Journal of Andrology & Gynaecology
Download PDF
Research Article
*Address for Correspondence: Steven V. Kardos, MD, Department of Urology, Yale University School of Medicine, New Haven, CT, USA, E-mail: stevenkardos@gmail.com
Citation: Kardos SV, Lopez JM, Foster HE Jr. Transvaginal Bladder Neck Closure Revisited: A Less Invasive Approach to the Management of a Destroyed Urethra. J Androl Gynaecol. 2013;1(2): 4.
Copyright © 2013 Kardos SV, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN 2332-3442 | Volume: 1, Issue: 2
Submission: 30 July 2013 | Accepted: 16 September 2013 | Published: 18 September 2013
Transvaginal Bladder Neck Closure Revisited: A Less Invasive Approach to the Management of a Destroyed Urethra
Steven V. Kardos*, Jean M. Lopez and Harris E. Foster Jr
- Department of Urology, Yale University School of Medicine, New Haven, CT, USA
*Address for Correspondence: Steven V. Kardos, MD, Department of Urology, Yale University School of Medicine, New Haven, CT, USA, E-mail: stevenkardos@gmail.com
Citation: Kardos SV, Lopez JM, Foster HE Jr. Transvaginal Bladder Neck Closure Revisited: A Less Invasive Approach to the Management of a Destroyed Urethra. J Androl Gynaecol. 2013;1(2): 4.
Copyright © 2013 Kardos SV, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN 2332-3442 | Volume: 1, Issue: 2
Submission: 30 July 2013 | Accepted: 16 September 2013 | Published: 18 September 2013
Abstract
Introduction: An inevitable consequence of chronically urethral catheterized female patients with a neurogenic bladder is an incompetent urethra leading to leakage around the catheter. This is often managed by increasing the catheter size and/or the volume in the retaining balloon. Eventually these common practices lead to further urethral dilation and an incompetent urethra. The social embarrassment and skin breakdown from the incontinence can place significant demands on the patient and/or caregiver. Eventually this process of chronic urethral dilation leads to a destroyed urethra. Surgical options for this unique patient population is often compounded by medical comorbidities, obesity, poor nutritional status, and limited functional capacity [1]. Bladder neck suspension and suburethral slings are insufficient at providing continence thereby making bladder neck closure and suprapubic catheter placement a feasible alternative. Transabdominal bladder neck closure has been reported to have a lower risk of failure; however, it also has increased morbidity [2]. Transvaginal bladder neck closure affords a less invasive approach to a complex problem with quicker recovery while achieving satisfactory clinical continence in this difficult group of patients [1,3].Study design, materials and methods: A retrospective analysis was performed in a cohort of female patients who had undergone transvaginal bladder neck and suprapubic catheter placement at a single institution by a single surgeon. All patients had an incompetent urethra secondary to the use of a chronic indwelling urethral catheter manifested by leakage around the catheter. Data reviewed included demographics, cause of neurogenic bladder, medical comorbidities, and length of hospital stay, complications, and clinical continence.
Results: Five patients underwent transvaginal bladder neck closure and suprapubic catheter placement. The etiology of neurogenic bladder included spinal cord injury secondary to MVC, multiple sclerosis, and pathologic fracture of the spine. Average age and length of foley catheter use was 41.2 years and 6.2 years, respectively. Hospital stay averaged 3.2 days with a range of 1-7 days. 80% of patients were clinically continent with a mean post operative follow-up of 8.2 months. One of these patients had an improvement in incontinence, but is now clinically dry after a following operation.
Conclusions: Transabdominal bladder neck closure has been described in the literature to have a lower risk of fistulas and failure; however, it carries increased morbidity and hospital stay in a patient population with multiple complex medical problems. Transvaginal bladder neck closure has been described in the literature to have a failure rate of 17 to 60% with patients developing fistulas and florid incontinence [1,2]. In our experience, transvaginal bladder neck closure and suprapubic tube placement affords a less invasive approach to the incompetent urethra with a mean hospital stay of 3.2 days while achieving clinical continence. Transvaginal bladder neck closure with suprapubic catheter placement is a less invasive approach when compared to its transabdominal counterpart for female patients with a neurogenic bladder and incompetent urethra secondary to prolonged urethral catheter drainage. While peri-operative morbidity may not be insignificant, continence rates are satisfactory.
Introduction
Unfortunately, many patients with a neurogenic bladder aremanaged with a chronic indwelling urethral catheter. Reasons are varied and can include simplicity, inability to perform or have someone else perform intermittent catheterization, and reluctance to undergo any form of management that precludes its need (i.e. placement of suprapubic tube, creation of a continent cutaneous conduit, or urinary diversion). Long term indwelling urethral catheterization however can lead to many complications including recurrent urinary tract infections, hematuria, stone formation, refractory bladder spasms, and urethral incompetence. The latter is particularly problematic in females due to the anatomy of the urethra, primarily its length. Failure to secure the foley catheter or placing it on too much traction can further exacerbate the urethral damage. Pericatheter incontinence is frequently managed conservatively with sanitary towels, pads, or, pharmacotherapy; however, many patients and caregivers choose to increase the catheter and/or retaining balloon size or over inflate the balloon to reduce the incontinence and prevent extrusion of the catheter. In many instances, this common practice of upsizing catheter size or balloon volume leads to an incompetent and destroyed urethra necessitating change to another form of management or lower urinary tract reconstructive surgery [1,2,4].Surgical management of the destroyed female urethra secondary to chronic indwelling urethral catheterization is often compoundedby medical comorbidities, poor nutritional status, and limited functional capacity. Options include supravesical diversion, attempted functional closure with a tight pubovaginal sling if there is enough preserved urethra, and transabdominal or transvaginal bladder neck closure with an incontinent ileovesicostomy, continent catheterizable stoma or suprapubic catheter (cystostomy) placement [2,3,5]. Pubovaginal slings have generally been unsuccessful in providing continence in this patient population secondary to the severity of urethral injury and its proximity to its closure mechanism. Supravesical diversion with an ileal conduit can be challenging in this patient population due to concomitant comorbidities and body habitus (i.e. obesity) and may result in delayed recovery. Bladder neck and urethral closure is considered a feasible alternative. Concomitant placement of a suprapubic tube is the simplest option for draining the bladder however creation of an incontinent ileovesicostomy or a continent cutaneous catheterizable conduit can be entertained in appropriate circumstances [1,4]. Bladder neck closure can be achieved via a transabdominal or transvaginal approach. Transabdominal bladder neck closure has been described in the literature to have a lower risk of fistulas and failure; however, it also carries increased morbidity in patients with multiple medical comorbidities [1,2,6]. A transvaginal bladder neck closure can however afford a less invasive approach with quicker recovery while achieving acceptable clinical continence.
Material and Methods
After obtaining Institutional Review Board approval, a retrospective analysis was performed in a cohort of female patients with neurogenic bladder and a destroyed urethra who underwent transvaginal bladder neck closure and suprapubic catheter placement at a single institution by a single surgeon. Five patients were identified who had been chronically urethrally catheterized and reported intolerable incontinence around the catheter. All patients had an incompetent urethra secondary to the use of a chronic indwelling urethral catheter. Standard evaluation included a complete history, physical examination, routine laboratory evaluation, and upper tract imaging. Data reviewed included demographics, mobility, renal function, cause of neurogenic bladder, medical comorbidities, and prior urologic surgery (Table 1) Postoperative information analyzed included length of hospital stay, complications, and clinical continence (Table 2).Table 1: Demographics of Patients
Age (years) | Etiology | Length of Foley (years) | |
Patient 1 | 38 | Multiple Sclerosis | 1 |
Patient 2 | 37 | MVA, C7 injury | 14 |
Patient 3 | 57 | MVA | 7 |
Patient 4 | 47 | Pathologic fracture T12/L1 | 4 |
Patient 5 | 27 | Spinal Cord Injury C5-T8 | 5 |
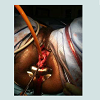
Table 2: Post-operative follow-up
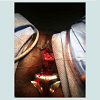
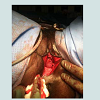
All patients underwent transvaginal bladder neck closure with suprapubic catheter placement. A thorough physical examination in the lithotomy position confirmed a capacious incompetent bladder neck and urethra as seen in Figure1. Cystoscopy was performed for complete bladder surveillance to rule out neoplasia, locate both ureteral orifices, and place a suprapubic catheter (20 French) with the assistance of a Lowsley retractor as previously described [7]. Following placement of a large caliber foley catheter per urethra, 1% lidocaine with epinephrine was used to hydrodissect the anteriorvaginal wall and to improve hemostasis. A 4 cm vertical incision was made in the anterior vaginal wall from a point 2-3 cm proximal to the bladder neck continuing up towards the urethral meatus. Curved scissors were used to bluntly dissect the anterior vaginal wall off of the underlying urethra. Dissection was carried laterally and through the endopelvic fascia into the retropubic space. The dissection was extended dorsally over the urethra to the inferior margin of the pubic symphysis connecting the incisions from both sides and the retropubic space by dividing the pubourethral ligaments. The lateral attachements were subsequently divided to mobilize the bladder and urethra. This completely freed the bladder neck and urethra circumferentially. The urethral closure was performed in two layers. First a horizontal interrupted or running 2-0 vicryl suture(s) was placed from each lateral end to reapproximate the mucosal and submucosal edges of the urethra, removing the foley catheter when the midline was reached as seen in Figure2. Placement of sutures continued until the bladder neck and urethra were completely closed.A second layer incorporating detrusor muscle was then closed in vertical fashion with interrupted 2-0 vicryl. The final closure in two layers can be seen in Figure3. Following this, the bladder was effectively transposed further up into the retropubic space. The vaginal wall was then closed with a running 2-0 chromic suture. Vaginal packing impregnated with bacitracin ointment was inserted overnight for added hemostasis. All patients were admitted overnight for observation and the vaginal packing was removed on postoperative day 1. Continuous bladder drainage was provided by the suprapubic tube. Initial follow up occurred at 3-4 weeks where saline was instilled via the suprapubic tube to assess integrity of the bladder neck/urethral closure. Hospital Stay (days) | Length of follow-up (months) | Continence | Complications | |
Patient 1 | 2 | 11 | Yes | None |
Patient 2 | 7 | 12 | Yes | Intubated, transfusion |
Patient 3 | 1 | 9 | Yes | None |
Patient 4 | 4 | 8 | Yes (after second procedure) | Transfusion, Redo operation |
Patient 5 | 2 | 1 | Yes | None |
Results
Five patients underwent transvaginal bladder neck closure and suprapubic catheter placement utilizing a previously described technique [7]. The etiology of neurogenic bladder included spinal cord injury, multiple sclerosis, and cerebrovascular accident. None of the patients had undergone prior surgery to the lower urinary tract. Indications for bladder neck closure included severe urethral erosion, skin breakdown exacerbated by urinary incontinence, and social embarrassment from global urinary incontinence. Figure1 depicts the characteristic appearance of the destroyed bladder neck and urethra with a large urethral catheter in place. Methods of bladder management just prior to the surgery included indwelling urethral catheter in four patients and sanitary pads in one. Average age and length of foley catheter use was 41.2 years and 6.2 years, respectively. Hospital stay averaged 3.2 days with a range of 1-7 days.Complications included immediate post-operative respiratory failure requiring intubation in a patient with poor respiratory status and peri-operative hemorrhage requiring transfusion in two patients. In all patients, the initial postoperative suprapubic catheter change occurred at 4 weeks which then continued monthly. Four patients (80%) were deemed clinically continent as defined by the use of no pads or the occasional use of pads with a mean post operative follow-up of 8.2 months. One patient continued to have persistent incontinence through the failed urethral closure and required further treatment. Subsequent repeat transvaginal urethral closure was successful and she is dry without the need for incontinence pads.
Discussion
Urethral injury secondary to a chronic indwelling urethral catheter resulting in pericatheter incontinence in the female neurogenic patient population poses many potential hurdles not only to the patient, but also to the caregiver. Nonoperative management can include incontinence pads and diapers as well as pharmacotherapy; however, outcomes are poor with the potential for skin breakdown leading to decubitus ulcers. Although increasing the size of the catheter and/or the retaining balloon may provide temporary relief, it generally only delays the ultimate outcome of worsening urethral function and incontinence. Surgical management can offer satisfactory continence rates however at the expense of surgical morbidity, poor wound healing, and long recovery in these chronically ill patients. Options include supravesical diversion, tight suburethral sling, and transabdominal versus transvaginal bladder neck closure with urinary diversion via suprapubic tube, incontinent ileovesicostomy, or continent catheterizable conduit. Bladder neck closure is a procedure not frequently performed, but can be beneficial in the appropriately selected patient [1,2].Feneley initially described transvaginal bladder neck closure in 24 patients using three circumferential purse string sutures placed intravesically to close the urethra. The initial fistula rate was 17% (4/24) [1]. Stoffel et al. noted 1 of 8 female patients’ continent after transvaginal bladder neck closure, but eventually yielded clinical continence after 2.3 procedures per patient [8]. Levy et al. noted an initial failure rate of 60% with the transvaginal approach; therefore, modified his technique to a combined transvaginal and transabdominal approach which decreased failure rate to 10% [6]. Andrews et al. reported a transvaginal bladder neck closure with a three layered closure; however, noted 50% failure rate at 3 months [9].
In a long term follow-up of this procedure in 47 patients with multiple sclerosis, 34 women were dry after the initial operation. Of the 13 patients who still experienced incontinence, 12 underwent a subsequent operation that eventually yielded seven patients with clinical continence. The long-term complications included eight with pericatheter leakage, ten with bladder stones, four with recurrent urinary tract infections, and five with recurrent catheter obstruction [4]. Zimmerman described a modified transvaginal bladder neck closure with 100% success rate in six patients; however, his technique was not reproducible as Nielson reported a 20% fistula rate with the same approach in 5 patients [10].
Transabdominal bladder neck closure has been described in the literature to have a lower risk of fistulas and failure; however, it carries increased morbidity, recovery, and hospital stay in a patient population at high risk of pulmonary, vascular, and wound-related complications. Conversely, transvaginal bladder neck closure has the advantage of a more rapid convalescence and shorter hospital stay by avoiding manipulation of the peritoneal cavity. In our experience, transvaginal bladder neck closure and suprapubic tube placement affords a less invasive approach to the incompetent urethra with a mean hospital stay of 3.2 days while achieving clinical continence in 80% after one procedure.
Conclusion
Transvaginal bladder neck closure with suprapubic catheter placement is a less invasive approach for female patients with a neurogenic bladder and incompetent urethra secondary to prolonged urethral catheter drainage. While peri-operative morbidity may not be insignificant, continence rates are satisfactory.References
- Ginger VT, Miller JL, Yang CC (2010) Bladder neck closure and suprapubic tube placement in a debilitated patient population. Neurourol Urodyn 29: 382- 386.
- Rovner ES, Goudelocke CM, Gilchrist A, Lebed B (2011) Transvaginalbladder neck closure with posterior urethral flap for devastated urethra. Urology 78: 208-212.
- Colli J, Lloyd LK (2011) Bladder neck closure and suprapubic catheter placement as definitive management of neurogenic bladder. J Spinal Cord Med 34: 273-277.
- Kubal U, Arunkalaivanan AL, Baptiste M (2009) Transvaginal closure of urethra and correction of uterovaginal prolapse in neurologically impaired patient with chronic indwelling catheter. Int Urogynecol J Pelvic Floor Dysfunct 20: 991-993.
- Shpall AI, Ginsberg DA (2004) Bladder neck closure with lower urinary tract reconstruction: technique and long-term followup. J Urol 172: 2296-2299.
- Levy JB, Jacobs JA, Wein AJ (1994) Combined abdominal and vaginal approach for bladder neck closure and permanent suprapubic tube: urinary diversion in the neurologically impaired woman. J Urol 152: 2081-2082.
- Edokpolo LU, Foster HE Jr (2011) Suprapubic cystotomy for neurogenic bladder using Lowsley retractor method: a procedure revisited. Urology 78: 1196-1198.
- Stoffel JT, McGuire EJ (2006) Outcome of urethral closure in patients with neurologic impairment and complete urethral desutruction. Neurourol Urodyn 25: 19-22.
- Andrews HO, Shah PJ (1988) surgical management of urethral damage in neurologically impaired female patients with chronic indwelling catheters. BrJ Urol 82: 820-824.
- Zimmerman P, Leach GE, Hadley HR, Schmidbauer CP, Staskin D, et al. (1986) Transvaginal closure of bladder neck. Seminars in Urology 4: 30-32.