Journal of Clinical & Medical Case Reports
Download PDF
Case Report
*Address for Correspondence: Anne-Luise Thorsteinsson, Department of Cardiology, Nephrologyand Endocrinology, Nordsjællands Hospital-Hillerød, Dyrehavevej 29,DK-3400 Hillerød, Tel: +45 4829 7483; Fax: +45 4829 4783; E-mail: Anne-Luise.Thorsteinsson@regionh.dk
Citation: Thorsteinsson AL, Lomholt AF, Eiken P. Bisphosphonate-Induced Osteonecrosis of the External Auditory Canal: A Case Report. J Clin Med Case Reports. 2015;2(1): 3.
Copyright 2015 ©Thorsteinsson et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Medical Case Reports | ISSN: 2332-4120 | Volume: 2, Issue: 1
Submission: 30 January 2015| Accepted: 25 February 2015 | Published: 28 February 2015
In 2007, the patient was referred to the hospital’s endocrinology outpatient clinic for optimizing osteoporosis treatment because of back pain. An X-ray of the spine showed multiple fractures of both thoracic and lumbar vertebrae and a Dual-energy X-ray Absorptiometry (DXA) showed a T-score of minus 3.5 standard deviations (SD) in the total hip; spine could not be evaluated. The patient was shifted to ibandronate (150 mg/month).
In January 2014, the patient was treated surgically with bilateral removal of necrotic bone and reconstruction of the ear canal. Postoperatively, signs of healing were seen in both EACs, but still the patient suffered from bilateral ear pain. Unfortunately, no biopsy was taken for histological examination during treatment. Blood samples for analyzing bone turnover markers were not available, but since the patient had received three years of zoledronic acid suppressed levels of carboxy-terminal collagen crosslinks (CTX) and procollagen type I propeptides (PINP) are to be expected.
Bisphosphonate-Induced Osteonecrosis of the External Auditory Canal: A Case Report
Anne-Luise Thorsteinsson1,2*, Anne Fog Lomholt3 and Pia Eiken1,2
- 1Department of Cardiology, Nephrology and Endocrinology,Nordsjællands Hospital-Hillerød, Denmark
- 2Faculty of Health and Medical Sciences, University of Copenhagen,Denmark
- 3Department of Ear, Nose and Throat Diseases,Nordsjællands Hospital-Hillerød,Denmark
*Address for Correspondence: Anne-Luise Thorsteinsson, Department of Cardiology, Nephrologyand Endocrinology, Nordsjællands Hospital-Hillerød, Dyrehavevej 29,DK-3400 Hillerød, Tel: +45 4829 7483; Fax: +45 4829 4783; E-mail: Anne-Luise.Thorsteinsson@regionh.dk
Citation: Thorsteinsson AL, Lomholt AF, Eiken P. Bisphosphonate-Induced Osteonecrosis of the External Auditory Canal: A Case Report. J Clin Med Case Reports. 2015;2(1): 3.
Copyright 2015 ©Thorsteinsson et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Medical Case Reports | ISSN: 2332-4120 | Volume: 2, Issue: 1
Submission: 30 January 2015| Accepted: 25 February 2015 | Published: 28 February 2015
Abstract
Objective:Worldwide millions of patients are treated with bisphosphonates (BPs) for osteoporosis and cancer-associated bone diseases. In recent years rare side effects as osteonecrosis of the jaw and atypical femur fracture have been reported to be associated with long-term treatment with BP. A national register-based cohort study and eight cases of BP-associated osteonecrosis/cholesteatoma of the external auditory canalhave been reported in the world literature.
Methods:
In this study we present a case with a 76-year old female diagnosed with bilateral osteonecrosis of the external auditory canal possibly due to long-term oral and intravenous BP treatment of osteoporosis.
Conclusion:
BP-associated osteonecrosis of the external auditory canal is a rare and still relatively unknown condition. The case underlines the significant impact of the diagnosis and its complications on quality of life. Although BP induced osteonecrosis is rare, the large volume of BP prescriptions makes the number of patients at risk significant. However we still think that the benefits of therapy with BPs in osteoporosis patients with high risk of fractures outweigh the risk of osteonecrosis of the external auditory canal.
Keywords
Osteonecrosis; Osteoporosis; External ear canal; Bisphosphonate therapyIntroduction
Bisphosphonates (BP) are first-line choice for treatment of osteoporosis [1] and are efficacious in preventing and delaying cancer-related bone disease [2]. Overall, BP treatment is safe with only few serious adverse events. However, since an increasing number of patients are treated with BPs and duration of treatment is increased, rare side effects to long-term treatment have emerged [3-5]. In recent years the associations between long-term treatment with BP and osteonecrosis of the jaw (ONJ) [6-8] as well as atypical femur fracture (AFF) [9] have been identified. In addition, a recently published case report mentions a possible association between ankylosis of the temporomandibular bone and BP therapy [10].Within the last decade case reports of BP-associated osteonecrosis of the external auditory canal (EAC) have emerged [11-15]. We have identified eight cases and a Danish national register-based cohort study has described an increased risk of cholesteatoma of the EAC during long-term BP-treatment [16].
Osteonecrosis of the EAC is not an independent diagnosis in the International Classification of Diseases 10th revision (ICD-10) and the diagnosis is still not a well-known diagnosis among ear, nose and throat (ENT) specialists [15]. For this reason the condition may be mistaken and misdiagnosed for cholesteatoma, malignant external otitis or temporal bone malignancies [15]. We present a case with a patient diagnosed with bilateral osteonecrosis of the EAC after longterm treatment with BP for osteoporosis.
Case
76-year old female diagnosed with osteoporosis in 1999 (Figure 1). Previously, the patient had undergone bilateral mastectomy and local radiotherapy due to breast cancer (2001 and 2004), and received adjuvant therapy with antioestrogenes since 2001 (tamoxifen (2001-2004), anastrozole (2004-2009)). She had a family history of osteoporosis, was an active smoker (25 pack-years), drinking 2 units of alcohol per day and had hypertension (antihypertensive therapy from 1990’s). Since 2003 she has been using bilateral hearing aids due to age-related hearing loss. She had no history of ear disease or operation, no diabetes and never received chemotherapy. The patient took calcium and vitamin D supplements before she was diagnosed with osteoporosis. She had no secondary causes of osteoporosis at baseline visit 2007. The osteoporosis was initially treated by her general practitioner with oral BP (alendronate 10 mg/day, later switched to 70 mg/week).In 2007, the patient was referred to the hospital’s endocrinology outpatient clinic for optimizing osteoporosis treatment because of back pain. An X-ray of the spine showed multiple fractures of both thoracic and lumbar vertebrae and a Dual-energy X-ray Absorptiometry (DXA) showed a T-score of minus 3.5 standard deviations (SD) in the total hip; spine could not be evaluated. The patient was shifted to ibandronate (150 mg/month).
In 2008, a new DXA-scan showed an increase in total hip bone mass density (BMD) (T-score minus 3.1 SD). The patient continued treatment with ibandronate.
In 2010, a DXA scan was performed showing no improvement in total hip BMD compared to 2008. Consequently the patient was switched to treatment with IV zoledronic acid (5 mg/year) to ensure full compliance. The patient did not want denosumab and teriparatide was contra-indicated due to previous breast cancer.
In May 2013 (after the total of three years of zoledronic acid (total 15 mg), the patient presented with bilateral ear pain and was referred from an ENT practitioner to the ENT department, with the tentative diagnosis malignant external otitis. The otologic examination showed extensively exposed bone in the right EAC and a smaller area of exposed bone in the left EAC. Microbiological examination showed no growth of bacteria. A computed tomography (CT) scan showed pathology consistent with ostitis in both ear canals. The patient was diagnosed with bilateral osteonecrosis of the EAC, presumably on the basis of long-term BP treatment. She was treated conservatively with removal of debris followed by local and oral antibiotics (ciprofloxacin) for eight weeks. The treatment with BP was discontinued and the patient continued taking calcium and vitamin D. In October 2013, a DXA scan showed a T-score of minus 3.3 SD in the total hip. All DXA scans were performed on the same DXA machine.
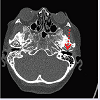
In November 2013, the patient was admitted to hospital with a right-sided peripheral facial paralysis. A new CT scan showed fluid in the right middle ear and bone destruction in the left EAC (Figure 2). Still, microbiological examination showed no growth of bacteria. The facial paralysis was presumed to be due to edema around the nerve. The patient was treated with IV antibiotics (cefuroxime) for six weeks, systemic glucocorticoids for 10 days (50 mg/day), and conservative debridement was performed. During treatment the patient’s facial paralysis was in remission, the otologic examination showed signs of healing in the EAC and the patient had no otorrhea.
In January 2014, the patient was treated surgically with bilateral removal of necrotic bone and reconstruction of the ear canal. Postoperatively, signs of healing were seen in both EACs, but still the patient suffered from bilateral ear pain. Unfortunately, no biopsy was taken for histological examination during treatment. Blood samples for analyzing bone turnover markers were not available, but since the patient had received three years of zoledronic acid suppressed levels of carboxy-terminal collagen crosslinks (CTX) and procollagen type I propeptides (PINP) are to be expected.
Discussion
We present a patient diagnosed with BP-associated bilateral osteonecrosis of the external auditory canal following treatment with BP for osteoporosis for 15 years. Initially the patient was diagnosedwith bilateral cholesteatoma, however, due to a history of long-term treatment with bisphosphonate and the clinical presentation with bilateral affection of the external auditory canal, it was concluded that these changes represented BP-associated osteonecrosis, in accordance with other case reports [9-13]. We have recently reported an increased incidence of cholesteatoma of the EAC associated with treatment with BP [16]. The same study found no cases of osteonecrosis of the EAC in either cases or controls. This indicates that osteonecrosis of the EAC is not an established diagnosis and patients may instead be diagnosed with cholesteatoma.Pathogenesis and manifestations of osteonecrosis of the EAC and ONJ may be similar despite their different anatomic location. The first report in 2003 on osteonecrosis in relation to BP therapy was on ONJ [6]. Since then several case reports have been published, but still the underlying pathology of ONJ is not well established. It has been hypothesized that a combination of micro-fractures, not healing, infection of closely advanced tissues and the anti-angiogenetic effect of BP [6] may eventually lead to osteonecrosis.
Risk factors for ONJ are IV BP, cancer and anti-cancer therapy, duration of treatment, glucocorticoids, alcohol/tobacco use and dental factors as dental disease, concomitant or past oral infection, maxillary or mandibular bone surgery, poor fitting dental appliances and intraoral trauma, poor oral hygiene, chronic inflammation, diabetes mellitus, ill-fitting dentures, as well as other drugs [6,8]. In defining ONJ it is stated that the patient should not have received radiotherapy to the craniofacial region [6]. In our case, the patient had had breast cancer and only received local radiotherapy therapy to the left hemithorax, but no glucocorticoids or chemotherapy. However, the patient did smoke cigarettes and had an intake of two units of alcohol a day. Studies have shown that both the duration of exposure to BP therapy and the type of BP are associated with development of ONJ [6]. In the existing case reports on BP-associated osteonecrosis of the EAC patients were BP-treated from 4 to 11 years.
According to the guidelines on ONJ from the American Society for Bone and Mineral Research (ASBMR), there are no published data indicating that discontinuation of BP therapy will promote resolution [6]. Therefore it is recommended by the ASBMR that the indication for giving BPs is considered before choosing to continue or discontinue BP therapy [6]. In the present case, treatment with BPs was discontinued and the patient is currently not receiving other treatment for her osteoporosis than calcium and vitamin D supplements despite a DXA scan still showing osteoporosis. Although the patient had multiple fractures of the spine before BP treatment, no new fractures appeared during BP treatment. Due to the patient’s medical history, including breast cancer twice and prior external radiotherapy involving the skeleton, anabolic therapy with teriparatide is contraindicated. Concerning ONJ earlier data have suggested enhanced osseous wound healing with teriparatide in those without contraindications for its use [8].
Our patient developed a peripheral facial paralysis, underwent several months of treatment with local, oral and IV antibiotics, underwent surgery and had numerous visits to the outpatient clinic and admissions to hospital, and is still suffering from chronic ear pain. This underlines the significant impact of the diagnosis and its complications on the patient’s quality of life. Therefore it is of great importance to be aware of this rare diagnosis so that appropriate actions can be taken and treatment begun to prevent severe complications. In the future, patients with several risk factors for developing external otitis should probably be otologically assessed before commencement of BP therapy.
Conclusion
BP-associated osteonecrosis of the external auditory canal is a rare condition and may well be misclassified. Thorough medical history including medication is important in these patients to establish a correct diagnosis. In BP treated patients even with vague otological symptoms, osteonecrosis must be considered and a cancer ruled out. Although BP-induced osteonecrosis is rare, the large volume of BP prescriptions makes the number of patients at risk significant. However we still think that the benefits of therapy with BPs in osteoporosis patients with high-fracture risk outweigh the risk of osteonecrosis of the external auditory canal.Acknowledgements
This case-report was funded by a research grant from Nordsjællands Hospital-Hillerød.References
- McClung M, Harris ST, Miller PD, Bauer DC, Davison KS, et al. (2013) Bisphosphonate therapy for osteoporosis: benefits, risks, and drug holiday. Am J Med 126: 13-20.
- Rizzoli R, Body JJ, Brandi ML, Cannata-Andia J, Chappard D, et al. (2013) Cancer-associated bone disease. Osteoporos Int 24: 2929-2953.
- Khosla S, Bilezikian JP, Dempster DW, Lewiecki EM, Miller PD, et al. (2012) Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab 97: 2272-2282.
- Orozco C, Maalouf NM (2012) Safety of bisphosphonates. Rheum Dis Clin North Am 38: 681-705.
- Reid IR (2013) Osteoporosis treatment: focus on safety. Eur J Intern Med 24: 691-697.
- Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, et al. (2007) Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 22: 1479-1491.
- Vestergaard P, Schwartz K, Rejnmark L, Mosekilde L, Pinholt EM (2012) Oral bisphosphonate use increases the risk for inflammatory jaw disease: a cohort study. J Oral Maxillofac Sur 70: 821-829.
- Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, et al. (2015) Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res 30: 3-23.
- Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, et al. (2010) Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 25: 2267-2294.
- Hammarfjord O, Stassen LF (2014) Bisphosphonate therapy and ankylosis of the temporomandibular joint: is there a relationship? A case report. Oral Surg Oral Med Oral Pathol Oral Radiol 118: e68-e70.
- Polizzotto MN, Cousins V, Schwarer AP (2006) Bisphosphonate-associated osteonecrosis of the auditory canal. Br J Haematol 132: 114.
- Froelich K, Radeloff A, Kohler C, Mlynski R, Müller J, et al. (2011) Bisphosphonate-induced osteonecrosis of the external ear canal: a retrospective study. Eur Arch Otorhinolaryngol 268: 1219-1225.
- Bast F, Fuss H, Schrom T (2012) Bilateral bisphosphonate-associated osteonecrosis of the external ear canal : a rare case. HNO 60: 1127-1129.
- Wickham N, Crawford A, Carney AS, Goss AN (2013) Bisphosphonate-associated osteonecrosis of the external auditory canal. J Laryngol Otol 127: S51-S53.
- Salzman R, Hoza J, Perina V, Starek I (2013) Osteonecrosis of the external auditory canal associated with oral bisphosphonate therapy: case report and literature review. Otol Neurotol 34: 209-213.
- Thorsteinsson AL, Vestergaard P, Eiken P (2014) External auditory canal and middle ear cholesteatoma and osteonecrosis in bisphosphonate-treated osteoporosis patients: a Danish national register-based cohort study and literature review. Osteoporos Int 25: 1937-1944.