International Journal of Otorhinolaryngology
Download PDF
Case Report
*Address for Correspondence: Young Joon Seo, MD, PhD, Department of Otolaryngology, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 220-701,Korea, Tel: +82-33-741-0642; E-mail: okas2000@yonsei.ac.kr
Citation: Lee YS, Ku CH, Park SY, Seo YJ. Assessment and Treatment of Spontaneous Temporal Bone Meningoencephalocele for Hearing Gain. Inter J Otorhinolaryngology. 2015;2(2): 3.
Copyright © 2015 Seo YJ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolaryngology| ISSN: 2380-0569 | Volume: 2, Issue: 2
Submission: 02 November, 2015 | Accepted: 03 December, 2015 | Published: 08 December, 2015
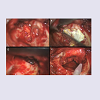
Through the facial recess, incus-stapes joint was separated with erosion on a short process of incus. We supposed that this might cause the conductive hearing loss on left ear. After the incus and the head of the malleus were removed, the bone defect was exposed ( Figure 4). We confirmed the CSF leakage around the defect in the surgical field. The size of the defect was 8 mm X 8 mm and the amount of herniated tissue was small. With coagulation of the herniated tissue, we reduced it into the intracranial compartment and covered the bony defect with deep temporalis fascia. Instead of dural suturing, we used a “Sandwich” technique in which conchal cartilage was inserted into the dehiscence with a fibrinogen-based collagen fleece (TachoComb®), and sealed the defect with artificial glue (Fibringlue®). With the “Sandwich” method, the middle cranial fossa dura was smoothly detached 3 or 4 mm from the bony borders of the defect with an elevator. The final sizes of the cartilages were slightly larger (1 to 2 mm) than that of the defect. The implant was placed in the intracranial compartment between the dura and the petrous bone, such that it was held in place by gravity and intracranial pressure. After this, we applied fibrin glue over the cartilage. Finally, to treat the hearing impairment, a 2.0 mm partial ossicular replacement prosthesis (PORP) was applied.
A follow-up MRI revealed that there was no herniation of the brain into the middle ear cavity and no mucosal hypertrophy. We plan to repair the opposite site via the same transmastoid approach,but the patient wants to observe the symptoms without any surgery.
Assessment and Treatment of Spontaneous Temporal Bone Meningoencephalocele for Hearing Gain
Young Sub Lee, Cheol Hyo Ku, Sang Yoo Park and Young Joon Seo*
- Department of Otorhinolaryngology, Yonsei University Wonju College of Medicine, Wonju, Korea
*Address for Correspondence: Young Joon Seo, MD, PhD, Department of Otolaryngology, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 220-701,Korea, Tel: +82-33-741-0642; E-mail: okas2000@yonsei.ac.kr
Citation: Lee YS, Ku CH, Park SY, Seo YJ. Assessment and Treatment of Spontaneous Temporal Bone Meningoencephalocele for Hearing Gain. Inter J Otorhinolaryngology. 2015;2(2): 3.
Copyright © 2015 Seo YJ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Otorhinolaryngology| ISSN: 2380-0569 | Volume: 2, Issue: 2
Submission: 02 November, 2015 | Accepted: 03 December, 2015 | Published: 08 December, 2015
Introduction
Meningoencephaloceles in the temporal bone originate from defects in the bony floor of the lateral skull base, i.e., in the upper surface of the temporal bone, and can lead to Cerebrospinal Fluid (CSF) leaks or meningitis [1]. Trauma, surgery, and malignancy most commonly produce these defects, but the spontaneous development of these complications without identifiable causes is less common [2]. The defects are conventionally repaired through a limited subtemporal craniotomy with elevation of the temporal lobe, or through a combined transmastoid and Middle Cranial Fossa (MCF) approach [3-6]. A more conservative intervention through the mastoid alone has been proposed by some authors in order to reduce the morbidity of the procedure. Combined cranioplasty techniques often are recommended for treating larger bone defects.With the aim of increasing the understanding and awareness of treatments for meningoencephaloceles in the temporal bone, we present the following case report of a satisfactory transmastoid repair of a spontaneous meningoencephalocele.
Case Report
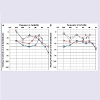
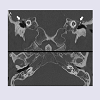
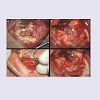
A 54-year-old man with slow progressive hearing impairment for three months was referred to the otorhinolaryngology clinic. He had no history of chronic otitis media or ear surgery. On otoscopy, there were no definite effusions in his ears. His immediate audiometry showed conductive hearing loss (30 dB in the left ear and 20 dB in the right ear, Figure 1). Air-bone gaps at low and middle frequencies were noticeably larger than those at high frequencies. While neurologic examinations did not produce any abnormal findings, computed tomography (CT) scanning revealed an oval, dense soft tissue mass in the middle ear cavity, small bone defects in the tegmen tympani, and effusion in the mastoid cavity on each side ( Figure 2). Based on the results of Magnetic Resonance Imaging (MRI), we supposed that both-sided meningoencephaloceles through an approximately 8 mm defect were present in the tegmen tympani, but the cortical floor of the middle fossa was thin bilaterally. A meningoencephalocele was diagnosed. The patient consented to undergo repair of the tegmental defect via the mastoid approach in the left ear first, because the defect was small and his hearing threshold was worse in the left ear.During surgery, we followed a surgical plan conventionally used to repair small tegmen plate defects causing brain hernias: a retro-auricular transmastoid approach using soft tissue grafts and cartilage ( Figure 3). This is the best way to ensure minimal morbidity in patients who have mild to moderate conductive hearing loss with the involvement of the ossicular chain in the attic. A complete mastoidectomy with the canal wall down was performed so that the boundaries of the tegmen defect could be demarcated with a broad surgical field.
Figure 3: Operative findings. (A) A mass of meningoencephalocele (arrow) was revealed after the mastoid cortical bone was removed. (B) After canalwall-down mastoidectomy with removal of the incus and the head of the malleus, demarcation of the dural defect was possible (arrowhead). (C) Conchal cartilage was harvested through an external auricular approach. (D) With coagulation of the herniated tissue, we reduced it into the intracranial compartment and covered the bony defect with deep temporalis fascia (arrowhead).
At his 3-month follow-up visit, the patient had no progressive hearing loss on right ear and decreased gap of bone and air conduction on left ear ( Figure 5).
A follow-up MRI revealed that there was no herniation of the brain into the middle ear cavity and no mucosal hypertrophy. We plan to repair the opposite site via the same transmastoid approach,but the patient wants to observe the symptoms without any surgery.
Discussion
A meningoencephalocele is, by definition, an extension of the cranial contents beyond the confines of the skull. Despite various names according to the content of the herniated tissue (e.g., meningocele versus meningoencephalocele), the term meningoencephalocele may be used broadly in reference to the temporal bone [1]. Meningoencephaloceles can be classified into cranial and basal varieties; cranial meningoencephaloceles typically involve the occipital and frontonasal regions, while lateral temporal lobe meningoencephaloceles and midline temporal lobe meningoencephaloceles present as masses in the sphenoid sinus [3-6]. Our patient presented a lateral temporal lobe meningoencephalocele with a small spontaneous defect of the tegmen tympani. Furthermore, there were no suspicious causes for the hernia bilaterally. He did not have any evidences of otitis media. We thought this herniation might be occurred spontaneously. The incidence of meningoencephalocele remains rare, with estimations between 1/3,000 and 1/35,000 [3]. Acquired CSF leaks are noted in most cases of meningoencephalocele [7]. Thus, a description of a surgical technique for a small defect (i.e., a lateral temporal bone meningoencephalocele with no history of CSF leakage) would be meaningful as an example of a minimally invasive treatment.We chose the active treatment from several options for intervention and conservative treatment. The symptoms of which the patient complained were ongoing conductive hearing loss and ear fullness. There was mucosal hypertrophy on the CT images because of obstructions of the antrum. The herniated mass had filled.the attic and compressed the ossicular chains. On left ear, erosion of incus and separation of incus-stapes joint were detected. This observation suggested a possible treatment. However, we achieved minimal invasiveness with the “Sandwich” method in a transmastoid approach, with the result that the patient regained some hearing [8]. Sanna et al. reported on the treatment of meningoencephalic hernias with the transmastoid approach alone in 93/122 patients, including 55 with total obliteration of the middle ear cavities [9]. There were no complications associated with this approach, while one case of meningitis and one case of epidural hematoma occurred following the MCF approach. Zanetti et al. treated seven patients with petrous bone dehiscences less than 3 cm in diameter by the transmastoid route [8]. None of the patients suffered from immediate side effects related to the operation. In our patient, the successful repair accompanied by a hearing gain was unique for treatments of meningoencephaloceles.
It is meaningful that the herniated mass disturbing the ossicular chains could be repaired by a simple method that improved the hearing thresholds. There were several possible surgical treatments, including a middle fossa craniotomy alone, a middle cranial fossa approach, a transmastoid approach, and a combined middle cranial fossa/transmastoid approach [10-13]. The choice of surgical approach should be driven by the etiology of the defect, the site and extent of the bony defect and the brain hernia, the type and degree of hearing loss, the presence of chronic infection in the middle ear, and the intraoperative finding of active CSF leakage. There is no consensus on which method is preferred, and any repairs should be customized for the patient’s specific defect. The middle cranial fossa extradural approach has the potential for higher surgical and perioperative morbidity on account of the craniotomy, the temporal bone retraction, the need for a lumbar drain, and the long hospital admission. While the transmastoid approach provides a less secure repair, it has minimal morbidity and is less destructive to the hearing structures because it follows a direct path to the lateral cranial base, often leading to only mild or moderate conductive deafness [14,15]. We recommend “Sandwich” repair via the transmastoid approach for cases with defects less than 1 cm without active CSF leakages.
Many biological and synthetic materials currently are used to create waterproof seals of bone defects in meningoencephaloceles of the temporal bone [16-18]. Autologous and homologous bone or cartilage grafts, local pedicles or soft tissue flaps, as well as many alloplastic materials (bone substitutes, cements, ceramics, metals, polymers, acrylics and their composites) have been used. Cartilage grafts are sufficiently elastic, but offer little resistance to deformation, and often are reabsorbed to various extents or converted to fibroid tissue a year after their insertion, so additional protection is needed. In our “Sandwich” method, sheets of fascia are added to secure a watertight closure of the defect. The use of biological sealants, such as fibrin glue guarantee support for the reconstruction inside the cavity.
Early intervention before a larger defect occurred was very important in this successful repair with good hearing improvement. CT and MRI images helped us determine which surgical method would be appropriate. Proper initial assessments by otologists prior to treatment for meningoencephaloceles of the temporal bone are needed. This case will help to guide clinicians to make better decisions for the treatment of spontaneous meningoencephaloceles of the temporal bone without CSF leakages.
Acknowledgements
Financial disclosure informationThis work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (2015R1C1A1A02036354).
References
- Golding-Wood DG, Williams HO, Brookes GB (1991) Tegmental dehiscence and brain herniation into the middle ear cleft. J Laryngol Otol 105: 477-480.
- Gladstone HB, McDermott MW, Cooke DD (1995) Implants for craniopalsty. Otolaryngol Clin North Am 28: 381-400.
- Wind JJ, Caputy AJ, Roberti F (2008) Spontaneous encephaloceles of the temporal lobe. Neurosurg Focus 25: E11.
- Brown NE, Grundfast KM, Jabre A, Megerian CA, O’Malley BW Jr, et al. (2004) Diagnosis and management of spontaneous cerebrospinal fluidmiddle ear effusion and otorrhea. Laryngoscope 114: 800-805.
- Glasscock ME 3rd, Dickins JR, Jackson CG, Wiet RJ, Feenstra L (1979) Surgical management of brain tissue herniation into the middle ear and mastoid. Laryngoscope 89: 1743-1754.
- Wilkins RH, Radtke RA, Burger PC (1993) Spontaneous temporal encephalocele. Case report. J Neurosurg 78: 492-498.
- Sdano MT, Pensak ML (2005) Temporal bone encephaloceles. Curr Opin Otolaryngol Head Neck Surg 13: 287-289.
- Zanetti D, Garavello W, Gaini L (2011) Transmastoid repair of temporal meningoencephaloceles and cerebrospinal fluid otorrhea. Otorhinolaryngol Clin Int J 3: 31-41.
- Sanna M, Fois P, Russo A, Falcioni M (2009) Management of meningoencephalic herniation of the temporal bone: Personal experience and literature review. Laryngoscope 119: 1579-1585.
- Ramdsen RT, Latif A, Lye RH, Dutton JE (1985) Endaural cerebral hernia. J Laryngol Otol 99: 643-651.
- Piattelli A, Franco M, Ferronato G, Santello MT, Martinetti R, et al. 1977)Resorption of composite polymer-hydroxyapatitie membranes: a time-course study in rabbit. Biomaterials 18: 629-633.
- Nahas Z, Tatlipinar A, Limb CJ, Francis HW (2008) Spontaneous meningoencephalocele of the temporal bone: clinical spectrum and presentation. Arch Otolaryngol Head Neck Surg 134: 509-518.
- Semaan MT, Gilpin DA, Hsu DP, Wasman JK, Megerian CA (2011) Transmastoid extradural-intracranial approach for repair of transtemporal meningoencephalocele: a review of 31 consecutive cases. Laryngoscope 121: 1765-1772.
- Oliaei S, Mahboubi H, Djalilian HR (2012) Transmastoid approach to temporal bone cerebrospinal fluid leaks. Am J Otolaryngol 33: 556-561.
- Boo SH, Goh YB, Han CS (2013) Repair of spontaneous cerebrospinal fluid otorrhea from defect of middle cranial fossa. Korean J Audiol 17: 148-151.
- Dormer KJ, Bryce GE, Hough JV (1995) Selection of biomaterials for middle and inner ear implants. Otolaryngol Clin North Am 28: 17-27.
- Blayney AW, Williams KR, Erre JP, Lesser TH, Portmann M (1992) Problems in alloplastic middle ear reconstruction. Acta Otolaryngol 112: 322-327.
- Remacle M, Marbaix E, Musetin V (1991) Tissue integration of the collagenhydroxylapatitie implant: histological examination in canine bone and surrounding tissues. Eur Arch Otorhinolaryngol 248: 337-341.