Journal of Andrology & Gynaecology
Download PDF
Case Report
*Address for Correspondence: Susmita Pankaja, Department of Obstetrics & Gynaecology, St Helens & Knowsley NHS Trust, Whiston Hospital, Prescot L35 5DR, UK, Tel: +44 151 430 2354; Fax: +44 151 430 1335; E-mail: susmitapankaja@yahoo.com
Citation:Pankaja S, Ip P, O’Mahony F. Successful Pregnancy with Uterus Didelphys. J Androl Gynaecol. 2016;4(2): 3.
Copyright © 2016 Pankaja S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN : 2332-3442 | Volume: 4, Issue: 2
Submission: 18 July, 2016| Accepted: 19 September, 2016 | Published: 28 September, 2016
Successful Pregnancy with Uterus Didelphys
Susmita Pankaja1*,Patricia Ip2and Fidelma O’Mahony3
- 1Department of Obstetrics & Gynaecology, St Helens & Knowsley NHS Trust, Whiston Hospital, Prescot, UK
- 2Prince of Wales Hospital, 30-32 Ngan Shing Road, Shatin, New Territories, Hong Kong
- 3Department of Obstetrics & Gynaecology, University Hospital of North Midlands, Newcastle Road, Stoke-on-Trent, UK
*Address for Correspondence: Susmita Pankaja, Department of Obstetrics & Gynaecology, St Helens & Knowsley NHS Trust, Whiston Hospital, Prescot L35 5DR, UK, Tel: +44 151 430 2354; Fax: +44 151 430 1335; E-mail: susmitapankaja@yahoo.com
Citation:Pankaja S, Ip P, O’Mahony F. Successful Pregnancy with Uterus Didelphys. J Androl Gynaecol. 2016;4(2): 3.
Copyright © 2016 Pankaja S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN : 2332-3442 | Volume: 4, Issue: 2
Submission: 18 July, 2016| Accepted: 19 September, 2016 | Published: 28 September, 2016
Abstract
Uterine anomalies can be associated with various complications in pregnancy and labour. We report 3 cases of uterus didelphys with varying clinical courses in pregnancy and labour. Case 1 had an uneventful pregnancy, labour and delivery. Case 2 went into preterm labour at 33 weeks and had a Caesarean section due to failure to progress in the first stage of labour and fetal distress. Case 3 had an elective Caesarean section due to her history of uterine surgery.Keywords
Uterus didelphys; Mullerian anomalies; Obstructed hemivagina; ipsilateral renal anomaly; Double cervixIntroduction
The female reproductive organs are largely derived from the two paramesonephric or mullerian ducts in fetal life which give rise to the upper third of the vagina, cervix, uterus and the fallopian tubes. The Mullerian ducts of the two sides fuse from the caudal end to form the uterovaginal canal. The cranial ends remain unfused and form the fallopian tubes. If there is a failure of fusion of the mullerian ducts, various anomalies ensue, ranging from septate and bicornuate uteri to uterus didelphys. Uterus didelphys occurs due to mullerian unification defects resulting in various abnormalities with the presence of 2 uteri, 2 cervices and often 2 vaginas [1]. Occasionally a longitudinal or transverse vaginal septum is present [2]. Mullerian abnormalities are frequently associated with renal tract anomalies due to their common origin [1]. Ovarian development, however is not affected as ovaries are not derived from the mullerian ducts but have their origin from the primordial germ cells [1,2].Congenital anomalies of the uterus are considered important due to the associated complications with pregnancy. We report 3 cases of uterus didelphys with successful pregnancy outcome. All cases were managed with input from a paediatric and adolescent gynaecologist as well as a fetal medicine specialist.
Case Series
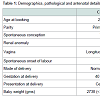
Case 1: A 23 year old primigravida presented to the antenatal clinic (ANC) following a spontaneous conception (Table 1).She was investigated at 18 years of age for chronic pelvic pain and was found to have a uterus didelphys bicollis with a longitudinal vaginal septum. No renal abnormalities were identified.The pregnancy was in the right uterus and was monitored with serial growth scans. She went into spontaneous labour a day after her expected date of delivery and went on to have a normal vaginal delivery. The baby weighed 2738 grams.
Case 2: A 28 year old primigravida presented to ANC following spontaneous conception (Table 1).
She had been investigated 2 years prior to conception for heavy postcoital bleeding (Estimated blood loss = 250 ml). On that occasion an examination under anaesthesia was carried out and a torn longitudinal vaginal septum was found as the source of the bleeding. Two cervices were identified and the septal edges were sutured. An ultrasound scan confirmed the presence of uterus didelphys with normal renal tract.
Her dating ultrasound scan showed the pregnancy to be in the left uterus and serial growth scans were planned during pregnancy. She presented in preterm labour at 33 weeks gestation and had a Caesarean section for failure to progress and a pathological cardiotocogram (CTG). The baby weighed 2130 grams.
Case 3: A 26 year old primigravida was referred to the ANC following spontaneous conception in view of the presence of uterus didelphys (Table 1).
At 23 years of age she had presented, with abdominal pain and a left sided palpable mass reaching to the level of the umbilicus. The pain commenced with menarche and had progressively worsened. A 95 x 40 x 45 mm mass was confirmed on ultrasound scan. Differential diagnoses included a tubo-ovarian mass related to a torted left ovary or pyosalpinx. In view of the size of the mass and the severity of the pain an exploratory laparotomy was carried out by the on call team.
The findings were of a uterus didelphys with a left sided hematometra which was adherent to the sigmoid colon posteriorly (Figure 1). The left fallopian tube was also distended. Both ovaries were normal. The vagina on the left side was blind ended. The hematometra was drained vaginally and abdominally and further imaging was arranged postoperatively.Magnetic resonance (MR) imaging demonstrated a normal right kidney, with an absent left kidney. The right sided uterus, cervix and ovary appeared normal and the cervix on that side appeared to be communicating with the vagina. The findings on the left side were suggestive of dilated left uterus and fallopian tube with a normal left ovary.
She went on to have a second laparotomy with removal of the left uterus, cervix and the fallopian tube. She had an uncomplicated postoperative period. At follow up she reported a normal menstrual pattern and an ultrasound scan showed a normal uterus.
During her pregnancy, she had a dating scan at 12 weeks, an anomaly scan at 20 weeks and serial growth scans thereafter. The growth scans confirmed fetal growth along the 10th centile. The amniotic fluid index (AFI) was below the 5th centile on several occasions but the umbilical artery Dopplers were normal.
In view of her previous uterine surgery, an elective Caesarean section was carried out at 38 weeks.
The baby weighed 2988 grams, which was just above the 10th centile.
Discussion
Patients with Mullerian anomalies can be asymptomatic or can present with primary infertility or hematometra. Fertility is not reduced in unification defects but they can be associated with miscarriage and preterm delivery. A systematic review by Chan et al. grouped the anomalies as arcuate uteri, canalisation defects (septate and subseptate uteri) and unification defects (unicornuate uterus, bicornuate uterus and uterus didelphys). Renal anomalies can be also associated with Mullerian anomalies due to the common mesonephric origin [3].Although the presence of double cervix on vaginal examination almost certainly indicates the presence of uterus didelphys, there are case reports of 2 cervices with a single normal uterus. The underlying pathological mechanism is unclear as it cannot be explained by the usual embryological pathogenesis [4].
Smith et al. performed MR imaging on 64 women found to have double cervices over a period of 24 years. Thirty two (50%) had septate uterus, 27 (42%) uterus didelphys and 5 (8%) bicornuate uterus. Cervical canal divergence was present in 11/32 (34%) with septate uterus, 7/27 (26%) with uterus didelphys, and none with bicornuate uterus. They concluded that septate uterus is as common as uterus didelphys, and considerably more common than bicornuate uterus, in women with double cervices [5].
Hua et al. describe a patient who presented with hematometra leading to pyometra and removal of one uterus (uterus didelphys), similar to case 3. This presentation is termed Herlyn-Werner-Wunderlich syndrome (HWW) which is a rare entity with obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) [6]. Clinical diagnosis relies on a high index of suspicion as the patient menstruates normally from the patent side while vaginal examination reveals a single cervix.
MR and ultrasound imaging is useful in determining the exact morphology and planning of surgery in such patients [7,8]. Our patient presented at the age of 23 which was unusual given that it tends to present shortly after menarche with pelvic pain and/or a mass and rarely, in later years, with primary infertility [4,7,8]. Management is by resection of the blind-ended uterine horn.
Pregnancy in women with congenital uterine anomalies can be associated with complications both in pregnancy and labour [3,6]. The incidence of uterine anomalies has been quoted between 1 - 10% in the literature [3]. Zhang et al. in their retrospective study over an 11 year period found the incidence of uterine anomalies to be approximately 0.45% of all deliveries and uterus didelphys was seen in 24.2% of all uterine anomalies [9]. Simon et al. found the incidence of uterine anomalies to be 3.5% of the population studied (22/679). Of these, 90% had a septate uterus, 5% had a bicornuate uterus and another 5% had a uterus didelphys [10].
Patients with uterine anomalies have a high Caesarean section (CS) rate (53%) which is highest (82%) in the uterus didelphys group [6]. They are also associated with an increased risk of preterm birth, preterm prelabour rupture of membranes, breech presentation, labour dystocia, placenta praevia and placental abruption [6]. Fetal malpresentation is increased in all types of anomalies and there is an increased incidence of small for gestational age fetuses [3].
All three of our patients had uterus didelphys and had spontaneous conception with no history of infertility or miscarriage. One of the three patients went in to preterm labour at 34 weeks. One baby weighed below the 10th centile while the other two weighed between the 10th and 25th centiles.
Conclusion
Women who have uterus didelphys due to Mullerian unification defect with the presence of 2 uteri, 2 cervices and often 2 vagina can have varying presentations. Studies have shown that this is not associated with difficulty in conception but there is increased incidence of preterm labour, malpresentation and malposition. Labour dystocia can occur due to malposition and Caesarean section can be difficult due to thick dividing septum. However, as shown in our series, with appropriate antenatal and intrapartum surveillance pregnancy outcomes are good. The diagnosis can be challenging in the presence of one blind vagina and is reliant on a high index of suspicion in order to achieve prompt and appropriate treatment.References
- Mitchell B, Sharma R (2012) Embryology: an illustrated colour text (2nd edn.), Churchill Livingstone.
- Chandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD (2009) Müllerian duct anomalies: from diagnosis to intervention. Br J Radiol 82: 1034-1042.
- Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, et al. (2011) Reproductive outcomes in women with congenital uterine anomalies: a systematic review: Ultrasound Obstet Gynecol 38: 371-382.
- Del Vescovo R, Battisti S, Di Paola V, Piccolo CL, Cazzato RL, et al. (2012) Herlyn-werner-wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging 12: 4.
- Smith BC, Brown DL, Carter RE, Famuyide AO (2014) Double cervix: clarifying a diagnostic dilemma. Am J Obstet Gynecol 211: 26.e1-e5.
- Hua M, Odibo AO, Longman RE, Macones GA, Roehl KA, et al. (2011) Congenital uterine anomalies and adverse pregnancy outcomes. Am J Obstet Gynecol 205: 558.e1-e5.
- Heinonen PK, Saarikoski S, Pystynen P (1982) Reproductive performance of women with uterine anomalies. An evaluation of 182 cases. Acta Obstet Gynecol Scand 61: 157-162.
- Cox D, Ching BH (2012) Herlyn-Werner-Wunderlich syndrome: a rare presentation with pyocolpos. J Radiol Case Rep 6 : 9-15.
- Zhang Y, Zhao YY, Qiao J (2010) Obstetric outcome of women with uterine anomalies in China. Chin Med J (Engl) 123: 418-422.
- Simon C, Martinez L, Pardo F, Tortajada M, Pellicer A (1991) Müllerian defects in women with normal reproductive outcome: Fertil Steril 56 : 1192-1193.