Advances in Diabetes & Endocrinology
Download PDF
Congenital heart defects, most common abnormality,
comprising 35 to 40 percent of major congenital anomalies,
and includes tetralogy of Fallot, transposition of the great
arteries, septal defects, and anomalous pulmonary venous
return [27].
Central nervous system defects (anencephaly, spina bifida,
encephalocele, hydrocephaly, anotia/microtia)
Limb defects
Orofacial clefts
Defects in the urogenital system [28,29].
Sacral agenesis/caudal dysplasia (lack of fetal development of
the caudal spine and corresponding segments of the spinal
cord) accounts for 15 to 25 percent of all cases [30].
Review Article
Diabetes Mellitus and Planning Conception
TG Singh*
MBBS; MS (Obs/Gynae), FIAOG Associate member Royal College
of Obstetrics and Gynaecology, UK High Risk Pregnancy Specialist
Managing Director GNS Hospital, Chattarpur, New Delhi India
*Address for Correspondence: Dr. Tania G Singh, MBBS; MS (Obs/Gynae), FIAOG Associate member Royal College of Obstetrics and Gynaecology, UK High Risk Pregnancy Specialist,
Managing Director GNS Hospital, Chattarpur, New Delhi, India. E-mail id:
taniasingh.ts@gmail.com
Submission: 08 April, 2023 Accepted: 16 May, 2023 Published: 19 May, 2023
Copyright: © 2023 Singh TG. This is an open access article distributed
under the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided
the original work is properly cited.
Keywords: Diabetic Embryopathy; Metabolic Syndrome; Diabetic
Keto acidosis; Medical Nutrition Therapy; Pre Gestational Diabetes;
Diabetic Retinopathy; Diabetic Nephropathy; Ketogenic Diet
Abstract
Diabetes mellitus is a disease which affects endocrine system
and it is considered to beone of the most serious health problems to
modern global health. Glycemic control is one of themost important
aspects of preconception care; however other aspects such as folic
acid supplementation, smoking cessation, screening and treatment
of diabetes complications and discontinuing teratogenic medication,
are as important for improving maternal and fetal outcomes.
Effective preconception care is associated with improved
pregnancy outcomes for women with diabetes. A multidisciplinary
team work is essential for preconception care. Outcome becomes
fruitful with patient awareness and managing diabetes before
pregnancy in an organised manner.
Diabetes and Fertility- An Overview:
Diabetes is a disease that affects millions of people and their
families. The WHO estimates that more than 180 million people
worldwide have diabetes. This number is likely to become 300 million
by 2030 [1].Diabetes has become a major health burden affecting primarily
young adults and women in their reproductive age [2,3]. Type 1
diabetes is rising alarmingly worldwide, at a rate of 3% per year. Some
70,000 children aged 14 and under, develop Type 1 diabetes annually.
Type 2 diabetes is also increasing in number among children and
adolescents as obesity rates in this population continue to soar, in
both developed and developing nations [4].
Given its’ prevalence and heavy healthcare and quality-of-life
burden [6], there is a great need for better treatment options. Despite
improved access and quality of antenatal care, women and their
foetuses with pre gestational diabetes are associated with increased
risks of adverse pregnancy outcomes [7-11].
The first population-based epidemiological study on fertility
rates over time among women with Type 1 diabetes was conducted
in Sweden during 1965 to 2004 [12]. The lowest standardized fertility
ratios were observed among women who had their first hospitalization
for diabetes in the earliest years. The presence of diabetic microvascular
or cardiovascular complications was associated with particularly low
fertility, essentially regardless of year of first hospitalization.
Infertility risk factors related to diabetes [5]:
Menstrual abnormalities
Shortening of reproductive period (late menarche and premature
menopause)
Poor glycemic control and presence of diabetes complications
Hyperandrogenism and polycystic ovary syndrome
Autoimmunity (Hashimoto's thyroiditis and antiovarian
autoantibodies)
Sexual dysfunctionWith changing dietary and lifestyle patterns, the prevalence of
obesity is increasing, thus raising the incidence of Type 2 diabetes
during the reproductive years. Going in this direction, the disease
can be linked to polycystic ovarian syndrome, the most common
hormonal disorder among women of reproductive age, and a leading
cause of infertility. Legro et al. showed that PCOS women are at
significantly increased risk for impaired glucose tolerance and Type
2 diabetes mellitus at all weights and at a young age [13]. A study by
A mini et al. showed that PCOS is highly prevalent in Type 2 diabetic
patients [14].
Again, obesity is common in both PCOS and Type 2 diabetic
women. Studies show that obese women seeking pregnancy
experience longer times to conception, unrelated to age and to cyclic
regularity, which is suggestive of alterations in ovarian function
during the periconceptual period [15,16].
Diabetes and the Preconception Care:
Preconception care is defined as a care that aim to identify and
modify risks during pregnancy and improves pregnancy outcome
through prevention and management. It is very alarming that 50% of
all pregnancies are unplanned [17]. Improved preconception care is a
mandatory component for women with diabetes.Diabetes affects women in many ways, and one of them is the
focus of the present discussion – the association between diabetes
mellitus and planning conception.Women with diabetes should be
informed about the benefits of preconception glycaemic control
at each contact with healthcare professionals, from adolescence
onwards [18]. Many of the complications of diabetes mellitus during
pregnancy can be prevented by optimizing maternal health in the
preconception period [19].
Periconceptional period is one of the most vital periods in a
woman’s life especially if she is suffering from any major illness like
diabetes. Preconception care for women with diabetes is an effective
means to reduce the incidence of adverse pregnancy outcomes
[20-23]. Diabetic mothers are vulnerable to early pregnancy losses
together with an increased incidence of congenital malformations
in infants. Therefore, optimal medical care and pre conceptional
counselling becomes a must in such patients [24]. This is best
accomplished through a multidisciplinary team approach including
a diabetologist, obstetrician, a dietitian, and other specialists as and
when necessary.
Education in self management skills have a special role in
diabetes. This model of care is important for patients to achieve the
level of sustained glycemic control necessary to prevent congenital
malformations. All diabetic women of child-bearing potential should
be counselled about the risks of unplanned pregnancy and their
use of appropriate contraception should be assured until metabolic
control is achieved and conception is attempted. The first few weeks
of pregnancy, when a woman may not be aware of her ongoing
pregnancy, are particularly important because diabetic embryopathy
induced by hyperglycaemia develop during this time [25,26].
Diabetic embryopathy includes the following congenital
malformations in the fetus and are strongly related to the degree of
hyperglycaemia in the periconceptional period:
In women with advanced complications of diabetes, weighing the
risk of a pregnancy to their health versus the desire for child bearing
is particularly important.
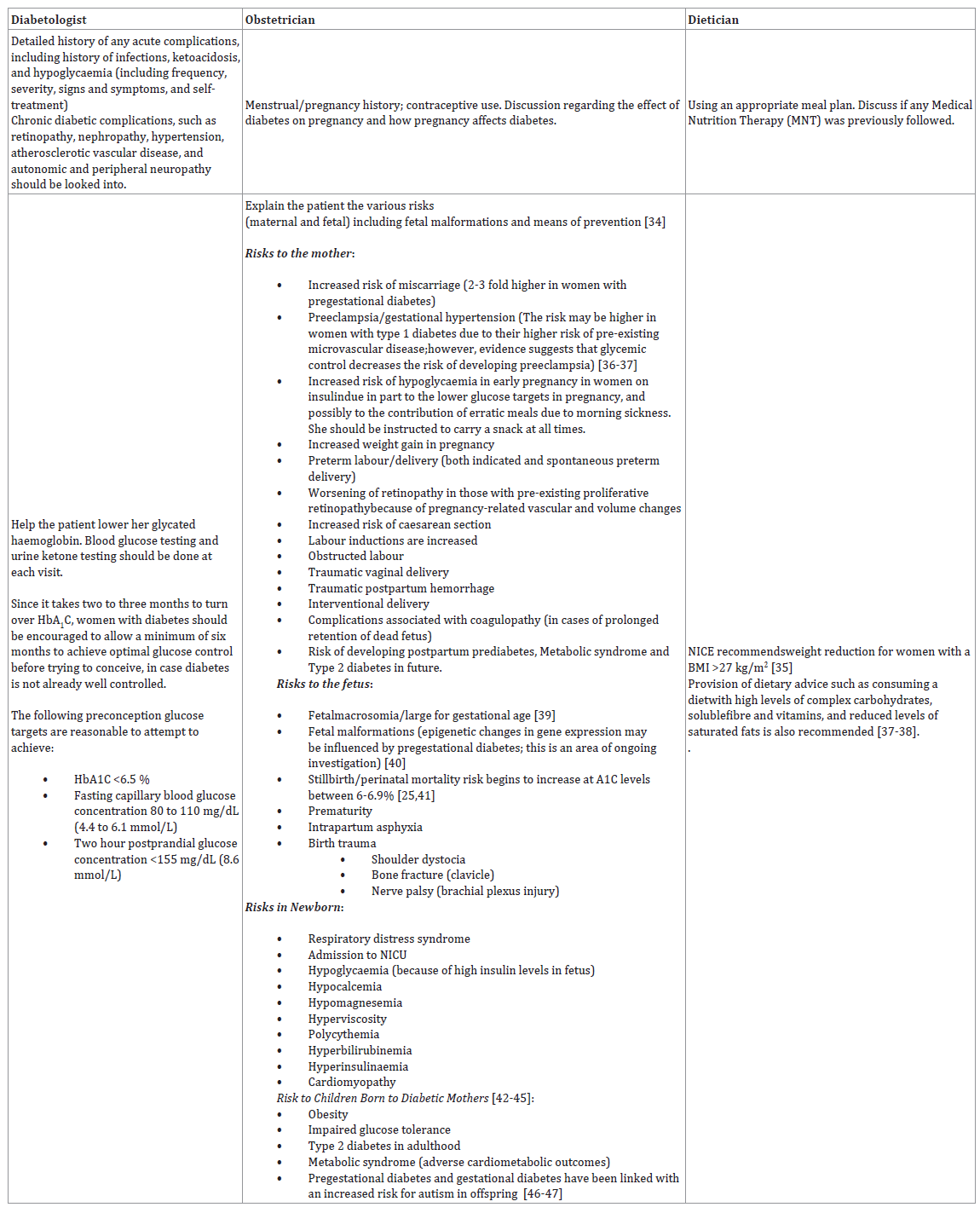
The Goals and the Roles:
Women with diabetes should be empowered to take control
of their own disease process. Therefore, its very important that the
goals and specific roles of each member of the team should be clear
[31]. Women with type 2 diabetes may be less likely to prepare for
pregnancy and achieve good glycemic control compared with those
with type 1 diabetes [32,33]. While the risk of pregnancy complications
may be similar for women with type 1 and type 2 diabetes, women
with type 1 diabetes are more likely to have pre gestational micro
vascular complications and are at higher risk of developing severe
hypo- and hyperglycaemia and diabetic ketoacidosis.The above constitutes an integrated model of care, demanding
coordination of the roles of the different team members. Motivation
for intensive self-management is dependent on the team’s approach
to imparting knowledge and skills to women with diabetes.
Comprehensive and ongoing patient education is critical for shared decision-making about management goals and medication changes and for helping patients meet the considerable demands of self-care.
Support system, includes family and work environment. Psychosocial
status including adherence issues, social support network, and stress
factors related to both diabetes and pregnancy should be discussed.
Based on the above information gathered, these professionals
will review the patient’s current management plan and develop a
comprehensive treatment plan.
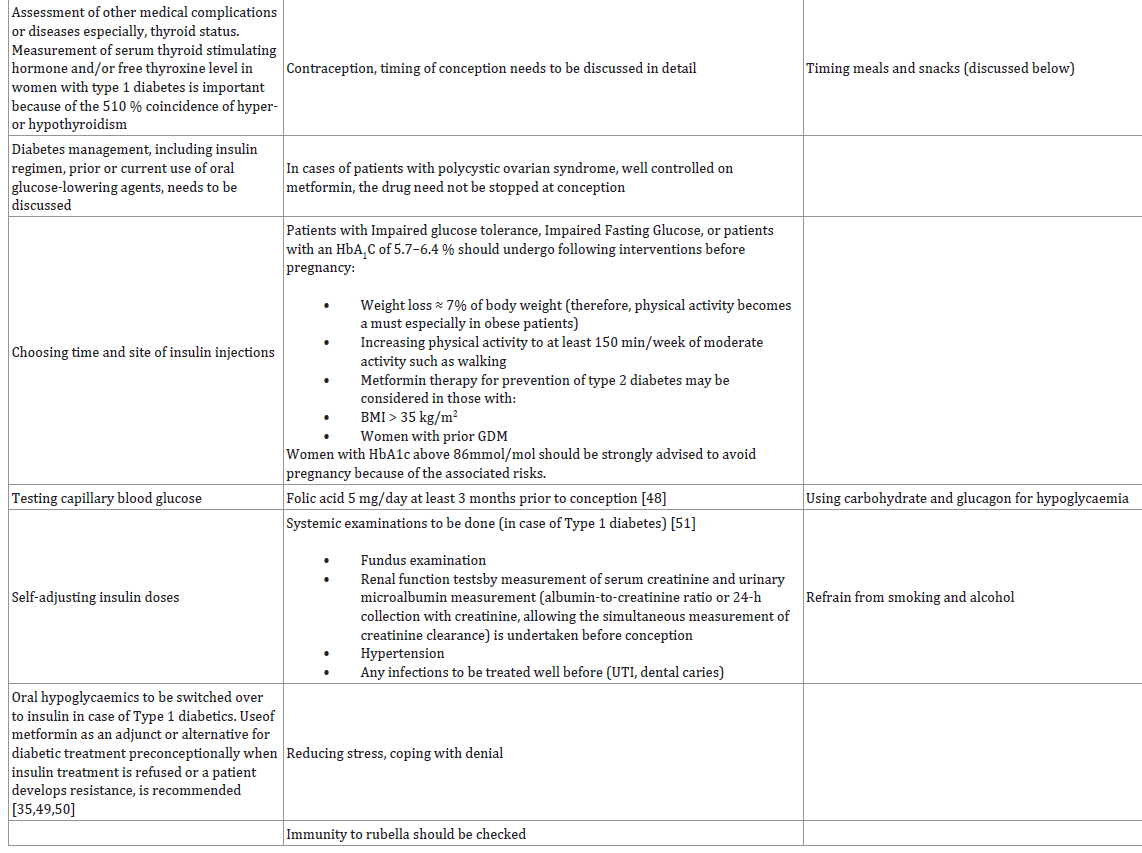
Contraindications to pregnancy:
The NICE guideline states that an HbA1C > 10% is a
contraindication to pregnancy. In contrast ADIPS suggests that
impaired renal function as measured by a serum creatinine> 0.2
mmol/L should be a contraindication to pregnancy.Role of Diet and Nutrition Therapy in the Management of Diabetes:
Diet is one of the most important behavioural aspects of diabetes
treatment. Understanding how different food intakes affect glycemia
and developing a food plan of meals and snacks helps women reduce
glucose fluctuations and manage fluctuations that occur.The desired outcome of the preconception phase of careis
to lower HbA1C test values to a level associated with optimal
development during organogenesis. In order to achieve this goal,
diet and nutrition has a great role. Nutrition history includes weight
changes, history of eating disorders, gastrointestinal problems, and
lifestyle considerations. Diet recall or food diaries may be of benefit
in identifying specific problems within the meal plan.
Calculation of caloric needs based on height, weight, age, and
activity level with development of a meal plan, including distribution
of calories, carbohydrate, fat, and protein to achieve optimal nutrition
while maintaining appropriate weight and acceptable glycemic
control is the need of the hour.
Medical Nutrition Therapy for Diabetes should consider the
following key aspects:
Consistency in day-to-day carbohydrate intake at meals and
snacks
Weight management and increased physical activity
Caloric intake (balanced with caloric expenditure)
Nutritional content (balance of selected protein,
carbohydrates, and fats)
Timing of meals and snacks
Adjusting insulin (in case of Type 1 diabetics) for variations
in blood glucose, food, or activity
Meal-insulin timing
Rallis in his study [51]concluded that a high-fat, low-carbohydrate,
ketogenic diet may prove to be a more effective dietary intervention in
the treatment of type 2 diabetes mellitus [52,53], whereas the present
nutritional guidelines appear biased towards the promotion of
carbohydrate-rich diets as mentioned above. The concept behind
a ketogenic diet uses the idea that dietary macronutrient content
modification promotes a shift from a carbohydrate to a lipid dominant
metabolism. In order to achieve a ketogenic state, carbohydrate
intake must be restricted to about 10% of total dietary intake. Protein
and fat should make up ~20% and ~70% of the diet, respectively
[54]. Under these conditions, the body begins to upregulate lipolytic
enzymes and bypass the dependence on glucose for energy [55].
Hallberg et al did assess compliance of the ketogenic diet among
diabetic patients using objective serum ketone monitoring and
demonstrated that 87% of their participants were able to maintain a
ketogenic diet for at least a year [56]. Dietary fats appear to play a role
in mood stability [57], and endogenously produced ketone bodies
(by-product of a ketogenic diet) naturally suppress appetite [58] both
of which may assistin improving patient satisfaction and compliance
with this nutritional methodology. A recent meta-analysis by
Sainsbury et al however found that while carbohydrate-restricted
dietsproduced greater reductions in HBA1C at 3 and 6 months, there
was no statistically significant difference at 12 or 24 months [59].
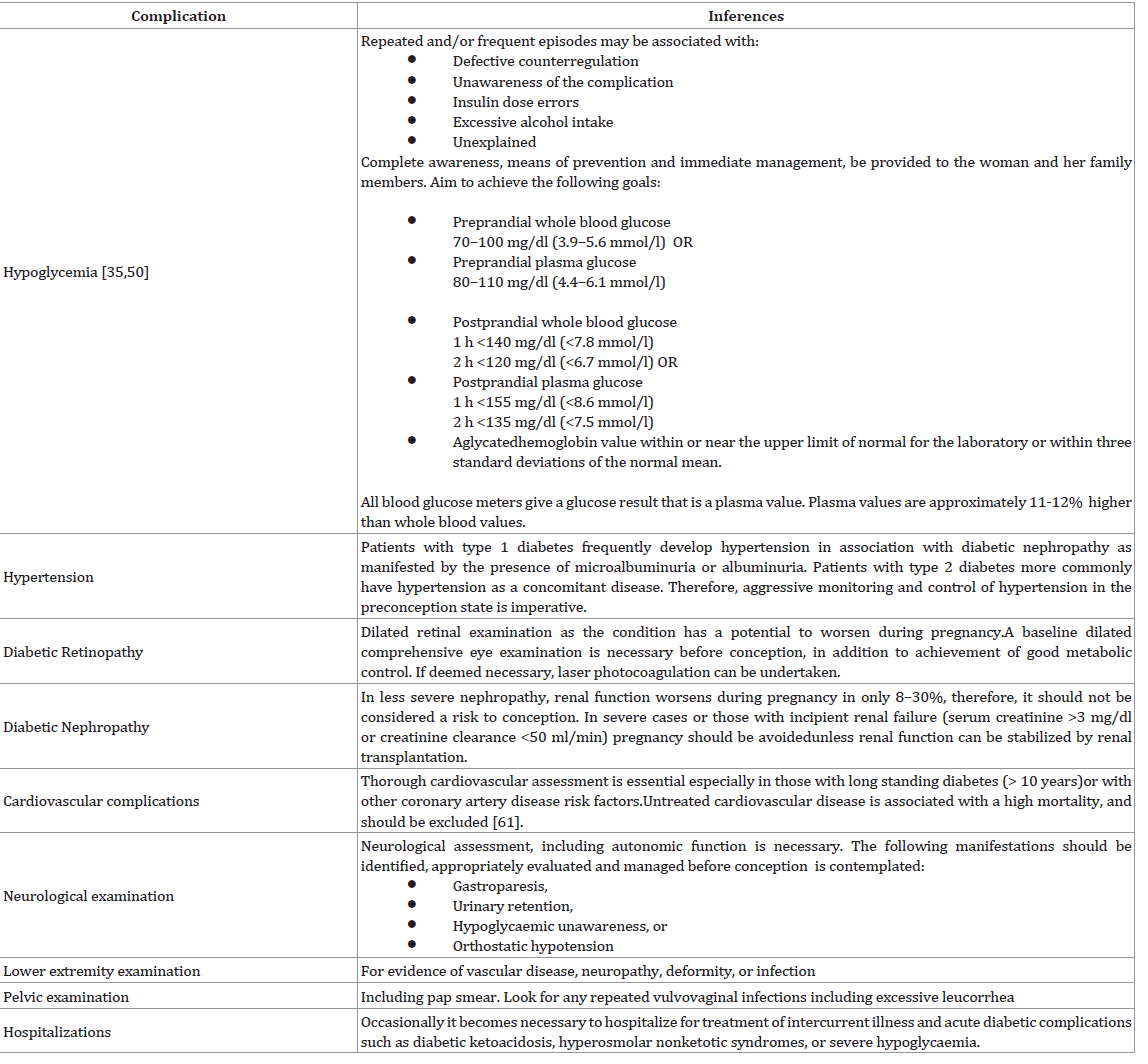
Associated Complications and Management:
High risk of diabetic complications and potential risks for
pregnancy-related complications [60] require a detailed physical
examination initiating with a blood pressure measurement
(including orthostatic changes) before conception with special
emphasis on the following [10]:Counselling and Continued Care:
The counselling sessions are important primarily for patient
education, motivation, and instruction in more effective management
strategies. At each visit, it is extremely important to make sure that
the patient has understood what is being discussed and instructed.
Evaluation of self monitoring of blood glucose; observation of
technique used by the patient and to correlate test with the laboratory;
testing log of the patient should be reviewed for appropriate timing
of testing, frequency of testing, and values. Make sure that the patient
has understood the insulin algorithms, identify the problem areas and
reinstruct.Evaluation of frequency, duration and timing of hypoglycaemic
and hyperglycaemic episodes with an attempt to identify its’ cause,
are reviewed. Monthly HbA1C measurements prior to pregnancy
are needed. Review the exercise plans, including timing, duration,
and intensity as it relates to her tolerance of the activity.
Review with the nutritionist/dietician is extremely important.
Root cause of many of the associated complications can be identified
tracking the food records of each day (with timings), the blood
glucose values before and after those particular meals and the amount
of insulin injected. Review weight changes and determine the
appropriateness of the prescribed meal plan and adjust as necessary.
Unfortunately, unplanned pregnancies occur in about twothirds
ofwomen with diabetes, precluding adequate preconception
care and leading to apersistent excess of malformations in their
infants [62]. There are no contraceptive methods that are specifically
contraindicated in women with diabetes.
Compliance is the sole issue seen in many patients. Again,
counselling has a key role in overcoming the patient’s resistance.
Stress issues should be discussed in detail. Explore ways and give
suggestions on how to cope with it.Reinforce the importance of the
overall treatment plan with the patient.
In the end, the importance of carefully planning a pregnancy and
the need for effective contraceptionand avoiding pregnancy until a
good glycemic control is achieved, should again be elaborated. The
contraceptive methods with proven high degrees of effectiveness
are to be preferred. Together with this, there is a need to review the
current medications and their safety in pregnancy.
References
5. Livshits A, Seidman DS (2009) Fertility Issues in Women with Diabetes. Women's Health. 5: 701-707.