Journal of Emergency Medicine & Critical Care
Download PDF
Case Report
*Address for Correspondence: Elizabeth M Dorn, MD DTMH, Assistant Professor of Emergency Medicine, Division of Emergency Medicine, University of Washington, Box 359702, 325 Ninth Ave, Seattle, WA 98104-2499, USA, E-mail: edorn@u.washington.edu
Citation: Dorn EM. Electrical Storm - Brugada’s Syndrome- A Case Report and Literature Review. J Emerg Med Critical Care. 2015;1(1): 5.
Copyright © 2015 Dorn EM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Emergency Medicine & Critical Care | Volume: 1, Issue: 1
Submission: 23 July, 2015 | ISSN: 2469-4045 |Accepted: 07 August, 2015 | Published: 12 August, 2015
Reviewed & Approved by: Dr. Christopher R. Tainter, Assistant Professor, Department of Emergency Medicine, University of California, USA
Risk factors for BrS include Asian descent, male gender - with a RR 8.8(4)- and middle age (mean age 41 +/-15 years) [1]. Dysrhythmias are more likely during periods of vagal prominence-at night, during sleep and post prandial [3,17,18] as with this patient. Studies in Thailand showed that 84% of dysrhythmias occur at night [5].
Electrical Storm - Brugada’s Syndrome- A Case Report and Literature Review
Elizabeth M Dorn*
- Division of Emergency Medicine, University of Washington, WA USA
*Address for Correspondence: Elizabeth M Dorn, MD DTMH, Assistant Professor of Emergency Medicine, Division of Emergency Medicine, University of Washington, Box 359702, 325 Ninth Ave, Seattle, WA 98104-2499, USA, E-mail: edorn@u.washington.edu
Citation: Dorn EM. Electrical Storm - Brugada’s Syndrome- A Case Report and Literature Review. J Emerg Med Critical Care. 2015;1(1): 5.
Copyright © 2015 Dorn EM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Emergency Medicine & Critical Care | Volume: 1, Issue: 1
Submission: 23 July, 2015 | ISSN: 2469-4045 |Accepted: 07 August, 2015 | Published: 12 August, 2015
Reviewed & Approved by: Dr. Christopher R. Tainter, Assistant Professor, Department of Emergency Medicine, University of California, USA
Abstract
Brugada Syndrome is an uncommon and potentially lethal disease with a high potential for morbidity if not diagnosed and treated early. New findings have changed detection and management. This case report illustrates a presentation of symptomatic dysrhythmia and aborted sudden cardiac death (SCD) in a patient who was found to have Brugada Syndrome (BrS) and demonstrates the presentation of electrical storm and the rapidly changing morphologies of the electrocardiogram (ECG) over time, characteristic of the disease.Emergency Physicians should be aware of the varying presentations of Brugada Syndrome and understand:1. Variability and evanescent nature of the ECG changes diagnostic for the disease;
2. Conditions and medications that can unmask or exacerbate the dysrhythmias;
3. The need for judicious use of medications in the Emergency Department and timely referral and treatment.
This article presents the case and discusses the incidence, presenting symptoms, diagnostic criteria and course of treatment for this particular diagnosis, as well as a review of the pertinent literature in the past ten years.
Introduction
Brugada Syndrome is one of a handful of identified primary electrophysiological disorders with a proclivity for malignant cardiac dysrhythmias and SCD, notably in younger patients. Brugada Syndrome is channelopathy, primarily a sodium channel abnormality, and deemed responsible for at least in 20% of sudden cardiac death in patients with structurally normal hearts [1]. Symptomatic patients with this defect are at higher risk for recurrent sudden cardiac death events. There is a growing body of research elucidating this disease and it is an important condition for Emergency Physicians to identify, make timely diagnosis and treat dysrhythmias appropriately.Case Report
A previously healthy 50-year old Chinese man was brought in by ambulance at dawn. According to his wife he was speaking to her in bed when suddenly he lay back, stared at the ceiling and grimaced, clenched his fists and did not respond for “about 5 minutes.” He then regained composure but was amnestic of the event, felt fearful and said he “didn’t feel well” without the ability to further elaborate. Medics who were dispatched to the scene found the patient upset, diaphoretic, with vital signs within normal limits in the field and en route.The patient had no significant past medical history, no history of similar episodes and had been feeling fine previous to the event. He complained of feeling a little bit nauseated and scared, but otherwise well. He reported no preceding palpitations, chest pains or pressure, dyspnea or dizziness. He denied recent headache, neck pain or neurological symptoms, chest pain, dyspnea, palpitations, syncope or change in exercise tolerance, fevers, abdominal pain, diarrhea or melena. Family history was negative for heart disease, stroke, seizure, sudden death, or other major diseases. The patient took no medication, prescription, over-the-counter or herbal.
Upon arrival, the patient was alert and composed but anxious with mild forehead diaphoresis. His vital signs showed temperature of 98.1, blood pressure 134/61, pulse 64, respiratory rate of 20 and oxygen saturation of 99% on room air. His physical exam showed a trim, athletic man, with clear lung sounds, no jugular venous distension, heart sounds without murmur or gallops, peripheral pulses intact and was otherwise normal.
During the physical exam, the patient abruptly grimaced, clenched his fist, flexed his arms, and stared at the ceiling unresponsively. This posturing was accompanied by the following telemetry and oximetry monitor tracings with no palpable carotid pulse (see Figure 1).
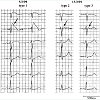
His initial electrocardiogram (ECG) showed a pattern consistent with Type 2 BrS morphology (see Figure 2 Figure 2).
Laboratory tests (chemistries, cardiac enzymes and blood cell counts) were all within normal limits.
During the Emergency Department (ED) stay, the patient subsequently had recurrent runs of symptomatic polymorphic ventricular tachycardia (VT) which seemed to worsen in frequency after a lidocaine bolus had been given. Defibrillation pads were placed on the patient and he received a total of 18 defibrillating shocks for recurrent ventricular fibrillation (VF) while in the ED.
Serial ECGs over 2 hours, taken during quiescent moments within electrical storm, showed evolution of the ECG which was concerning for ischemia, seen below (see Figure 3).
The ECG evolved into anterior ST elevations and the patient was taken emergently to angiography with concern of acute anterior ischemia. In the angiography suite, the patient continued to have runs of VT requiring repeated defibrillation. The angiogram showed widely patent coronary arteries, no inducible vasospasm and grossly normal structure and function of the heart. He was later diagnosed with Brugada Syndrome with genetic testing, and subsequently had an AICD implanted as definitive treatment.
Discussion
Brugada Syndrome (BrS) was first described in 1992, by Portuguese cardiologists, the Brugada brothers, who noted an increase in dysrhythmias and sudden cardiac death (SCD) in patients with right bundle branch block (RBBB) morphology. It is characterized electrocardiographically as RBBB morphology, with elevated J point and ST segments in the right precordial leads (V1-3) and episodes of malignant ventricular arrhythmias. It has been found to be linked to primarily cardiac sodium channel defects, [2]. BrS is considered a leading cause of SCD in patients with structurally normal hearts, and a leading cause of death, second only to automobile accidents, in patients less than 40 years old, in countries where the defect is endemic [3].Though BrS was first described in Europe, the highest prevalence is in Southeast Asia. Natives of this part of the world have long recognized a phenomenon of young men dying in their sleep and named it Lai Tai (“died during sleep”) in Thailand, Bangungut (“moaning and dying during sleep”) in the Philippines and Pokkuri (“sudden unexpected death at night”) in Japan [3]. Researchers had been investigating the epidemic of sudden nocturnal death syndrome in Southeast Asian young men since the early 1980s. In 1997, Nadamnee and colleagues working with the Thai population postulated the syndrome was the same as BrS, which was later confirmed through genetic research [3-5]. BrS is associated with several genetic defects of cardiac sodium channels, most prominently SCN5A which encodes for the alpha-subunit dominant in cardiac sodium channels. Genetic defect in SCN5A are found in up to 30% of cases, although calcium channel mutations and conduction abnormalities of the RV outflow track epithelium involving both sodium and calcium channel depolarization conduction abnormalities have also been implicated [5-9].
Unlike congenital Long QT syndrome, which presents with harbingers of prior syncope before significant dysrhythmia, BrS usually presents initially with a life threatening event [10], cardiac arrest or recurrent runs of symptomatic VT or VF requiring repeated defibrillation - known as electrical storm - as seen in this patient. Patients with Brugada Syndrome can, however, present with complaints of syncope or nocturnal agonal breathing, as frequently noted in the Thai population [3-5].
There are three types of BrS morphology characteristic ECG tracings:
Type 1 is diagnostic of BrS and is characterized by a coved STsegment elevation ≥2 mm followed by a negative T wave in more than one right precordial lead. Type 2 BrS displays a saddleback configuration with a high take-off ST-segment elevation of ≥2 mm, a trough displaying ≥1 mm ST elevation, and either a positive or biphasic T wave. Type 3 has either a saddleback or coved appearance with an ST-segment elevation of ≤1 mm (see Figure 4).
One study found that ECGs taken in the 2nd or 3rd intercostal spaces yield higher sensitivity [11].It is important to note that the BrS changes in ECGs of patients with BrS aren’t always present. Their ECGs are protean. Richter et al. in a study of patients with implanted defibrillators showed that the degree of ST elevation was variable, such that only one third of ECGs were diagnostic and one third were normal [12]. Nademanee also found this in his initial study in Thai men found to have Brugada syndrome [3]. Thus a single ECG tracing cannot rule it out. Furthermore, patients who do exhibit the classic tracing may vacillate between Types, as in this patient who, after presenting with initial ECG showing Type 2 morphology, subsequently developed features of Type 1 and Type 3 ECG morphology during electrical storm. In addition, the “burden” or frequency of Type 1 morphology over time [10,13] and presence of Brugada morphology in more than the precordial leads [14-16] bodes worse prognosis.
Figure 4:: Brugada ECG tracings, Type 1 and 2 with J point elevation ˃2 mm, Type 1 with ˂1 mm J point elevation. Type 1 with marked ST segment elevation andcoving or sloping ST segment and flipped T wave, without isoelectric separation. Type 2 and 3 with isoelectric or upright T wave and ST segment with frequent saddle back deformity. Arrows denote the J-point elevation.Courtesy of: Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, et al. Proposed diagnostic criteria for the Brugada syndrome: consensus report.Circulation. 2002;106(19): p 2615
Fever unmasks Brugada morphology, making it 20 times more apparent in patients when febrile [19] and was the precipitating factor for VF in 18% of patient presenting with cardiac arrest in one study [20]. Medications, most prominently those that block sodium channels can unmask ECG morphology [7,21,22].
Certain medications such procainamide, flecainide, propofol, propafenone have been found to precipitate VF [6,7]. Case reports show that diphenhydramine, bupivacaine, propofol and phenothiazinescan trigger VF. Vernooy et al. describe six patients who developed a Brugada-like ECG pattern during propofol infusionand died within hours, of irrecoverable electrical storm [6].
Many drugs unmask the BrS ECG changes, such as amiodarone, verapamil, propanolol, nitroglycerin, and antiepileptic and psychotropic drugs [1,23]. Whether or not all the medications that have been found to unmask the BrS tracings are causal in VF has yet to be elucidated, but given the observation that BrS morphology load increases risk of VF events, all drugs that could potentiate BrS morphology should be avoided in those with baseline BrS morphology.
Other factors that have been implicated include: metabolic abnormalities including hypokalemia, hyperkalemia orhypercalcemia; ingestion of alcohol, cocaine, or methanol; and exposure to carbon monoxide [1,24].
Prognosis
In two studies, patients who presented with aborted SCD (pulseless dysrhythmia requiring cardioversion) wereat highest risk for recurrent VF - 62% in Brugada et al. and 41% in Japanese population study [25,26]. Patients who presented with syncope had rates of recurrent VF of 19% and 11.8%, respectively. These are considered high-risk patients when symptomatic.
The importance of incidentally-found Brugada pattern ECG tracing is unclear, but the current recommendation is to refer on for further outpatient testing. However, a symptomatic patient - anyone who presents after aborted SCD, VT, syncope or nocturnal agonal respirations requires immediate Cardiology consult and admission [27].
Evaluation
Evaluation includes, excluding other pathological etiologies for the ECG changes. In absence of vascular, structural or electrolyte abnormalities, sodium channel blocker challenge, EPS diagnostics and genetic testing may be performed as indicated [1,10].
Treatment in the ED
Electrical storm is treated with repeated cardioversion.
If present, treat fever with antipyretics.
If BrS in suspected in any patient, it is important to avoid drugs that are deemed arrhythmogenic in these patients.
Avoid drugs that have the highest risk of electrical storm, such as procainamide, beta blockers, propofol (see Table 1) and possibly lidocaine, amiodarone, diphenhydramine, and other sodium channel blockers (see Table 1).
For a list of drugs that can unmask the Brugada pattern, access www.brugadadrugs.org
Anti-arrhythmic therapy
Isoproterenol has been recommended in treating electrical storm, though this should be considered with caution as certain mutations can accelerate into worsening electric storm.
Quinidine has been used to decrease the incidence and acuity of electrical storm [28]. However the pharmacologic treatment of Brugada syndrome is best done with cardiac or EP consultation.
Definitive treatment
An implanted defibrillator is the treatment of choice in symptomatic patients. There is much debate about how best to follow the genetically-predisposed or those with positive ECG changes but no symptoms [29]. Quinidine has been found to decrease the incidence of events [28,29]. There is some evidence to suggest that right ventricular outflow tract ablation may be curative in severe BrS [8,28].
Conclusion
Brugada Syndrome is an important and increasingly recognized phenomenon which requires early recognition, especially in younger patients, with VF arrest or other dysrhythmia, syncope, or agonal nocturnal respirations. Emergency Physicians may have the first opportunity to recognize and implement treatment for this dangerous condition. The electrical instability from BrS needs to be considered as it is treated differently than other malignant arrhythmias. ECG patterns may be initially absent, subtle or protean and cardiology or EP should be consulted as soon there is ECG evidence of BrS. Treating fever urgently may ebb electrical storm. Certain medications are contraindicated or must be used with caution in a patient suspected of having BrS. Symptomatic patients with Brugada ECG morphology requires immediate evaluation and admission for further work up, and asymptomatic patients with an ECG showing Brugada morphology should be referred for further evaluation.References
- Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, et al. (2005) Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 111: 659-670.
- Brugada P, Brugada J (1992) Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 20: 1391-1396.
- Nademanee K, Veerakul G, Nimmannit S, Chaowakul V, Bhuripanyo K, et al. (1997) Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men. Circulation 96: 2595-2600.
- Tatsanavivat P, Chiravatkul A, Klungboonkrong V, Chaisiri S, Jarerntanyaruk L, et al. (1992) Sudden and unexplained deaths in sleep (Laitai) of young men in rural northeastern Thailand. Int J Epidemiol 21: 904-910.
- Tungsanga K, Sriboonlue P (1993) Sudden unexplained death syndrome in north-east Thailand. Int J Epidemiol 22: 81-87.
- Letsas KP, Kavvouras C, Kollias G, Tsikrikas S, Korantzopoulos P, et al. (2013) Drug-induced brugada syndrome by noncardiac agents. Pacing Clin Electrophysiol 36: 1570-1577.
- Postema PG, Wolpert C, Amin AS, Probst V, Borggrefe M, et al. (2009) Drugs and Brugada syndrome patients: review of the literature, recommendations, and an up-to-date website (www.brugadadrugs.org). Heart Rhythm 6: 1335-1341.
- Nademanee K, Veerakul G, Chandanamattha P, Chaothawee L, Ariyachaipanich A, et al. (2011) Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation 123: 1270-1279.
- Watanabe H, Minamino T (2013) Role of mutations in L-type calcium channel genes in Brugada syndrome, early repolarization syndrome, and idiopathic ventricular fibrillation associated with right bundle branch block. Circ J 77: 1689-1690.
- Viskin S, Adler A, Rosso R (2013) Brugada burden in Brugada syndrome: the way to go in risk stratification? Heart Rhythm 10: 1019-1020.
- Holst AG, Tango M, Batchvarov V, Govindan M, Haunso S, et al. (2012) Specificity of elevated intercostal space ECG recording for the type 1 Brugada ECG pattern. Ann Noninvasive Electrocardiol 17: 108-112.
- Richter S, Sarkozy A, Veltmann C, Chierchia GB, Boussy T, et al. (2009) Variability of the diagnostic ECG pattern in an ICD patient population with Brugada syndrome. J Cardiovasc Electrophysiol 20: 69-75.
- Priori SG, Gasparini M, Napolitano C, Della Bella P, Ottonelli AG, et al. (2012) Risk stratification in Brugada syndrome: results of the PRELUDE (PRogrammed ELectrical stimUlation preDictive valuE) registry. J Am Coll Cardiol 59: 37-45.
- Rollin A, Sacher F, Gourraud JB, Pasquie JL, Raczka F, et al. (2013) Prevalence, characteristics, and prognosis role of type 1 ST elevation in the peripheral ECG leads in patients with Brugada syndrome. Heart Rhythm 10: 1012-1018.
- Kamakura S, Ohe T, Nakazawa K, Aizawa Y, Shimizu A, et al. (2009) Long-term prognosis of probands with Brugada-pattern ST-elevation in leads V1-V3. Circ Arrhythm Electrophysiol 2: 495-503.
- Kawata H, Morita H, Yamada Y, Noda T, Satomi K, et al. (2013) Prognostic significance of early repolarization in inferolateral leads in Brugada patients with documented ventricular fibrillation: a novel risk factor for Brugada syndrome with ventricular fibrillation. Heart Rhythm 10: 1161-1168.
- Kasanuki H, Ohnishi S, Ohtuka M, Matsuda N, Nirei T, et al. (1997) Idiopathic ventricular fibrillation induced with vagal activity in patients without obvious heart disease. Circulation 95: 2277-2285.
- Talib S, van de Poll SW (2013) Brugada syndrome diagnosed after Ramadan. Lancet 382: 100.
- Adler A, Topaz G, Heller K, Zeltser D, Ohayon T, et al. (2013) Fever-induced Brugada pattern: How common is it and what does it mean? Heart Rhythm 10: 1375-1382.
- Amin AS, Meregalli PG, Bardai A, Wilde AA, Tan HL (2008) Fever increases the risk for cardiac arrest in the Brugada syndrome. Ann Intern Med 149: 216-218.
- Brugada P, Brugada J, Brugada R (2000) Arrhythmia induction by antiarrhythmic drugs. Pacing Clin Electrophysiol 23: 291-292.
- Letsas KP, Kavvouras C, Kollias G, Tsikrikas S, Korantzopoulos P, et al. (2013) Drug-induced Brugada syndrome by noncardiac agents. Pacing Clin Electrophysiol 36: 1570-1577.
- Bardai A, Amin AS, Blom MT, Bezzina CR, Berdowski J, et al. (2013) Sudden cardiac arrest associated with use of a non-cardiac drug that reduces cardiac excitability: evidence from bench, bedside, and community. Eur Heart J 34: 1506-1516.
- Nimmannit S, Malasit P, Vasuvattakul S, Nilwarangkur S, Chaovakul V, et al. (1991) Pathogenesis of sudden unexplained nocturnal death (lai tai) and endemic distal renal tubular acidosis. Lancet 338: 930-932.
- Brugada J, Brugada R, Antzelevitch C, Towbin J, Nademanee K, et al. (2002) Long-term follow-up of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation 105: 73-78.
- Hiraoka M, Takagi M, Yokoyama Y, Sekiguchi Y, Aihara N, et al. (2013) Prognosis and risk stratification of young adults with Brugada syndrome. J Electrocardiol 46: 279-283.
- Veerakul G, Nademanee K (2012) Brugada Syndrome: two decades of progress. Cir J 76: 2713-2722.
- Belhassen B, Glick A, Viskin S (2004) Efficacy of quinidine in high-risk patients with Brugada syndrome. Circulation 110: 1731-1737.
- Viskin S, Rogowski O (2007) Asymptomatic Brugada syndrome: a cardiac ticking time-bomb? Europace 9: 707-710.
- Mizusawa Y, Sakurada H, Nishizaki M, Hiraoka M (2006) Effects of low-dose quinidine on ventricular tachyarrhythmias in patients with Brugada syndrome: low-dose quinidine therapy as an adjunctive treatment. J Cardiovasc Pharmacol 47: 359-364.