Journal of Orthopedics & Rheumatology
Download PDF
Research Article
*Address for Correspondence: Charla R. Fischer, MD, Department of Orthopedic Surgery, The Spine Hospital, Columbia University Medical Center, New York, USA, E-mail: cdr2112@columbia.edu
Citation: Fischer CR, Hanson G, Eller M, Lehman RA. A Systematic Review of Treatment Strategies for Lumbar Spine Fusion Surgery in OsteoporoticPatients. J Orthopedics Rheumatol. 2016; 3(1): 9.
Copyright © 2016 Fischer CR, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 3, Issue: 1
Submission: 30 May, 2016 | Accepted: 18 June, 2016| Published: 23 June, 2016
Keywords: Lumbar fusion; Osteoporosis
The relevant information from each study was extracted and input into tabular form. The following information was collected: patient population including sample size, pre-operative measurement techniques of bone density, medical intervention type, dosage information, duration of treatment, and surgical technique used. The definition and adequate assessment of fusion being utilized in this study is based on the guideline update by Choudhri et al. in 2014 [6]. In order to be included, the study had to include fusion rate and the method used to assess successful fusion. In some studies, the pedicle screw loosening rate was stated and identified as a radiographic sign of nonunion. The information regarding the methodology of assessment for the perceived successful fusion was also recorded when available. The methodologies of fusion assessment include the following: radiography imaging, CT imaging (2D and 3D), the imaging study reader/s, any blinding information available, and the technical components to assess radiologic evidence of spine fusion. In several studies, more than one treatment group was used to evaluate the effects of multiple medications on fusion rates, in these cases; each medication group is listed separately. When included in the article, the statistical significance of the findings was collected and included in the table.
A Systematic Review of Treatment Strategies for Lumbar Spine Fusion Surgery in Osteoporotic Patients
Charla R. Fischer1*, Gregory Hanson2, Melinda Eller3 and Ronald A. Lehman1
- 1Department of Orthopedic Surgery, The Spine Hospital, Columbia University Medical Center, New York, USA
- 2Geisel School of Medicine, Dartmouth Hitchcock Medical Center, New Hampshire, USA
- 3Mailman School of Public Health, Columbia University Medical Center, New York, USA
*Address for Correspondence: Charla R. Fischer, MD, Department of Orthopedic Surgery, The Spine Hospital, Columbia University Medical Center, New York, USA, E-mail: cdr2112@columbia.edu
Citation: Fischer CR, Hanson G, Eller M, Lehman RA. A Systematic Review of Treatment Strategies for Lumbar Spine Fusion Surgery in OsteoporoticPatients. J Orthopedics Rheumatol. 2016; 3(1): 9.
Copyright © 2016 Fischer CR, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 3, Issue: 1
Submission: 30 May, 2016 | Accepted: 18 June, 2016| Published: 23 June, 2016
Abstract
Purpose: Evaluate the current evidence in the literature on treatment strategies for lumbar spine fusion in patients with osteoporosis.Methods: A systematic review of the literature from 1950-2015.Results: The review of the literature yielded 15 studies on the effect of treatment options for osteoporosis on lumbar fusion rates. One study demonstrated an association between low bone mass as measured by Hounsfield Units and lower fusion rates. Six studies evaluated perioperative medical treatment of osteoporosis and showed higher fusion rates in patients treated with alendronate and teriparatide. The strongest evidence was for perioperative teriparatide. Eight studies evaluated surgical treatment strategies in osteoporosis patients and showed that cement augmentation of pedicle screws and expandable pedicle screws demonstrated improved fusion rates over traditional pedicle screws. The strongest evidence was for expandable pedicle screws.
Conclusion: There are 15 articles evaluating osteoporosis in lumbar fusion patients and the highest level of evidence is for perioperative use of teriparatide.
Keywords: Lumbar fusion; Osteoporosis
Introduction
Osteoporosis is an issue facing spine surgeons with increasing importance [1]. In patients over 50 years old, 50% of women and 15% of men have osteoporosis [2]. Some authors have reviewed the rates of osteopenia and osteoporosis amongst patients undergoing spine surgery. Chin et al. found 46.1% of male patients and 41.4% of female patients with osteopenia, and 14% of male patients and 51.3% of female patients with osteoporosis amongst their spine patients [2].With such high rates of patients with osteopenia or osteoporosis undergoing spine surgery, it is important to review treatment strategies for these patients. The study by Anderson et al. in 2013 found a higher rate of low bone mass in patients with degenerative spondylolisthesis than spinal stenosis [3]. These patients had higher pain scores at one year after surgery. This highlights the importance of the treatment of osteoporosis before surgery to improve postoperative outcomes.
The metabolic dysfunction in osteoporosis is of concern to spine surgeons in regards to instrumentation and fusion. Conventional pedicle screws can only obtain as strong a fixation as the bone it is placed into. Pseudarthrosis is a common complication with lumbar fusion and can related to the patient’s quality of bone [4,5]. Thus, it is important to review the pre-operative and intra-operative treatment strategies for patients undergoing spinal fusion with osteoporosis to see if there are ways to augment the bone and prevent higher rates of nonunion and post-operative pain.
Methods
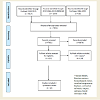
A comprehensive search of the literature was performed to identify articles that evaluated the effects on clinical outcomes from preoperative measurements of osteoporosis, pre and/or post-operative medications, and surgical interventions on lumbar spine fusion rates in low bone density patients. An electronic search of PubMed (MEDLINE), Ovid MEDLINE, and Cochrane was conducted using the following search terms: ((osteoporosis AND spine) AND (fusion or surgery or instrumentation) AND (bone density AND spine) AND (fusion or surgery or instrumentation)). The search yielded 7001 original articles and a reviewer screened all titles and abstracts for inclusion.During the screening process, any articles meeting the following criteria were excluded from the review: (1) animal studies, (2) literature reviews, (3) biomechanical studies, (4) vertebral compression fractures studies, (5) cervical or deformity surgery studies, (6) nonclinical outcomes studies. The search exclusion strategy yielded 110articles from the screened literature. Further screening of the titles and abstracts of the studies produced 15 articles included in the review, as shown in Figure 1. Studies with Level III or higher levels of evidence were excluded to provide the highest quality evidence based medicine review of the literature that can possible guide treatment.
The relevant information from each study was extracted and input into tabular form. The following information was collected: patient population including sample size, pre-operative measurement techniques of bone density, medical intervention type, dosage information, duration of treatment, and surgical technique used. The definition and adequate assessment of fusion being utilized in this study is based on the guideline update by Choudhri et al. in 2014 [6]. In order to be included, the study had to include fusion rate and the method used to assess successful fusion. In some studies, the pedicle screw loosening rate was stated and identified as a radiographic sign of nonunion. The information regarding the methodology of assessment for the perceived successful fusion was also recorded when available. The methodologies of fusion assessment include the following: radiography imaging, CT imaging (2D and 3D), the imaging study reader/s, any blinding information available, and the technical components to assess radiologic evidence of spine fusion. In several studies, more than one treatment group was used to evaluate the effects of multiple medications on fusion rates, in these cases; each medication group is listed separately. When included in the article, the statistical significance of the findings was collected and included in the table.
Results
The search guidelines above yielded 15 articles that met the inclusion criteria. All of these studies evaluated the various effects of osteoporosis on patients undergoing lumbar spinal fusion surgery. Pre-clinical animal model studies, biomechanical studies, vertebral compression fracture studies, and non-lumbar spine studies were not included. There was one study assessing the effect of different preoperative measure bone density on fusion rates, shown in Table 1. There were 6 studies evaluating the effect of the medical management of osteoporosis on lumbar fusions, shown in Table 2. There were 8 studies on the effect of alternative fixation strategies on lumbar fusion in osteoporosis patients, shown in Table 3. The effect of pre-operative measures of osteoporosis on fusion outcomes
There was one study on the effect of pre-operative measures of osteoporosis on lumbar fusion outcomes, as shown in Table 1. There are quite a few studies in the literature evaluating the ability DEXA scans and Hounsfield units to accurately and reliably measure bone density in lumbar spine patients, but these routinely do not evaluate fusion rates after surgery [2,3,7-11]. Other studies are evaluating the relationship of pre-operative vitamin D levels and outcomes after spine surgery [12,13].
The study looking at bone density and fusion rates used Hounsfield units as a measure of bone mass. Schrieber et al. in 2014 evaluated the relationship between pre-operative Hounsfield units and lumbar spine fusion [14]. They studied a cohort of 28 patients who underwent stand alone lateral lumbar interbody fusion with a total of 52 fusion levels. The global bone quality as measured by Hounsfield units was significantly higher in the patients with a successful fusion compared to those with nonunions (133.7 compared to 107.3, p < 0.05).
When evaluating the bone quality at the each individual level, the levels that fused had significantly higher Hounsfield units compared to the unfused levels (203 vs. 140, p < 0.05).There is a study evaluating bone mass with DEXA scores, but the primary outcome is subsidence and not fusion rates. Tempel et al. in 2015 reviewed patients who underwent lateral lumbar interbody fusion to look for an association between pre-operative DEXA scores and interbody subsidence [15]. They found a subsidence rate of 78% in patients with low bone density (T score less than - 1.0) as compared to a subsidence rate of 22% in patients with normal bone density (T score greater than - 2.0), and this was statistically significant. While subsidence is associated with nonunion and a return of pre-operative pain, this study does not fully evaluate fusion rates.
The effect of pre-operative osteoporosis medications on lumbar fusion
There were 6 studies looking at the effect of medical treatment for osteoporosis on fusion rates after lumbar spine surgery, as shown in Table 2. Four of these studies evaluate the effect of bisphosphonates on lumbar fusion, and two studies evaluate teriparatide. There are two studies on the use of the bisphosphonate alendronate (Fosamax®). Nagahama et al. evaluated the effect of alendronate on lumbar fusion in 40 patients using a prospective, randomized trial in 2011 [16]. These patients underwent single level posterior lumbar interbody fusion with instrumentation and assessed fusion on post-operative CT scans. The patients in the alendronate group had a significantly higher fusion rate of 95% compared to 65% in the alfacalcidol (Vitamin D) group. Kim et al. also studied the effect of alendronate 44 patients undergoing single level lumbar interbody fusion and instrumentation in 2014 and found different results [17]. They found a non-statistically significant difference in the fusion rates as assessed by plain radiographs. The patients in the alendronate group had a 66.7% fusion rate, and the control group had a fusion ate of 73.9%, with an overall higher rate of patients with endplate degeneration in the alendronate group.
There are two studies on the use of zoledronate (Zometa® and Reclast®) in patients undergoing lumbar fusion. Park et al. evaluated the effect of zoledronic acid on 44 patients with lumbar spinal stenosis in 2013 [18]. These patients underwent 1 or 2 level instrumentation and fusion and were given either one dose of zoledronic acid or one dose of a control. There was no significant increase in fusion mass in the single dose zoledronic acid patients as seen on three dimensional CT scans at 6 months after surgery. Of note, there was a significant improvement in the clinical outcome measures of VAS and ODI. Tu et al. also studied the effect of zoledronic acid on fusion rates in patients with osteoporosis after posterior lumbar interbody fusion at 2 years follow up in 2014 [19]. The zoledronic acid group received an intravenous infusion at 3 and 12 months after surgery. There as a non-statistically significant difference in the zoledronic acid patients, with a fusion rate of 75%, compared to 56% in the non-zoledronic acid patients. Additionally, there was a non-statistically significantly lower VAS and ODI scores at final follow up in the zoledronic acid patients. The rate of pedicle screw loosening was significantly lowerin the zoledronic acid patients at 18% compared to 45% in the control group.
There are two prospective studies on the effect of teriparatide (Forteo®) on lumbar fusions. Ohtori et al. studied the effect of teriparatide compared to risedronate (Actonel®, a bisphosphonate) on lumbar posterolateral fusions in osteoporotic, post-menopausal women with degenerative spondylolisthesis in 2012 [20]. The administration of teriparatide or risedronate was for 2 months before the surgery and 8 months after surgery. The first 28 patients were assigned to the teriparatide group and the second 28 patients were assigned to the risedronate group. The surgery consisted of decompression, instrumentation and posterolateral fusion at the level of the spondylolisthesis. The fusion rate in the teriparatide group was 84% by radiograph and 82% by CT, compared to 74% and 68% in the risedronate group, p < 0.05. This study shows a significant advantage to teriparatide in post-menopausal, osteoporotic women undergoing lumbar spine fusion. Another study on teriparatide by Ohtoria et al. evaluated the effect of teriparatide or risedronate on pedicle screw loosening in patients undergoing one or two level instrumented posterolateral fusions with local bone graft in 2013 [21]. These 62 women had degenerative spondylolisthesis and osteoporosis. The administration of the teriparatide, risedronate or control was for 2 months before and 10 months after surgery. There was a statistically significant lower rate of pedicle screw loosening in the teriparatide group (7-13%) and equivalent rates of pedicle screw loosening in the risedronate and control group (15-26%).
The effect of surgical interventions for low bone density patients on lumbar fusion rates
There are eight studies evaluating different surgical techniques for patients with osteoporosis, as shown in Table 3. The major goal of augmented surgical techniques for patients with osteoporosis is to improve the implant/bone interface to increase stability in an otherwise weaker bone.
Cavagna et al. in 2008 evaluated 39 patients over the age of 65 who underwent arthrodesis with at least 2 years follow up [22]. Posterior spinal instrumentation and fusion was done for patients with spinal stenosis due to spondylolitheisis, scoliosis, kyphosis, or post-laminectomy syndrome with a range of fusion levels of 1-4. The bone graft used was autologous laminectomy bone and iliac crest bone. The evaluation of the fusion by an independent radiologist shows radiographic fusion in 89.7% (35/39), and CT evidence of facet fusion in 100% (39/39) of patients. The authors found asymptomatic patients with 2 broken screws and 2 broken rods at 2 year follow, that they determined were stress fractures, and not actual nonunions. This study provides a good baseline of instrumentation and fusions in patients at risk for osteoporosis.
The technique of vertebroplasty of the levels within the fusion construct was evaluated by Kim et al. in 2010 retrospectively reviewed 62 patients with lumbar spondylolisthesis at L4-5 or L5- S1 and osteoporosis who were treated with ALIF and percutaneous posterior spinal instrumentation [23]. Thirty-one patients underwent polymethacrylate cement augmentation of the ALIF, and Thirty-one did not. Dynamic radiographs and 3-D CT was performed at final follow up in 46 patients. There was no significant difference in union rate between the two groups. Of note, there was a significantly higher rate of cage subsidence the patient cohort without vertebroplasty augmentation.
There were 3 studies that evaluated the effect of cement augmentation of pedicle screws in patients with osteoporosis. Moon et al. in 2009 reported on 3 year follow up of 37 patients withosteoporosis who underwent PSFI with cement augmented cannulated pedicle screws. The pre-operative diagnoses included degenerative spondy (16.2%), isthmic spondy (13.5%), and stenosis (70.3%). They found one loose screw at 2 years post-op which implies a union rate of 97%. Pinera et al. in 2011 reviewed a series of 23 elderly patients (mean age of 77) with degenerative spondylolisthesis or lumbar spinal stenosis who underwent posterior spinal instrumentation and fusion with cement augmented cannulated screws [24]. Radiographic fusion was seen in 74% of the patients, and CT evidence of posterior and/or posterolateral fusion at 6 months was seen in all patients. Dai et al. in 2015 evaluated the effect of cement injectable cannulated pedicle screws used in 43 patients with osteoporosis who underwent posterior spinal instrumentation and fusion [25]. The diagnoses included degenerative spondylolisthesis (49%), disc herniation or spinal stenosis (34.9%), ankylosing spondylitis (9.3%), osteopetrosis or compression fractures (16.3%). The fusion was assessed at 6 and 12 months after surgery with CT scans and showed and implied union rate of 100%, since no patients required revision surgery for nonunion or screw loosening. This does not negate the possibility of asymptomatic nonunion.
There were three studies evaluating the effect of expandable pedicle screws on fusion rates in patients with osteoporosis. Cook et al. in 2001 retrospectively reviewed 152 patients who underwent posterior spinal instrumentation and fusion with iliac crest bone graft and expandable pedicle screws [26]. The design of the expandable pedicle screw was to allow the tip to expand by 2 mm. Of the patients with expandable pedicle screws, 21 were diagnosed with osteoporosis. Fusion was evaluated with dynamic radiographs. Of the patients with osteoporosis, the fusion rate was 86% (18/21) which is equivalent to the fusion rate of the total patient cohort 86% (125/145). Gazzeri et al. in 2012 evaluated 10 patients with osteoporosis treated with posterior spinal instrumentation and fusion using expandable pedicle screws [27]. The diagnoses included spondylolisthesis (4), fracture (3), lumbar spinal stenosis (1) and failed back syndrome (2). Fusion was assessed on final follow up X-ray and CT. There were no instances of motion on dynamic radiographs or screw loosening on CT. The overall fusion rate was 100%. Wu et al. in 2012 conducted a prospective randomized study comparing expandable pedicle screws to conventional pedicle screws in patients with osteoporosis and undergoing posterior spinal instrumentation and fusion [28]. The diagnoses included spondylolistheis, spondylolysis, kyphosis, cancer or pseudarthrosis. There was a minimum follow up of 24 months, and the average follow up was 43 months. The fusion was evaluated on dynamic radiographs at 2 years postop and CT 1 year post op by a blinded, independent radiologist. The expandable pedicle screw group had a significantly higher fusion rate at 92.5% (compared to 80.5%) and lower screw loosening rate of 4.1% (compared to 12.9%). All of these studies on expandable pedicle screws demonstrate a fusion rate equal to or greater than conventional pedicle screws.
Discussion
A growing portion of spine patients will have osteopenia or osteoporosis as patients remain active at an older age [2]. A previous systematic review was performed by Hirsch et al. evaluating theanimal data of osteoporosis medications on spinal fusion [29]. Since that time, a multitude of studies have been performed on the effect of osteoporosis medications on patients undergoing lumbar fusion. Additionally, more research has been performed on pre-operative evaluation of osteoporosis in patients undergoing lumbar fusion and on specific surgical techniques for patients with osteoporosis undergoing lumbar fusion. This systematic review is designed to review the highest quality studies on the diagnostic, medical and surgical technique options for patient with low bone mass undergoing lumbar fusion.While there are many studies on the pre-operative evaluation of low bone mass in lumbar spine patients, there was only one study to evaluate low bone mass measurement in relation to lumbar fusion rates. Tempe et al. and other studies, have shown that low bone mass leads to higher rates of subsidence of interbody devices [7,12,13,15,[30]. While this is not a direct evaluation of fusion rates, it can be inferred that the lack of stability will likely lead to nonunion. The study by Schrieber et al. found a correlation between low bone mass, as measure by Hounsfield Units, and lower fusion rates [14]. This demonstrates the need for alternate treatment strategies for osteoporotic patients undergoing a lumbar fusion.
Once a patient has been diagnosed with low bone density, it may be feasible to treat him or her with an osteoporosis medication before or after surgery to help improve lumbar fusion rates. The two studies comparing alendronate to controls found contrasting results. One study demonstrated improvement in fusion amongst the patients treated with alendronate, and the other study found lower fusion rates in patients treated with alendronate. The earlier animal studies studying the effect of alendronate on fusion mass showed lower bone mass with alendronate [31]. Some surgeons may decide to avoid alendronate in their patients undergoing lumbar fusion. The two studies evaluating zoledronic acid showed a lower fusion rate in one study, and a non-statistically significant higher fusion rate in the other study [18,19]. This not strong evidence in support of using zoledronic acid on osteoporotic patients undergoing spinal fusion and thus some surgeons may decide to avoid it. The two studies evaluating teriparatide both show a significantly higher rate of fusion in patients treated with teriparatide, compared to risedronate and control groups [20,21]. Since these are studies on teriparatide are prospective trials, this represents the strongest evidence for peri-operative medical treatment of osteoporosis in patients undergoing lumbar fusion. Based on the available literature, it would be feasible for surgeons to advise their patients to start treatment with teriparatide before surgery, and continue during the post-operative fusion period.
In addition to medical treatment of osteoporosis, different surgical techniques can be employed in osteoporotic patients undergoing lumbar fusion. A study by Cavagna et al. shows a baseline fusion rate of 89.7% for osteoporotic patients undergoing posterior lumbar instrumentation and fusion [22]. Modified surgical techniques should increase this fusion rate. The use of vertebroplasty in combination with ALIF and percutaneous posterior fixation showed a fusion rate of 100%, which is a 5% increase over patients treated without vertebroplasty in one study [23]. The three studies on cement augmentation of pedicle screws are retrospective in nature, and all show a fusion rate of 100% on CT evaluation [24,25,32]. The three studies on expandable pedicle screws show a fusion rate of 86-100% based on radiographs and CT [26-28]. The study by Wu et al. had the highest number of patients as well as prospective and randomized with an independent radiologist evaluation of fusion. The fusion rate found by Wu et al. of 92.5% is the most accurate assessment of expandable pedicle screws [28].
One limitation to this systematic review is the low number of prospective, randomized studies on the topic of osteoporosis and lumbar spinal fusion currently in the literature. This highlights the need for high quality studies, prospective and randomized, that can provide meaningful information to providers that can guide treatment decisions. This will become more important in the coming years as our elderly population increases.
Future directions in this field will include clinical studies on denosumab, a RANK L binder. There are a large number of studies demonstrating increased bone mass and decreased markers of turnover in women with osteoporosis treated with denosumab [33-35]. Based on these promising results on osteoporosis, the effect of denosumab on lumbar fusion needs to be evaluated.
Conclusion
This systematic review of the existing literature determined that there are 15 studies evaluating the effect of treatment strategies for low bone density on lumbar fusion rates. There is a lower rate of fusions in patients with low bone density as measured with Hounsfield units on lumbar CT. Bisphosphonates do not increase rates of lumbar fusion. Forteo increased bone fusion mass, fusion rates, and decreases pedicle screw loosening in lumbar spine fusions. The use of expandable pedicle screws and cement augmented pedicle screws increases the fusion rate in osteoporotic patients compared to conventional pedicle screws. Due to the prospective, randomized nature of the studies, the best evidence for strategies in osteoporotic patients undergoing lumbar fusion is peri-operative use of teriparatide and expandable pedicle screws.References
- (2002) Report of the Surgeon General's Workshop on Osteoporosis and Bone Health: December 12 - 13, 2002, Washington, DC, USA.
- Chin DK, Park JY, Yoon YS, Kuh SU, Jin BH, et al. (2007) Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int 18: 1219-1224.
- Andersen T, Christensen FB, Langdahl BL, Ernst C, Fruensgaard S, et al. (2013) Degenerative spondylolisthesis is associated with low spinal bone density: a comparative study between spinal stenosis and degenerative spondylolisthesis. Biomed Res Int 2013: 123847<
- Reports of the Surgeon General (2004) Bone health and osteoporosis: a report of the surgeon general. Office of the Surgeon General, Rockville (MD), USA.
- Yoon ST, Boden SD (2004) Spine fusion by gene therapy. Gene Ther 11: 360-367.
- Choudhri TF, Mummaneni PV, Dhall SS, Eck JC, Groff MW, et al. (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 4: radiographic assessment of fusion status. J Neurosurg Spine 21: 23-30.
- Genant HK, Block JE, Steiger P, Glueer CC, Smith R (1987) Quantitative computed tomography in assessment of osteoporosis. Semin Nucl Med 17: 316-333.
- Dodwad SM, Khan SN (2013) Surgical stabilization of the spine in the osteoporotic patient. Orthop Clin North Am 44: 243-249.
- Lee S, Chung CK, Oh SH, Park SB (2013) Correlation between bone mineral density measured by dual-energy X-ray absorptiometry and Hounsfield units measured by diagnostic CT in lumbar spine. J Korean Neurosurg Soc 54: 384-389.
- Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 93: 1057-1063.
- Tay WL, Chui CK, Ong SH, Ng AC (2012) Osteoporosis screening using areal bone mineral density estimation from diagnostic CT images. Acad Radiol 19: 1273-1282.
- Kim TH, Yoon JY, Lee BH, Jung HS, Park MS, et al. (2012) Changes in vitamin D status after surgery in female patients with lumbar spinal stenosis and its clinical significance. Spine (Phila Pa 1976) 37: E1326-E1330.
- Stoker GE, Buchowski JM, Bridwell KH, Lenke LG, Riew KD, et al. (2013) Preoperative vitamin D status of adults undergoing surgical spinal fusion. Spine (Phila Pa 1976) 38: 507-515.
- Schreiber JJ, Hughes AP, Taher F, Girardi FP (2014) An association can be found between hounsfield units and success of lumbar spine fusion. HSS J 10: 25-29.
- Tempel ZJ, Gandhoke GS, Okonkwo DO, Kanter AS (2015) Impaired bone mineral density as a predictor of graft subsidence following minimally invasive transpsoas lateral lumbar interbody fusion. Eur Spine J 24 Suppl 3: 414-419.
- Nagahama K, Kanayama M, Togawa D, Hashimoto T, Minami A (2011) Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine 14: 500-507.
- Kim SM, Rhee W, Ha S, Lim JH, Jang IT (2014) Influence of alendronate and endplate degeneration to single level posterior lumbar spinal interbody fusion. Korean J Spine 11: 221-226.
- Park YS, Kim HS, Baek SW, Kong DY, Ryu JA (2013) The effect of zoledronic acid on the volume of the fusion-mass in lumbar spinal fusion. Clin Orthop Surg 5: 292-297.
- Tu CW, Huang KF, Hsu HT, Li HY, Yang SS, et al. (2014) Zoledronic acid infusion for lumbar interbody fusion in osteoporosis. J Surg Res 192: 112-116.
- Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, et al. (2012) Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine (Phila Pa 1976) 37: E1464-E1468.
- Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, et al. (2013) Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine (Phila Pa 1976) 38: E487-E492.
- Cavagna R, Tournier C, Aunoble S, Bouler JM, Antonietti P, et al. (2008) Lumbar decompression and fusion in elderly osteoporotic patients: a prospective study using less rigid titanium rod fixation. J Spinal Disord Tech 21: 86-91.
- Kim KH, Lee SH, Lee DY, Shim CS, Maeng DH (2010) Anterior bone cement augmentation in anterior lumbar interbody fusion and percutaneous pedicle screw fixation in patients with osteoporosis. J Neurosurg Spine 12: 525-532.
- Pinera AR, Duran C, Lopez B, Saez I, Correia E, et al. (2011) Instrumented lumbar arthrodesis in elderly patients: prospective study using cannulated cemented pedicle screw instrumentation. Eur Spine J 20 Suppl 3: 408-414.
- Dai F, Liu Y, Zhang F, Sun D, Luo F, et al. (2015) Surgical treatment of the osteoporotic spine with bone cement-injectable cannulated pedicle screw fixation: technical description and preliminary application in 43 patients. Clinics (Sao Paulo) 70: 114-119.
- Cook SD, Barbera J, Rubi M, Salkeld SL, Whitecloud TS 3rd (2001) Lumbosacral fixation using expandable pedicle screws. an alternative in reoperation and osteoporosis. Spine J 1: 109-114.
- Gazzeri R, Roperto R, Fiore C (2012) Litanium expandable pedicle screw for the treatment of degenerative and traumatic spinal diseases in osteoporotic patients: preliminary experience. Surg Technol Int 22: 320-325.
- Wu ZX, Gong FT, Liu L, Ma ZS, Zhang Y, et al. (2012) A comparative study on screw loosening in osteoporotic lumbar spine fusion between expandable and conventional pedicle screws. Arch Orthop Trauma Surg 132: 471-476.
- Hirsch BP, Unnanuntana A, Cunningham ME, Lane JM (2013) The effect of therapies for osteoporosis on spine fusion: a systematic review. Spine J 13: 190-199.
- Meredith DS, Schreiber JJ, Taher F, Cammisa FP Jr, Girardi FP (2013) Lower preoperative Hounsfield unit measurements are associated with adjacent segment fracture after spinal fusion. Spine (Phila Pa 1976) 38: 415-418.
- Lehman RA Jr, Kuklo TR, Freedman BA, Cowart JR, Mense MG, et al. (2004) The effect of alendronate sodium on spinal fusion: a rabbit model. Spine J 4: 36-43.
- Moon BJ, Cho BY, Choi EY, Zhang HY (2009) Polymethylmethacrylate-augmented screw fixation for stabilization of the osteoporotic spine : a three-year follow-up of 37 patients. J Korean Neurosurg Soc 46: 305-311.
- Anastasilakis AD, Polyzos SA, Efstathiadou ZA, Savvidis M, Sakellariou GT, et al. (2015) Denosumab in treatment-naive and pre-treated with zoledronic acid postmenopausal women with low bone mass: Effect on bone mineral density and bone turnover markers. Metabolism 64: 1291-1297.
- Papapoulos S, Lippuner K, Roux C, Lin CJ, Kendler DL, et al. (2015) The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM Extension study. Osteoporos Int 26: 2773-2783.
- Gu HF, Gu LJ, Wu Y, Zhao XH, Zhang Q, et al. (2015) Efficacy and safety of denosumab in postmenopausal women with osteoporosis: a meta-analysis. Medicine (Baltimore) 94: e1674.