (2001) Peer Education Literature Review. South Australian Community Health Research Unit, Adelaide.
- Cuijpers P (2002) Peer-led and adult-led school drug prevention: A meta-analytic comparison. J Drug Educ 32: 107-119.
- Backett-Milburn K, Wilson S (2000) Understanding Peer Education: insights from a process evaluation. Health Educ Res 15: 85-96.
- Romer D, Hennessy M (2007) A biosocial-affect model of adolescent sensation seeking: the role of affect evaluation and peer-group influence in adolescent drug use. Prev Sci 8: 89-101.
- Odgers P (1998) Adolescent Substance Use, in Drug use in Australia: a harm minimisation approach, M. Hamilton, A. Kellehear, and G. Rumbold, Editors. Oxford University Press: Melbourne.
- Spooner C (1999) Cause and correlates of adolescent drug abuse and implications for treatment. Drug Alcohol Rev 18: 453-475.
- Vervaeke H, van Deursen L, Korf D (2008) The role of peers in the initiation and continuation of ecstasy use. Subst Use Misuse 43: 633-646.
- Beck J, Rosenbaum M (1994) The pursuit of ecstasy: the MDMA experience. State University of New York Press, Albany, NY.
- Gowing L, Henry-Edwards S, Irvine R, Ali R (2002) The health effects of ecstasy: a literature review. Drug Alcohol Rev 21: 53-63.
- Turner G, Shepherd J (1999) A method in search of theory: peer education and health promotion. Health Educ Res 14: 235-247.
- UNAIDS (1999) Peer education & HIV/AIDS: concepts, uses and challenges. UNAIDS, Geneva.
- Ward J, Hunter G, Power R (1997) Peer education as a means of drug prevention and education among young people. Health Educ J 56: 251-263.
- Bleeker A, Silins E (2008) Faith, love and theory: peer-led interventions for 'party drug' users, in Drugs and Public Health: Australian perspective on policy and practice, D. Moore and P. Dietze, Editors. Oxford University Press: Melbourne.
- Audrey S, Holliday J, Campbell R (2006) It's good to talk: Adolescent perspectives of an informal, peer-led intervention to reduce smoking. Soc Sci Med 63: 320-334.
- Borgia P, Marinacci C, Schifano P, Perucci C (2005) Is peer education the best approach for HIV prevention in schools? Findings from a randomized controlled trial. J Adolesc Health 36: 508-516.
- Black E, Dunn M, Degenhardt L, Campbell G, George J, et al. (2008) Australian trends in ecstasy and related drug markets 2007: Findings from the Ecstasy and Related Drugs Reporting System (EDRS). Australian Drug Trends Series No. 10. National Drug and Alcohol Research Centre; University of New South Wales: Sydney.
- Fors S, Jarvis S (1995) Evaluation of a peer-led drug abuse risk reduction project for runaway/homeless youths. J Drug Educ 25: 321-333.
- Grund J, Broadhead D, Heckathorn L, Synn Stern (1996) Peer-driven outreach to combat HIV among IUDs: a basic design and preliminary results, in AIDS, drugs and prevention: perspectives on individual and community action, T. Rhodes and R. Hartnoll, Editors. Routledge: London.
- Herkt D (1993) Peer-based user groups: the Australian experience, in Psychoactive drugs and harm reduction: from faith to science, N. Heather and A. Wodak, Editors. Whurr Publishers: London.
- Skelton E, Shervil J, Mullan R (1997) Young People’s Drug Use at Dance Events. Crew 2000: Glasgow.
- Tobler N (1986) Meta analysis of 143 drug prevention programs: quantitative outcome results of program participants compared to a control or comparison group. Journal of Drug Issues 16: 537-567.
- Bleeker A ( 2000) The Drug Stop Project: development, implementation and evaluation of a drug and alcohol peer education project for young people, Manly Drug Education and Counselling Centre: Sydney.
- van Bakkum F (2005) Project Evaluation Report Unity 2005., Jellinek Drug Prevention: Amsterdam.
- Grund J, Blanken P, Adraans N, Kaplan C, Barendregt C, et al. (1992) Reaching the unreachable: targeting hidden IDU populations with clean needles via know user groups. J Psychoactive Drugs 24: 41-47.
- Grund J, Kaplan C, de Vries M (1993) Rituals of Regulation: Controlled and Uncontrolled Drug Use in Natural Settings, in Psychoactive drugs and harm reduction: from faith to science, N. Heather, et al., Editors. Whurr Publishers: London. 77-90.
- Rhodes T, Hartnoll R (1996) AIDS, Drugs and Prevention: Perspectives on Individual and Community Action. Routledge, London.
- Wye S (2006) A framework for peer education by drug user organizations. Australian Injecting and Illicit Drug Users League, Canberra.
- Elford J, Bolding G, Sherr L (2004) Popular opinion leaders in London: a response to Kelly. AIDS Care 16: 151-158.
- Webel A, Okonsky J, Trompeta J, Holzemer WL (2010) A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am J Public Health 100: 247-253.
- Frankham J (1998) Peer Education the unauthorised version. British Educational Research Journal 24: 179-193.
- Lindsey B (1997) Peer education: A viewpoint and critique. J Am Coll Health 45: 187-89.
- Shiner M (1999) Defining peer education. J Adolesc 22: 555-566.
- Walker S, Avis M (1999) Common reasons why peer education fails. J Adolesc 22: 573-577.
- Black E, Roxburgh A, Degenhardt L, Bruno R, Campbell G, et al., Australian drug trends 2007; Findings from the Illicit Drug Reporting System (IDRS). Australian Drug Trends Series No. 1. 2008, National Drug and Alcohol Research Centre; University of New South Wales: Sydney.
- Australian Institute of Health and Welfare (2008) 2007 National Drug Strategy Household Survey: detailed findings. Drug Statistic Series 22. AIHW, Canberra.
- Degenhardt L, Hall W, eds. The health and psychological effects of 'ecstasy' (MDMA) use: Monograph. 2009, National Drug and Alcohol Research Centre; University of New South Wales: Sydney.
- Gillman P (1999) The serotonin syndrome and its treatment. J Psychopharmacol (Oxf) 13: 100-109.
- Silins E, Copeland J, Dillon P (2007) Qualitative review of serotonin syndrome, ecstasy (MDMA) and the use of other serotonergic substances: hierarchy of risk. Aust N Z J Psychiatry 41: 649-655.
- Donaghy B (1996) Anna's story. Angus & Robertson, Sydney.
- Betts J, Betts P, Sage I (1999) Leah Betts: The legacy of ecstasy. Robson Books Ltd, London.
- Petty R, Cacioppo J (1981) Attitudes and persuasion: Classic and contemporary approaches. William. C. Brown, Dubuque.
- Berg CJ, Lust KA, Sanem JR, Kirch MA, Rudie M, et al. (2009) Smoker self-identification versus recent smoking among college students. Am J Prev Med 36: 333-336.
- Darke S (1998) Self-report among injecting drug users: a review. Drug Alcohol Depend 51: 253-263.
- Bleeker A, Jamin J (2003) Peer education at dance events: 'Unity' do-it-yourself guide. Jellinek Prevention, Amsterdam.