International Journal of Otorhinolaryngology
Download PDF
Review Article
The Indications, Timing,and Surgical Techniques for Performing Elective lingual and Labial Frenulectomies for Infants and Children
John E. Nathan*
- APT Research Foundation, Pune, India
*Address for Correspondence: John E. Nathan, Department of Otolaryngology, Northwestern University Feinberg, USA; E-mail: jnathandds@gmail.com
Citation: Nathan JE. The Indications, Timing, and Surgical Techniques for Performing Elective lingual and Labial Frenulectomies for Infants and Children. Inter J Otorhinolaryngology. 2017;4(1): 3.
International Journal ofOtorhinolaryngology | ISSN: 2380-0569 | Volume: 4, Issue: 1
Submission: 23 May, 2017| Accepted: 30 June, 2017 | Published: 03 July, 2017
Submission: 23 May, 2017| Accepted: 30 June, 2017 | Published: 03 July, 2017
Abstract
This article discusses the significance of anatomical variations of Maxillary and Mandibular frenula found in children, indications for surgical intervention vs deferment and no treatment, and the anesthetic and surgical techniques in contemporary use for their management. Ankyloglossia, or tongue-tie is a common phenomenon observed as early as birth which can become problematic for infants experiencing feeding difficulties when breast or bottle feeding. Secondarily, it has potential to impact on later speech developmentand the ability to verbalize certain sounds. While some children can overcome the anatomical defect, others require surgical intervention to free the anterior third of the tongue. Depending on the severity of the defect and anterior and superior nature of the attachment to the anterior alveolar ridge, ankyloglossia has potential to adversely affect periodontal health associated with lower incisors, both primary and permanent. The article describes various indications and variability of surgical approach for a given circumstance. Maxillary frenulums are probably the least understood and pose the most confusion for clinicians in the determination of actual need and timing for surgical intervention.
Keywords
Frenectomy; Indications; Surgical techniques
Introduction
Surgical management of lingual and labial frenula on infants and children in general falls under the category of elective procedures. These are performed on a daily basis by pediatric dental specialists, oral and maxillofacial surgeons, otolaryngologists, and on limited occasions for infants manifesting difficulty breast and bottle feeding by pediatricians lacking a referral option[1].
In the anterior maxillary dental arch, diastema (with excessive spacing) between maxillary primary and/or permanent central incisors created by virtue of an in growth of redundant fibrous gingival tissue preventing optimal eruption and positioning draws attention to a potential need for surgical intervention. Pediatric dental specialists are likely to be the best source with regard to timing decisions [1].
Definitive guidelines defining the relative indications and criteria for surgical intervention are essentially broad if not obscure, but in large part are followed or disregarded because the surgical procedures are simplistic and practitioner judgment-dependent [2]. Despite such, rationale and justification are somewhat elusive for some clinicians. For some, discretion is not made between those who are in virtual need of surgical management of excess frenulum tissue, rather the opportunity to treat by virtue of relative busyness or justification of the cost for laser instrumentation and/or hospitalization (for general anesthesia).
The intent of this paper is to provide clarification of the basis, timing, and techniques for addressing these soft tissue intra-oral anomalies. The need for maxillary anterior denture base frenulectomies in the presence of diastema is relatively rare and should in almost all cases be deferred until early adolescence following both natural and orthodontic closure of the diastema, in comparison to lingual ankyloglossia (tongue-tie) which has potential to impair nursing for the newborn. Specific indications and contraindications will be explored below in detail. A difference in opinion amongst clinicians clearly exists with respect to need and timing for intervention. This paper will explore options, benefits, and limitations of early or premature surgical management.
Motivation for this article arose from several surgical calendar days noted at institutions this author is affiliated. Multiple children appeared on the surgical schedule for the purpose of frenectomy or frenulectomy. Having cases of my own on the day attracted and permitted curiosity to oversee the specifics of the cases and techniques employed at this teaching institution by two otolaryngologists. Of twelve children on three days, scheduled frenectomies of both maxillary and mandibular anterior segments, essentially considered routine and an appropriate use of operating room time, personnel, and expense, it became somewhat clear that for only two of the children, ages, 18 months to 9 years of age, that selection criteria was appropriate for the anatomical abnormality and the planned surgical intervention. Five of the children under 2 years of age were subjected to general anesthetics where diagnoses included minimal ankyloglossia with minimal to no significant history of nursing or bottle feeding impairment. Four cases involved ablation of maxillary frenum for children less than 6 years with moderate 2 and 3 mm diastema. Elective decisions to treat at this juncture could at best be described as highly premature.
Subjecting children under these conditions to general anesthesia for these procedures is at the least ill-conceived. Two children, one 2 months of age presented with severe, broad-banded ankyloglossia and, the other 4.5 years, exhibited severe speech impairment described below after having undergone 2 years in speech therapy without notable success.
Indications for frenectomies
Ankyloglossia (Tongue-tie) where breast or bottle feeding is significantly impaired to the extent that the infant is unable to sufficiently latch on to the nipple (or bottle nipple) to suckle to empty the breast or bottle long before exhaustion. Adequate nourishment serves as the key guide in determining the degree to which suckling is or is not impaired. Parental frustration and difficulty in suckling due to anterior lingual frenulum attachment eventually comes to the attention of the pediatrician and/or lactation consultant for evaluation by a pediatric dental specialist for surgical consultation [3-5].
Constraints on suckling can result from anterior tissue attachment that can range from very thin fascial connective tissue (frequently treated with simple surgical scissor excision) to broad, thickened banded connective tissue necessitating more invasive surgical dissection for tissue management and hemostasis by scalpel or soft tissue laser. The extent of the dissection necessary and degree of cooperation required to safely perform the procedure generally determine the modality (topical and local anesthetic infiltration, by sedation, or general anesthetic) [4-6].
Adverse effect on speech
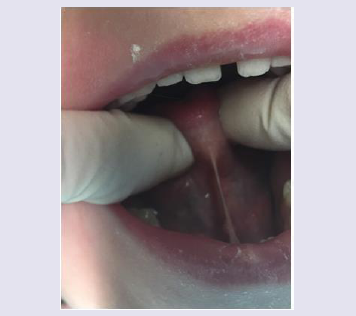
Speech development varies significantly among young children. The ability to generate certain sounds, i.e. “th” “ph”, “l”, generally require anterior and superior elevation of the anterior third of the tongue to the palatal side of the maxillary anterior incisors. Those with mild or heavy frenulum constraints can experience variable success in accomplishing tongue extension to enunciate these sounds (Figure 1).
While some children simply are able to adapt and overcome anatomical limitations, others have no success in doing so until surgical intervention is undertaken.
From this observers experience over 40 years, it is not uncommon to encounter a history which includes the child has been followed by a speech therapist without dental or intraoral anatomical assessment of possible etiologic cause. For some, two or more years of unproductive speech therapy, including the one case described above, occurswithout viable improvement reported.
Ascertaining the point at which maturation in speech development can alone compensate for a speech impediment, with or without anatomic cause, is not easily determined. Alternatively, surgical resection of the excessive gingival frenum alone, may not generally produce universal termination of the of the speech defect until corrective tongue re-positioning, through speech therapy, has a chance to occur.
Pathological retraction of lingual marginal gingival on the lingual side of lower incisors
This, while even rarer, can contribute to creation of a periodontal defect with gingival Recession beginning around age 6 years when the lower permanent incisors emerge. Allowed to persist, both soft tissue recession and bony defects have potential to compromise retention ofthe lower incisors.
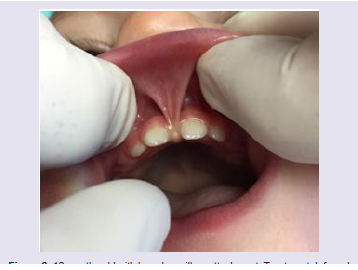
Perpetual diastema of maxillary primary and/or permanent central incisors due to a broad band of connective tissue embedded into palatal and labial aspects of the incisors originating from the inner aspect of the upper lip extending to the gingival borders of the incisors, palatal incisive papilla, and nasopalatine for men. Clinicians should be reminded of the normal anatomical changes that occurwith growth in the anterior maxilla which serves as further rationale to delay surgical management of the frenulum. With aging from 6-11 years, superior migration of the frenulum frequently occurs reducing the need or severity for surgical reduction of the fibrous connection. Secondly, as exfoliation of the primary canines occurs, eruption of the permanent maxillary canines self-contributes to significant or partial diastema closure of the incisor segment. These two naturally occurring events determine optimal timing for surgical intervention in combination with orthodontic management (Figure 2).
Figure 2: 12 months old with broad maxillary attachment. Treatment deferred until objective assessment of adverse effect speech is evident; or diastema results between permanent central incisors.
Lastly, because of the anterior prominence of this soft tissue attachment into the intraoral body of the upper lip, it is not at all uncommon for children in this age group to have at one time or another fallen or experienced traumatic injury which self-inflicts tearing of the frenulum, later minimizing or eliminating need for surgical modification-timely, yet traumatic.
Timing: The traditional recommendation has been to defer surgical excision of the maxillary anterior frenulum until after eruption of the permanent canines (age 11) or orthodontic closure of the diastema has been performed.
Surgical Techniques
If performed under local anesthesia, with or without sedation, bilateral lingual block administration of local is considered the method of choice. Lingual block anesthesia provides easiest access and visibility to permit optimal and precise visualization of the borders where anterior to posterior dissection is accomplished. Obviously, where general anesthetic is utilized, local anesthetic can beavoided. Even when general anesthetic is chosen, from a perspective of post-operative patient comfort, the lingual block anesthesia may be desirable. Post-operative tongue biting does not become a problem with infants until anterior teeth have erupted.
An alternate approach utilized by some surgeons over lingual nerve block, is to inject directly into the ventral surface of the tongue lateral to the frenulum. While this approach may be expedient and will serve to achieve sufficient paresthesia, it causes edema and bloating of the floor of the mouth which can obscure optimal visualization of the borders where incision and resection is made to permit optimal anterior to posterior extension of the surgical correction. Poorvisualization is likely to be the cause of inadequate extension of the surgical wound and result in subsequent need for revision.
Following induction of anesthesia, a single 3-0 silk suture is placed through the anterior tip of the tongue to literally provide the surgeon the ability to elevate and retract at will the anterior half of thetongue as needed for clipping/incision of the frenulum.
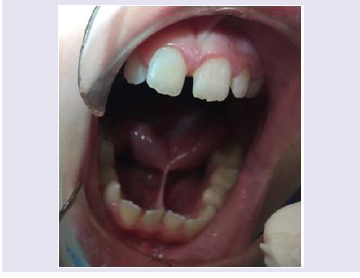
The intent of the surgical technique is to effectively sever the binding attachment of gingival mucosa from the base of the tongue to its anterior most attachment near the mucosal ridge in the lower jaw providing maximum mobility of the anterior third of the tongue. Thismay be accomplished via scalpel, electrosurgical cautery, or soft tissue laser. The latter offers simultaneous cutting and cautery minimizing hemorrhage and need for wound closure. Some surgeons prefer more precise dissection via scalpel. This method depending on the width of the fibrous and connective tissue band leaves an elliptical open wound in the floor of the mouth necessitating 2-4 interrupted 5-0 chromic or resorbable suture closures (Figure 3).
Figure 3: Lingual Ankyloglossia with retraction of lower lingual gingiva causing mal-position of central incisors and potential periodontal defect.
For patients 10 years and older needing surgical removal of the maxillary frenulum, any of the techniques are acceptable. Most surgeons probably choose soft tissue laser (vs. scalpel) because of anticipated bleeding as greater dissection is usually required to sever all connective tissue distal to the site of insertion of the frenulum between affected incisors. Local anesthetic infiltration to anesthetize the upper lip and alveolar mucosa is usually sufficient and hemostasis is facilitated by inclusion of a 1:100,000 epinephrine vasoconstrictor. Rarely is general anesthesia needed for this procedure. Alternatively, some surgeons prefer scalpel and local dissection with suture closureto gross obliteration of frenulum and connective tissue.
References
- Kupietzky A, Botzer E (2005) Ankyloglossia in the infant and young child: clinical suggestions for diagnosis and management. Pediatry Dent 27: 40-46.
- Wallace H, Clarke S (2006) Tongue tie division in infants with breast feeding difficulties. Int J Pediatr Otorhinolaryngol 70: 1257-1261.
- Ostapiuk B (2006) Tongue mobility in Ankyloglossia with regard to articulation. Ann Acad Med Stetin 52 Suppl: 37-47.
- Kloctiars T, Pitkaranta A (2009) Pediatric tongue-tie division: indications, techniques and patient satisfaction. Int J Pediatr Otorhinolaryngol 73: 1399-1401.
- Dollberg S, Botzer E (2011) Neonatal tongue-tie: myths and science. Harufuah 150: 46-49.
- Kumar M, Kalke E (2012) Tongue-tie, breastfeeding difficulties and the role of Frenotomy. Acta Peadiatr 101: 687-689.