Journal of Surgery
Validation of the ACS-NSQIP Liver Module: A Single-Center Experience
David A Daar, Aram N Demirjian and David K Imagawa*
- Division of Hepatobiliary & Pancreas Surgery, Department of Surgery, University of California, Irvine Medical Center, CA, USA
*Address for Correspondence: David K. Imagawa, MD, PhD, Division of Hepatobiliary & PancreasSurgery, Department of Surgery, University of California, Irvine MedicalCenter, 333 City Blvd West, Suite 1205, Orange, CA 92868, USA, Tel:714-456-3884; Fax: 714-456-3487; E-mail: dkimagaw@uci.edu
Citation: Daar DA, Demirjian AN, Imagawa DK. Validation of the ACS-NSQIP Liver Module: A Single-Center Experience. J Surgery. 2015; S(2): 8.
Copyright © 2015 Daar DA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Special Issue: 2
Submission: 10 September 2015 | Accepted: 14 October 2015 | Published: 19 October 2015
Editors:
Dr. Marlon A Guerrero, Assistant Professor of Surgery, University of Arizona, USA
Dr. James A Warneke, Associate Professor of Surgery, University of Arizona, USA
Abstract
Introduction: Large centralized databases are being increasingly utilized to assess surgical outcomes and determine reimbursement. The accuracy of liver resection data within the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) is assessed.
Methods: From August 2007 to May 2013, a retrospective review of liver resections captured by single-institution “standard” ACS-NSQIP data and a prospectively-maintained database was performed.
Results: Of the 93 liver resections captured by ACS-NSQIP, 12 were incorrectly classified (false positive rate, 12.9%). Of the 81 true liver resections reported (139 actually performed), ACS-NSQIP demonstrated high fidelity with the prospective database with respect to preoperative characteristics, median length of surgical stay (6 days, interquartile range: 4-7 days vs. 6 days, IQR: 4-7 days), and 30-daymortality (1.2% vs. 1.2%). The “standard” ACS-NSQIP underreported the overall complication rate (29.6% vs. 43.2%; P < 0.001) and failed to capture liver-specific complications including biliary leak, liver failure, pleural effusion, postoperative ascites, and small bowel obstruction (overall sensitivity, 68.6%).
Conclusions: Overall reporting of liver resection data within ACS-NSQIP is generally robust. While the ACS-NSQIP Procedure-Targetedprogram for liver resection instituted in 2012 would capture the majority of liver-specific complications, further refinement may improve the accuracy of this database.
Introduction
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) was first developed by the Department of Veterans Affairs (VA) in the early 1990s as a means of measuring the system’s overall quality of surgical care [1]. Today, ACS-NSQIP gathers data on over 150 clinical and surgical variables across over 550 institutions internationally [1,2].
ACS-NSQIP data has been used to improve general surgical care by means of reduced complications, mortality, and cost [3-5]. Surgical subspecialties, e.g., vascular and colorectal surgery, have also benefitted from the multi-institutional input ACS-NSQIP provides [6-8]. Recent studies have used ACS-NSQIP data to assess outcomes after hepatobiliary surgeries such as liver resection, including morbidity and mortality in the elderly [9]; surgical site infections and other postoperative complications [10-12]; as well as length of surgical stay [5].
Moreover, with the implementation of the Affordable Care Act (ACA) it is anticipated that public reporting of surgical outcomes may become increasingly linked to the Centers for Medicare and Medicaid Services (CMS) reimbursements [6,13,14]. A group of hospitals in ACS-NSQIP are already participating in this by voluntarily publicly reporting a small number of risk-adjusted outcomes [14], and for this reason the validity of ACS-NSQIP and other national databases should be assessed.
Along with its rigorous reviewer training process, ACS-NSQIP performs its own quality-assurance auditing [15]. Nevertheless, a few studies have shown concern over the ability of ACS-NSQIP to effectively assess outcomes regarding specific surgical procedures, namely within the field of hepatobiliary and pancreas surgery [10,16]. As an alternative to the “standard” database, in July 2011 a “Procedure-Targeted” option was implemented to address such issues [17]. Although hepatobiliary-specific modules, including that for liver resection, were implemented in July 2012, their procedurespecific outcomes data may be limited since many variables are not captured by ACS-NSQIP. The main objective of our study was to perform a retrospective review assessing the accuracy of liver resection data within the “standard” ACS-NSQIP database.
Methods
Patient population and data source
This study is a retrospective review, which relied on two databases: ACS-NSQIP and chart review. Chart review data was obtained from a prospectively maintained institutional database. This study was approved by the University of California, Irvine Institutional Review Board.
All adult patients who underwent elective or emergent liver resection for any diagnosis at our institution over a 5-and-a-half year period from August 2007 to May 2013 were included. Liver resectionwas determined using the following Current Procedure Terminology (CPT) codes: partial hepatectomy (47120), trisegmentectomy (47122), total left hepatectomy (47125), and total right hepatectomy (47130).
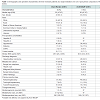
Preoperative variables were gathered from the medical record. Data included basic demographics, body mass index (BMI), and resence of comorbidities. Perioperative variables were gathered from surgery, anesthesia, and pathology reports, including operative time, tumor size and number of segments resected. Discharge diagnosis was identified using the appropriate diagnostic codes. To simplify the diagnosis variable we classified each diagnostic code into one of seven groups (Table 1).
The ACS-NSQIP was retrospectively reviewed for all reported cases of liver resection using the same CPT codes for single institution data. Direct comparison was then made with our institutional database.
Outcome definitions
Our primary outcomes included overall morbidity, length of surgical stay, and 30-day mortality rate. Overall complication rate was defined as a patient having at least one complication of ANY type within 30 days of operation. Although ACS-NSQIP tracks perioperative morbidity events and mortality that occur within 30 days of operation, the database did not begin gathering all-cause 30- day readmission until January 2011. Therefore, complete readmission data was only available in chart review data. We further stratified 30- day readmission to include only unplanned readmission related to the index case, as previously described [18].
Secondary outcomes reported were specific postoperative complications gathered by both ACS-NSQIP and our database, which included: superficial and deep incisional surgical site infection (SSI), organ space SSI, wound dehiscence, pneumonia, unplanned intubation, pulmonary embolism, greater than 48 hours of ventilatory assistance (failure to wean), progressive renal insufficiency, acute renal failure, urinary tract infection, stroke or cerebrovascular accident, coma of more than 24 hours, cardiac arrest, myocardial infarction, postoperative transfusion, deep vein thrombosis requiring treatment, sepsis, and septic shock. Superficial surgical site infections, deep surgical site infections, and wound disruptions were grouped together into one variable termed wound infection. Sepsis and septic shock were grouped together as a single sepsis variable [16].
The “standard” ACS-NSQIP database does not capture data on liver-specific complication variables. However, additional postoperative events captured by our institutional database and included in analysis of overall complication rate included biliary leak, liver failure, pleural effusion, postoperative ascites, and small bowel obstruction. Biliary leak was defined according to the International Study Group of Liver Surgery (ISGLS) guidelines as persistent drainage of bilious fluid (total bilirubin greater than three times serum bilirubin concentration) after postoperative day three [19]. However, our study included only those events requiring percutaneous drainage, ERCP stenting, or other surgical intervention. Post-hepatectomy liver failure was also defined according to ISGLS guidelines as an increasing INR and increasing serum bilirubin concentration on or after postoperative day five [20]. Pleural effusion was reported if responsible for hypoxemia and/or dyspnea requiring thoracentesis [21]. Postoperative ascites was defined as intraabdominal fluid requiring procedural intervention, e.g., paracentesis. Small bowel obstruction was only considered if requiring nasogastric decompression or surgical intervention.
Statistical analysis
Chart review was considered the gold standard [16,22]. The level of agreement between ACS-NSQIP and chart review with respect to demographic, preoperative comorbidity, and operative characteristics was assessed with percent agreement and Cohen’s kappa statistic [23], except difference in continuous variables (i.e., age, body mass index) were compared using the Wilcoxon signed rank sum test. With regards to outcomes, to measure agreement in postoperative complications, sensitivity and specificity were calculated for each individual variable as well as overall complication rate. In addition, McNemar’s test for correlated proportions was employed to assess difference in overall complication rate [24]. We compared differences in length of surgical stay and 30-day mortality with Wilcoxon signed rank sum test. All continuous variables are presented as the median and interquartile range (IQR).
When applicable, a significance level of 0.05 was used. Data analysis was performed using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY).
Results
Patient cases, demographics, and operative characteristics
Our prospectively maintained institutional database identified 139 liver resections, while query of the ACS-NSQIP database returned 93 liver resection patients at our institution. Among these 93 ACSNSQIP patients, 81 patients were identified as true liver resections when compared to chart review, and 12 patients were incorrectly classified (i.e., wedge biopsies, ablations, adrenal resection), giving a false positive rate of 12.9%. Further direct comparisons were made between the 81 patients correctly captured by ACS-NSQIP.
When examining demographic and operative characteristics, ACS-NSQIP demonstrated near complete agreement with the chart review, and there were no statistically significant differences in any variable. Demographic and operative characteristics of both ACSNSQIP data and chart review are illustrated in detail in Table 1.
Surgical outcomes
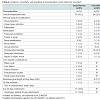
ACS-NSQIP accurately captured one death within 30 days of operation (30-day mortality, 1.2%). Median length of surgical stay did not differ between ACS-NSQIP and chart review (6 days, IQR: 4-7 days vs. 6 days, IQR: 4-7 days, respectively). There were 24 patients reported by ACS-NSQIP as having any complication (overall 30-day complication rate, 29.6%), compared with 35 patients in our chart review (overall 30-day complication rate, 43.2%). The 11 cases of patients with any complication who were not captured were due to the following: two organ space infections, two postoperative transfusions, one wound infection, and six liver-specific complications. The overall sensitivity of ACS-NSQIP for reporting patients with ANY complication was 68.6%, while the specificity was 100.0%. An exact McNemar’s test determined these overall complication rates to be significantly different (p < 0.001).
Postoperative transfusion was the most commonly reported complication in this patient group. Both chart review and ACSNSQIP captured 18 cases (22.2%). This variable was the most commonly misidentified. ACS-NSQIP falsely documented three cases while failing to capture three cases, giving ACS-NSQIP recognition of postoperative transfusion sensitivity and specificity of 83.3% and 95.2%, respectively. There were also inaccuracies in reporting wound infection and organ space infection. Seven cases of wound infection and five cases of organ space infection were identified by chart review. ACS-NSQIP failed to capture three cases of wound infection and two cases of organ space infection (sensitivity, 57.1% and 60.0%, respectively), while four cases of organ space infection were falsely reported (specificity, 94.7%). One case of renal failure was identified by chart review but was misclassified as renal insufficiency.
Thirty-day readmission was not introduced into the ACS-NSQIP database until 2011, thus the data for our study dates is incomplete. However, our prospectively maintained database monitored 30- day readmission, and we identified 15 readmissions (18.5%) during this period. Eleven (13.6%) readmissions were unplanned related readmissions, with causes including: three episodes each of wound infection (3.7%) and pleural effusion (3.7%); two episodes each of biliary leak (2.5%) and small bowel obstruction (2.5%); and one organ space infection (1.2%).
Liver-specific complications are not captured in the “standard” ACS-NSQIP database. However, our database identified a total of 18 liver-specific complications, including six cases of biliary leak (7.4%), four cases each of pleural effusion and liver failure (4.9%), three cases of small bowel obstruction (3.7%), and one case of postoperative ascites (1.2%). Of the liver failure events, two were ISGLS grade A, one was grade B, and one was grade C. The patient with grade C liver failure experienced multiple postoperative events and was the one case of mortality in this study group. One biliary leak was incorrectly captured by ACS-NSQIP as organ-space SSI.
A summary of postoperative complication incidence, sensitivity, and specificityis presented in Table 2.
Discussion
As ACS-NSQIP use continues to expand, its limitations must be determined and addressed. We examined, through a retrospective chart review, the accuracy of liver resection data within the “standard” ACS-NSQIP database. Our results demonstrate that overall reporting is generally robust, but this database lacks liver-specific postoperative complications. The new procedure-targeted program is a positive shift in direction for ACS-NSQIP but captures only a subset of these hepatobiliary-specific events. This underscores not only the value of the program but also the possible need for a more comprehensive module.
This study is, to our knowledge, the first to compare single institution ACS-NSQIP data to that of chart review in liver resection patients. In this analysis, we found an overall complication rate of 43.2% in chart review as opposed to 29.6% by ACS-NSQIP. Our singleinstitution ACS-NSQIP complication rate was relatively consistent with recent literature on liver resections, which report morbidity rates from 27% to 56% [25,26]. A recent meta-analysis showed among studies of liver resection that definitions of overall morbidity are inconsistent and often undefined in the literature [27]. Moreover, recent data suggests that complication rates are steadily increasing due to an increased willingness to perform liver resection on higher-risk patients, a greater percentage of patients with malignancy undergoing resection, and more complex operations [26,28]. Our findings suggest that with regard to liver resection, overall complication rate has most likely been underreported by the ACS-NSQIP database.
ACS-NSQIP performs regular audits of its clinical data abstractors and has demonstrated an inter-rater reliability within 1.56% overall [2]. Although overall morbidity showed 100% specificity, our results illustrate slight discrepancies in several postoperative variables as well as larger discrepancies in postoperative transfusion, wound infection, and organ-space SSI.
Issues with capturing postoperative transfusion have been cited previously [16,25]. Changes to the ACS-NSQIP definition of bleeding complications in 2010 may have contributed to the discordance in our study group. This variable includes but does not solely identify postoperative hemorrhage, which has been shown to be a risk factor for further postsurgical morbidity and has been linked to poor longterm outcomes in patients undergoing liver resection for malignancy [29-31]. Distinctions must be made with this variable in order to parse out the incidence of postoperative hemorrhage versus other reasons for postoperative transfusion captured by ACS-NSQIP.
Surgical site infection (SSI) significantly increases length of stay and rate of hospital readmission, thus increasing cost of care [12,32]. SSIs accounted for a clinically relevant 36.4% of unplanned related readmissions but demonstrated discordance in classification by ACS-NSQIP. Rates of SSI are being used to measure surgical quality [33]; a study of 2007 ACS-NSQIP colon resection data demonstrated that institutions needed to meet a threshold case volume of >94 to achieve an acceptable level of reliability [34]. With this in mind, the discordance for capturing SSI in our study may be attributable to our study size being below a threshold case level. Further research may indicate a different threshold for SSI data reliability for liver resection.
Regarding issues with incorrect classification of liver resection cases, our false positive rate of 12.9% more than likely reflects input error by the clinical data abstractor. Studies have shown administrative data collection to be less accurate [22,35], but both methods of review in our present study are performed by clinical reviewers and should make them comparable [16]. Suggestions for further improvement in ACS-NSQIP fidelity could be to develop more rigorous training modules for clinical nurse reviewers and enhanced communication with surgeons in their institution. At our institution we have begun reviewing all ACS-NSQIP reported complications in our Morbidity and Mortality committee prior to submission.
Through our comparison we can attribute the majority of our higher overall morbidity rate to the inclusion of liver-specific complications. The three most common liver-specific complications we encountered were biliary leak (7.4%), liver failure (4.9%),and pleural effusion (4.9%). Liver failure is considered the most important complication after liver resection and is often reported in institutional studies [10,26,27,36-39]. One of the four cases of liver failure was classified as grade C, and ultimately was the one case of 30-day mortality. Although one episode of biliary leak was captured by ACS-NSQIP as an organ-space SSI, the addition of a biliary leak variable further enhances distinctions within the dataset[10]. Incidence of biliary leak after liver resection has been shown to range between 3% and 12% [26,37,39,40] and is increased with the greater the complexity of resection [38]. Further diagnostic testing and intervention required often delay abdominal drain removal and hospital discharge, making it an especially long-term issue for patients having undergone resection for malignant disease [19,41-43].
Pleural effusion is not captured by ACS-NSQIP, nor has it been included in the procedure-targeted option for liver resection. A multivariate analysis of 555 liver resection patients showed a pleural effusion rate of 4.7% requiring non-pharmacological intervention, citing independent risk factors such as right hepatectomy andprolonged surgery time [21]. In addition, early small bowel obstruction is related to any major open abdominal surgery, with conservative reports of incidence ranging between 0.7% to 9.5% within 30 days of operation [44]. Reoperation is required in up to 3% of patients [45]. Chart review captured three cases of small bowel obstruction requiring non-pharmacological intervention, two of which were the cause of readmission, which indicates its more severe impact on patient outcomes as well as hospital costs. Our chart review captured a single case of postoperative ascites, a notable liverspecific complication [37,46], which plays a role in heralding possible underlying portal vein thrombosis [47]. Our study results suggest that it may be useful to include pleural effusion, small bowel obstruction, and postoperative ascites in ACS-NSQIP postoperative variables for liver resection.
Readmission is a complicated and not infrequent event in hepatobiliary patients, and ACS-NSQIP instituted this variable in data collection in 2011 [2,22,25,48]. Sellers et al. demonstrated that among surgical sub-specialties in the ACS-NSQIP database, the highest readmission rate was reported for hepatobiliary surgeries (16.7%) [22]. A recent study at a major academic center observed 18.7% of liver resection patients required hospital readmission [49]. Our all-cause readmission rate (18.5%) is consistent with the literature, although we could not directly compare our data to ACS-NSQIP for this study cohort. Moreover, we observed an unplanned related readmission rate of 13.6%, which is similar to 2011 national data in ACS-NSQIP for liver resection (10.5%) [18]. Major postoperative complications play a key role in early rehospitalization [48,50]. Interestingly, in our study population liver-specific complications caused the majority (63.6%) of unplanned related readmissions. In addition to biliary leak, which is already captured in the procedure-targeted module of ACSNSQIP, pleural effusion and small bowel obstruction contributed to five readmissions (45.5%), further underscoring the need for a more comprehensive inclusion of hepatobiliary-specific postoperative variables.
ACS-NSQIP has recognized that different operations can have specific risks and unique outcomes, and in July 2011 the first phase of a “Procedure-Targeted” program was implemented to address this issue [1,17]. In addition to capturing “standard” variables, procedurespecific variables were included for 34 high-risk, high-volume procedures. A procedure-targeted module for liver resection was initiated in July 2012, based on an earlier proposal by Pitt et al. [36]. The model includes several additional preoperative and intraoperative variables, as well as two liver-specific outcomes variables, posthepatectomy liver failure and biliary leak.
We believe this procedure-targeted program is a step in the right direction, but its scope may still be limited. Our study validates the merits of this program and suggests the adoption of additional of liver-specific complications may be warranted. Although liverfailure and biliary leak are the two most common events, the addition of postoperative variables such as pleural effusion, small bowel obstruction, and ascites will further enhance distinctions of postoperative liver resection data within ACS-NSQIP. Previous studies using ACS-NSQIP data to assess liver resection outcomes lack these liver-specific variables [9,12], but their addition may provide a more accurate estimate of how complicated the postoperative course after liver resection truly is. In addition, with a comprehensive group of outcomes for liver resection ACS-NSQIP can set a standard for the definition of overall morbidity, synchronizing further research on this procedure.
This study does have limitations. First, the sample size of our study is small due to utilizing single-institution data allowing small outcome rates to be more easily subjected to minor instances of missing or incorrectly captured data. Second, this study was performed at a highvolume academic medical center in which the ICD-9 coding may be muddled by the complexity of patient cases and therefore possibly less applicable to community institutions.
In conclusion, the use of large, multi-institutional databases such as ACS-NSQIP is crucial to assessing surgical outcomes and as a means of determining reimbursement. Accuracy both overall and within surgical subspecialties must be maintained, especiallyfor complex hepatobiliary patients. We compared chart review of a prospectively maintained database to single-institution ACSNSQIP data and observed that overall reporting of liver resection data within ACS-NSQIP is generally robust. While recent efforts to improve HPB procedure-specific tracking within ACS-NSQIP are underway, the database may benefit from further refinement with a more comprehensive set of liver-specific postoperative complication variables.
Acknowledgements
Michael Phelan, PhD contributed assistance with statistical analysis.
References
- (2014) ACS-NSQIP: program specifics.
- ACS-NSQIP Pediatric (2013) User Guide for the 2012 ACS NSQIP pediatric: Participant use data file. American College of Surgeons-National Surgical Quality Improvement Program, Chicago, IL.
- Khuri SF, Daley J, Henderson W, Hur K, Demakis J, et al. (1998) The Department of Veterans Affairs' NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228: 491-507.
- Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, et al. (2009) Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg 250: 363-376.
- Gedaly R, McHugh PP, Johnston TD, Jeon H, Ranjan D, et al. (2009) Obesity, diabetes, and smoking are important determinants of resource utilization in liver resection: a multicenter analysis of 1029 patients. Ann Surg 249: 414-419.
- Cima RR, Lackore KA, Nehring SA, Cassivi SD, Donohue JH, et al. (2011) How best to measure surgical quality? Comparison of the Agency for Healthcare Research and Quality Patient Safety Indicators (AHRQ-PSI) and the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) postoperative adverse events at a single institution. Surgery 150: 943-949.
- Cima R, Dankbar E, Lovely J, Pendlimari R, Aronhalt K, et al. (2013) Colorectal surgery surgical site infection reduction program: a national surgical quality improvement program--driven multidisciplinary single-institution experience. J Am Coll Surg 216: 23-33.
- Enomoto LM, Hill DC, Dillon PW, Han DC, Hollenbeak CS (2014) Surgical specialty and outcomes for carotid endarterectomy: evidence from the National Surgical Quality Improvement Program. J Surg Res 188: 339-348.
- de la Fuente SG, Bennett KM, Scarborough JE (2013) Functional status determines postoperative outcomes in elderly patients undergoing hepatic resections. J Surg Oncol 107: 865-870.
- Aloia TA, Fahy BN, Fischer CP, Jones SL, Duchini A, et al. (2009) Predicting poor outcome following hepatectomy: analysis of 2313 hepatectomies in the NSQIP database. HPB (Oxford) 11: 510-515.
- Li GZ, Speicher PJ, Lidsky ME, Darrabie MD, Scarborough JE, et al. (2014) Hepatic resection for hepatocellular carcinoma: do contemporary morbidity and mortality rates demand a transition to ablation as first-line treatment? J Am Coll Surg 218: 827-834.
- Moreno Elola-Olaso A, Davenport DL, Hundley JC, Daily MF, Gedaly R (2012) Predictors of surgical site infection after liver resection: a multicenter analysis using National Surgical Quality Improvement Program data. HPB (Oxford) 14: 136-141.
- (2010) 111th congress (2009-2010). The Patient Protection and Affordable Care Act.
- Dahlke AR, Chung JW, Holl JL, Ko CY, Rajaram R, et al. (2014) Evaluation of initial participation in public reporting of American College of Surgeons NSQIP surgical outcomes on Medicare's Hospital Compare website. J Am Coll Surg 218: 374-380.
- Shiloach M, Frencher SK Jr, Steeger JE, Rowell KS, Bartzokis K, et al. (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210: 6-16.
- Epelboym I, Gawlas I, Lee JA, Schrope B, Chabot JA, et al. (2014) Limitations of ACS-NSQIP in reporting complications for patients undergoing pancreatectomy: underscoring the need for a pancreas-specific module. World J Surg 38: 1461-1467.
- Cohen ME, Ko CY, Bilimoria KY, Zhou L, Huffman K, et al. (2013) Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical focus. J Am Coll Surg 217: 336-346.e1.
- Kim S, Maynard EC, Shah MB, Daily MF, Tzeng CW, et al. (2015) Risk factors for 30-day readmissions after hepatectomy: analysis of 2444 patients from the ACS-NSQIP database. J Gastrointest Surg 19: 266-271.
- Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, et al. (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149: 680-688.
- Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, et al. (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149: 713-724.
- Nobili C, Marzano E, Oussoultzoglou E, Rosso E, Addeo P, et al. (2012) Multivariate analysis of risk factors for pulmonary complications after hepatic resection. Ann Surg 255: 540-550.
- Sellers MM, Merkow RP, Halverson A, Hinami K, Kelz RR, et al. (2013) Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 216: 420-427.
- Fleiss JL, Cohen J (1973) The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas 33: 613-619.
- McNemar Q (1947) Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 12: 153-157.
- Lucas DJ, Pawlik TM (2014) Quality improvement in gastrointestinal surgical oncology with American College of Surgeons National Surgical Quality Improvement Program. Surgery 155: 593-601.
- Dokmak S, Ftériche FS, Borscheid R, Cauchy F, Farges O, et al. (2013) 2012 Liver resections in the 21st century: we are far from zero mortality. HPB (Oxford) 15: 908-915.
- LimC, Dejong CH, Farges O; e-HPBchir Study Group from the Association de Chirurgie Hépato-Biliaire et de Transplantation (ACHBT) (Association of Hepatobilary and Transplant Surgery) (2014) Improving the quality of liver resection: a systematic review and critical analysis of the available prognostic models. HPB (Oxford) 17: 209-221.
- Cescon M, Vetrone G, Grazi GL, Ramacciato G, Ercolani G, et al. (2009) Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg 249: 995-1002.
- Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, et al. (2011) Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford) 13: 528-535.
- Kooby DA, Stockman J, Ben-Porat L, Gonen M, Jarnagin WR, et al. (2003) Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases. Ann Surg 237: 860-869.
- Yamamoto J, Kosuge T, Takayama T, Shimada K, Yamasaki S, et al. (1994) Perioperative blood transfusion promotes recurrence of hepatocellular carcinoma after hepatectomy. Surgery 115: 303-309.
- Ceppa EP, Pitt HA, House MG, Kilbane EM, Nakeeb A, et al. (2013) Reducing surgical site infections in hepatopancreatobiliary surgery. HPB (Oxford) 15: 384-391.
- de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, et al. (2009) Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 37: 387-397.
- Kao LS, Ghaferi AA, Ko CY, Dimick JB (2011) Reliability of superficial surgical site infections as a hospital quality measure. J Am Coll Surg 213: 231-235.
- Bensley RP, Yoshida S, Lo RC, Fokkema M, Hamdan AD, et al. (2013) Accuracy of administrative data versus clinical data to evaluate carotid endarterectomy and carotid stenting. J Vasc Surg 58: 412-419.
- Pitt HA, Kilbane M, Strasberg SM, Pawlik TM, Dixon E, et al. (2009) ACS-NSQIP has the potential to create an HPB-NSQIP option. HPB (Oxford) 11: 405-413.
- Mathur AK, Ghaferi AA, Sell K, Sonnenday CJ, Englesbe MJ, et al. (2010) Influence of body mass index on complications and oncologic outcomes following hepatectomy for malignancy. J Gastrointest Surg 14: 849-857.
- Zimmitti G, Roses RE, Andreou A, Shindoh J, Curley SA, et al. (2013) Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. J Gastrointest Surg 17: 57-64.
- Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA (2015) Laparoscopic versus open liver resection for metastatic colorectal cancer: a meta-analysis of 610 patients. Surgery 157: 211-222.
- Erdogan D, Busch OR, van Delden OM, Rauws EA, Gouma DJ, et al. (2008) Incidence and management of bile leakage after partial liver resection. Dig Surg 25: 60-66.
- Reed DN Jr, Vitale GC, Wrightson WR, Edwards M, McMasters K (2003) Decreasing mortality of bile leaks after elective hepatic surgery. Am J Surg 185: 316-318.
- Chok KS, Ng KK, Poon RT, Lo CM, Fan ST (2009) Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg 96: 81-87.
- Farid SG, Aldouri A, Morris-Stiff G, Khan AZ, Toogood GJ, et al. (2010) Correlation between postoperative infective complications and long-term outcomes after hepatic resection for colorectal liver metastasis. Ann Surg 251: 91-100.
- Sajja SB, Schein M (2004) Early postoperative small bowel obstruction. Br J Surg 91: 683-691.
- Beck DE, Opelka FG, Bailey HR, Rauh SM, Pashos CL (1999) Incidence of small-bowel obstruction and adhesiolysis after open colorectal and general surgery. Dis Colon Rectum 42: 241-248.
- Dagher I, Belli G, Fantini C, Laurent A, Tayar C, et al. (2010) Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg 211: 16-23.
- Chan KM, Lee CF, Wu TJ, Chou HS, Yu MC, et al. (2012) Adverse outcomes in patients with postoperative ascites after liver resection for hepatocellular carcinoma. World J Surg 36: 392-400.
- Glance LG, Kellerman AL, Osler TM, Li Y, Mukamel DB, et al. (2014) Hospital readmission after non-cardiac surgery: the role of major complications. JAMA Surg 149: 439-445.
- Kimbrough CW, Agle SC, Scoggins CR, Martin RC, Marvin MR, et al. (2014) Factors predictive of readmission after hepatic resection for hepatocellular carcinoma. Surgery 156: 1039-1048.
- Schneider EB, Hyder O, Wolfgang CL, Hirose K, Choti MA, et al. (2012) Patient readmission and mortality after surgery for hepato-pancreato-biliary malignancies. J Am Coll Surg 215: 607-615.