Journal of Andrology & Gynaecology
Download PDF
Research Article
*Address for Correspondence: Osama Kamal Zaki Mahmoud Shaeer, Department of Andrology, Kasr El Aini Faculty of Medicine, Cairo University, 21 Gaber Ibn Hayan St., Dokki, Cairo, Egypt, 12311 AR, Cairo, Egypt, Tel: (202)33359047, (202)33374360; Fax: (202)37605181; E-mail: dr.osama@alrijal.com
Citation: Shaeer K, Shaeer O. Shaeer’s Corporal Rotation-II: No-Corporotomy Technique. J Androl Gynaecol. 2014;2(3): 3.
Copyright © 2014 Shaeer K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN 2332-3442 | Volume: 2, Issue: 3
Submission: 01 September 2014 | Accepted: 18 September 2014 | Published: 20 September 2014
Shaeer’s Corporal Rotation-II: No-Corporotomy Technique
Kamal Shaeer and Osana Shaeer*
- Department of Andrology, Kasr El Aini Faculty of Medicine, Cairo University, Egypt
*Address for Correspondence: Osama Kamal Zaki Mahmoud Shaeer, Department of Andrology, Kasr El Aini Faculty of Medicine, Cairo University, 21 Gaber Ibn Hayan St., Dokki, Cairo, Egypt, 12311 AR, Cairo, Egypt, Tel: (202)33359047, (202)33374360; Fax: (202)37605181; E-mail: dr.osama@alrijal.com
Citation: Shaeer K, Shaeer O. Shaeer’s Corporal Rotation-II: No-Corporotomy Technique. J Androl Gynaecol. 2014;2(3): 3.
Copyright © 2014 Shaeer K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN 2332-3442 | Volume: 2, Issue: 3
Submission: 01 September 2014 | Accepted: 18 September 2014 | Published: 20 September 2014
Abstract
Background: Surgical techniques for correcting congenital penile curvature -without hypospadias- can be classified into three main categories: tunical shortening procedures with possible loss in length, tunical lengthening procedures with possible erectile dysfunction (ED), and penile prosthetics. Corporal rotation can correct the most severe degrees of congenital curvature without the fore mentioned drawbacks. This work describes modification and troubleshooting of corporal rotation aiming at simpler and less invasive technique, preserving length, girth symmetry and erectile function.Methods: The penis was degloved through a subcoronal incision. The neurovascular bundle was mobilized. Interrupted multifilament Polyester 3/0 sutures were placed bridging the dorso-lateral aspects of the corpora cavernosa, proximal and distal to the point of maximum curvature. The sutures were tied in the semi-erect state while bending the penis dorsally (counter to the direction of curvature) and with the assistant dipping the midline inwards by a haemostat to allow approximation of both corpora on top of the midline, achieving corporal rotation. Manoeuvres to address residual curvature, narrowing or girth asymmetry were employed.
Results: Average pre-correction angle was 59.7° ± 12.8. Average post-correction angle was 0.9° ± 2.7. There was no statistically significant difference in penile length pre and post correction (p=0.07). There was a mild though statistically significant decline in girth following correction (3.4%, p=0.003). None of the cases showed girth asymmetry.
Conclusion: The current modification of corporal rotation allows minimally invasive correction of severe degrees of isolated ventral or dorsal congenital penile curvature, preserving length and girth, and with relatively short abstinence from coital activity. Troubleshooting manoeuvres described help avoid residual curvature, girth asymmetry and narrowing.
Keywords
Curvature; Penis; Congenital curvature; Corporal rotation; Corporeal rotationIntroduction
Penile curvature is addressed surgically if the degree and direction interfere with coital activity or are cosmetically unacceptable from the patient’s point of view. Focusing on congenital curvature without hypospadias (isolated congenital curvature), surgical techniques can be classified into three main categories: tunical shortening procedures, tunical lengthening procedures, and penile prosthetics. With shortening techniques, the tunica albuginea on the longer/ convex aspect of the penis is reduced, thereby correcting curvature on the expense of length. This includes Nesbit procedure, modified Nesbit technique, tunica albuginea plication (TAP), the 16 dot techniques, among others [1-5]. The extent of shortening is generally proportional to the degree of curvature, possibly leading to severe loss in length with the higher grades of curvature [6]. On the other hand, lengthening procedures are based on incision and grafting of the tunica albuginea on the shorter/concave side of the penis [7], correcting curvature on the expense of erectile function which is prone to deterioration [8]. Prosthetic surgery is reserved to patients with severe degrees of curvature or associated with refractory erectile dysfunction (ED).In 2006, “Shaeer’s Corporal Rotation” was first introduced to correct cases of severe isolated congenital curvature with neither shortening nor ED [9]. The technique is based on shifting the concavities of both corpora cavernosa from the ventral aspect of the penis to the lateral aspects in opposition, such that they flex against each other rather than synergistically, thereby neutralizing their curvature-inducing effect. Following mobilizing the neurovascular bundle, two incisions are cut, one on the dorso-lateral aspects of each corporus cavernosum at the point of maximum curvature. Suturing the two incisions to each other achieves rotation and corrects curvature. Further incisions are cut and sutured in case there is residual curvature [9]. The calibre of the urethra was not compromised. A drawback was the mild change in girth, wider distally and narrower proximally. In 2008, corporal rotation was modified [10,11] based on further experience, addressing the fore mentioned drawback. Instead of limited incisions at and around the point of maximum curvature, two longitudinal incisions along the length of the shaft were incised and sutured, thereby achieving rotation and correction of curvature without girth asymmetry. In 2011, corporal rotation was applied to correct cases of isolated congenital dorsal curvature, mobilizing the corpus spongiosum and rotating the corpora underneath the urethra [12].
This work describes further modification of corporal rotation, aiming at making the technique simpler and less invasive. Troubleshooting is described to address residual curvature, girth asymmetry and narrowing.
In this case presentation, we represent an endometrial TB case diagnosed during the investigation of abnormal uterine bleeding resistance to progestin therapy.
Methods
Sixteen patients with congenital penile curvature were operated upon. In all patients, curvature was ventral in direction, ranging from 45 to 85 degrees. Erectile function was normal as evaluated by the International Index of Erectile Function (IIEF) and intracorporal injection of Prostaglandin E1 (PGE1). Degree of curvature was evaluated using protractor. Surgery was performed under general anaesthesia. Partial artificial erection was induced by injection of low dose PGE1 (10ug), complemented when needed to full erection with intracorporal saline injection. Erect penile length was measured intraoperatively using rigid ruler on two segments, one from pubis to the point of maximum curvature and the other from the latter point to the tip of the penis (Figure 1). Erect girth was measured using flexible tape (Figure 2). The penis was degloved through a subcoronal incision. The neurovascular bundle was mobilized under optical magnification. Four to five interrupted Polyester 3/0 sutures were placed bridging the dorso-lateral aspects of the corpora cavernosa. Blunt tip needles were used. Each suture entered through and exited from the dorsum of one corpus cavernosum, then again into and out of the other on the same horizontal level. The sutures were tied in the semi-erect state, while bending the penis dorsally (counter to the direction of curvature) and with the assistant dipping the midline inwards by a haemostat to allow approximation of both needle entry/exit points on top of the midline, achieving corporal rotation rather than compressing corporal tissue within the tied suture. Sutures were placed proximal and distal to the point of maximum curvature, evenly spaced along the length of the shaft of the penis to avoid indentation and abrupt changes in penile girth (Figure 3). Full erection was re-induced by saline injection, and erect length, girth, and straightness were evaluated (Figure 3,4). Residual curvature was corrected by removing the sutures and reapplying them further from the midline thereby inducing more rotation or by dorsal plication if further rotation would result in appreciable narrowing. Conversely, noticeable narrowing was addressed by cutting the sutures, reapplying them closer to the midline, and correcting any residual curvature by dorsal plication. Localized bulging was addressed by applying another suture at the bulging point.The incision was closed in two layers. Patients were discharged the same day and instructed to abstain from intercourse for one month. Patients were followed up through one year as regards erectile function by IIEF and self-reported straightness of erection.
Results
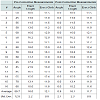
Average pre-correction angle was 59.7° ± 12.8. Average postcorrection angle was 0.9° ± 2.7. There was no statistically significant difference in penile length pre and post correction (p=0.07). There was a mild though statistically significant decline in girth following correction (3.4%, p=0.003). None of the cases showed girth asymmetry (Table 1). Average operative time was approximately 50 minutes.At the end of follow up, all cases reported a straight penis, normal erectile function and normal glans sensitivity despite initial sensory impairment that resolved spontaneously within the first six months, and painful erection that persisted for no more than 4 months. None of the patients reported shortening, two reported a decrease in girth and one reported girth asymmetry.
Discussion
Congenital penile curvatures -without hypospadias- are mostly managed by tunical shortening techniques, considering the possible ED following lengthening technique. The resultant shortening can sometimes be unacceptable particularly in the most severe degrees of curvature. Lengthening techniques via incision and grafting are employed more frequently in cases with Peyronie’s disease. In cases with congenital curvature however, the possible resultant ED may discourage some patients and surgeons. Discouragement is even more pronounced with prosthetic surgery that involves complications that may possibly result in permanent loss of erection in case infection or extrusion occur, and may also involve shortening. Corporal rotation corrects severe degrees of ventral or dorsal curvature with neither loss in length nor ED.Corporal rotation has evolved over time, from rotation by approximating shorter incisions at or around the point of maximum curvature with some girth asymmetry [9], to longer incisions that avoid the fore mentioned change in girth [11]. The technique has also been reproduced by other experts, with modifications as regards the method of anaesthesia, method of neurovascular bundle mobilization and suture material used, confirming the efficacy in straightening with length preservation in degrees of curvature ranging from 60-90° [13].
The current modification to corporal rotation provides several benefits. Above all, the required abstinence is significantly shorter, considering that there are no tunica incisions that require time to heal. The technique is now simpler than before. Operative time is shorter compared to the 2008 modification (50 versus 60 minutes on average). Lack of the formerly used tunical incisions should minimize the theoretical probability of ED even more.
Considering that narrowing or girth asymmetry are possible outcomes, troubleshooting manoeuvres presented herein help enhance the results and standardize the technique. Those manoeuvres were not feasible with the original technique involving incision of the tunica albuginea which cannot be easily undone. Employing the noncorporotomy technique allows undoing and redoing the sutures until the optimal state is reached.
Non-absorbable multifilament Polyester sutures are in our opinion preferable to monofilament Polypropylene sutures material considering that the former is less liable to cut through tissues thereby avoiding recurrence, are less liable to protrude thereby avoiding stitch sinus and pain, while still being highly biocompatible with minimal tissue reaction. Blunt tip needles also decrease tissue trauma and bleeding, while not exhibiting appreciable resistance upon needle entry and exit.
Corporal rotation still has some limitations. The technique is only suitable for purely ventral or dorsal congenital curvatures. Lateral curvature requires alternative techniques, and it is not known yet whether cases with combined horizontal and vertical axes curvature could benefit from the combination of a tunica shortening technique along with corporal rotation, where the former corrects horizontal axis (lateral) curvature and the latter corrects the vertical axis, thereby minimizing shortening. Furthermore, corporal rotation is yet to be tried in the management of Peyronie’s disease that are to date managed by alternative techniques.
Conclusion
The current modification of corporal rotation allows minimally invasive correction of severe degrees of isolated ventral or dorsal congenital penile curvature, preserving length and girth, and with relatively short abstinence from coital activity. The troubleshooting manoeuvres described help avoid residual curvature, girth asymmetry and narrowing.References
- Nesbit RM (2002) Congenital curvature of the phallus: report of three cases with description of corrective operation. 1965. J Urol 167: 1187-1188.
- Nesbit RM (1965) Congenital Curvature of the Phallus: Report of Three Cases with Description of Corrective Operation. J Urol 93: 230-232.
- Nesbit RM (1964) Congenital Curvature of the Phallus: Report of Three Cases with Description of Corrective Operation. Trans Am Assoc Genitourin Surg 56: 20-22.
- Baskin LS, Duckett JW (1994) Dorsal tunica albuginea plication for hypospadias curvature. J Urol 151: 1668-1671.
- Gholami SS, Lue TF (2002) Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 167: 2066-2069.
- Greenfield JM, Lucas S, Levine LA (2006) Factors affecting the loss of length associated with tunica albuginea plication for correction of penile curvature. J Urol 175: 238-241.
- Devine CJ, Jr, Horton CE (1975) Use of dermal graft to correct chordee. J Urol 113: 56-58.
- Dalkin BL, Carter MF (1991) Venogenic impotence following dermal graft repair for Peyronie’s disease. J Urol 146: 849-851.
- Shaeer O (2006) Correction of penile curvature by rotation of the corpora cavernosa: a case report. J Sex Med 3: 932-937.
- Shaeer O (2010) Shaeer’s Corporal Rotation. J Sex Med 7: 16-19.
- Shaeer O (2008) Shaeer’s corporal rotation for length-preserving correction of penile curvature: modifications and 3-year experience. J Sex Med 5: 2716- 2724.
- Shaeer O, Shaeer K, Abdulrasool M (2011) Corporal rotation for correction of isolated congenital dorsal curvature of the penis without shortening. HAJ 1: 26-29.
- Navarro N (2012) Key from Kols: Treatment of congential penile curvature by corpora cavernosa rotation. Modifications of Shaeer’s technique. A new surgical approach with minimal penile shortening ESSM Newsletter 9-10.