Journal of Orthopedics & Rheumatology
A Systematic Approach to Evaluating Knee Radiographs with a Focus on Osteoarthritis
Christopher M Melnic*, Joshua Gordon, P Maxwell Courtney, and Neil P Sheth
- University of Pennsylvania, Department of Orthopaedic Surgery Hospital of the University of Pennsylvania, USA
*Address for Correspondence: Christopher M Melnic, Hospital of the University of Pennsylvania, Department of Orthopaedic Surgery, 3400 Spruce Street, 2 Silverstein Philadelphia, PA 19104, USA, Tel: 610-751-3986; E-mail: Christopher.Melnic@uphs.upenn.edu
Citation: Melnic CM, Gordon J, Courtney PM, Sheth NP. A Systematic Approach to Evaluating Knee Radiographs with a Focus on Osteoarthritis. J Orthopedics Rheumatol. 2014;1(2): 6.
Copyright © 2014 Melnic CM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology |ISSN: 2334-2846 | Volume: 1, Issue: 2
Submission: 25 December 2013 | Accepted: 29 January 2014 | Published: 06 February 2014
Reviewed & Approved by: Dr. Jun Li Division of Clinical Immunology & Rheumatology, University of Alabama at Birmingham, USA
Abstract
Arthritis of the knee is commonly encountered in primary care and specialty settings. The initial work up and treatment of these patients requires a thorough evaluation and complete series of plain radiographs. Despite increased use of advanced imaging modalities, plain films remain the most instructive, available, and affordable diagnostic test. The evaluation of patients with arthritis can be challenging, by using a standardized approach one can perform a quick and adequately comprehensive evaluation. Here we outline an approach appropriate for the evaluation of these patients in any setting. Particularly, we advocate a complete history and physical exam augmented by a four view radiographic series: A weight bearing anterior-posterior (AP) of the knee, a 45 degree weight bearing posterior-anterior (PA) view of the knee, a standing lateral, and a Merchant view. Through our described systematic evaluation of these views, a great deal of information can be obtained often helping guide treatment plans created with the patient, and helping avoid a potential missed or delayed diagnosis.Background
Osteoarthritis (OA) is the most common form of arthritis, and the knee is the principal large joint affected by this process [1]. In men and women over the age of fifty-five, an estimated ten percent develop disabling knee pain from OA; 25% of those affected are considered severely disabled [2]. The incidence of osteoarthritis of the knee increases with age, is strongly associated with obesity [3], and more commonly affects women [4]. OA is the single greatest contributor to disability [5,6], and in the elderly, its overall risk of disability is comparable to that of cardiovascular disease. The precise etiology, pathogenesis, and progression of OA are not yet completely understood.Systematic Approach to the Arthritic Knee
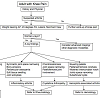
In the evaluation of the adult patient with degenerative joint disease of the knee, we suggest a systematic approach (Figure 1). Each patient should receive a thorough history and physical examination. Imaging by means of plain radiographs is valuable as a confirmatory test, but has been proven to be less sensitive and specific than clinical assessment by a physician [11]. There is often a disparity between clinical and radiographic severity of disease, and in most circumstances, radiographs do not provide a good metric by which to measure the likelihood of progression [11-13]. Although it is important to be aware of these limitations, radiographs remain the gold standard imaging modality [11,14,15]. Magnetic Resonance imaging (MRI) and other imaging modalities may prove useful but are often impractical and costly with limited availability in many settings. MRI should never be used as an initial evaluation tool for the painful knee. Weight bearing radiographs provide far more clinical information about the functional joint space than a non-weight bearing MRI performed in the supine position. Furthermore, these advanced imaging modalities infrequently supplement a standard radiographic series in patients with moderate to severe degenerative joint disease.
Radiographic Hallmarks of other Joint Diseases
Evaluation of secondary arthritis requires the same four radiographs. The underlying etiology can often be heralded by key radiographic features, which can help differentiate knee pain caused by secondary conditions. Here we outline some of the common causes of secondary arthritis and the radiographic features useful in diagnosis.
Joint destruction associated with hemophilia is also seen at a young age. Numerous intra-articular hemorrhages throughout a hemophiliac patient’s life may result in articular cartilage damage yielding chronic synovitis causing further joint destruction. Radiographic analysis typically demonstrates flattening of the distal femoral condyles, enlargement and widening of the epiphysis, trabecular accentuation, widening of the intercondylar notch, and squaring of the inferior margin of the patella [39]. The thickened synovium that results from this chronic process leads to marginal erosions and subarticular cyst formation. Joint effusion is typically encountered in the setting of an acute hemarthrosis.
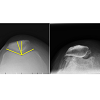
The knee is the most common joint affected by calcium pyrophosphate dihydrate (CPPD) deposition disease. The diagnosis is most commonly confirmed by knee joint aspiration, demonstrating the presence of rhomboid shaped crystals in the synovial fluid that are positively birefringent under a polarizing microscope. CPPD crystals are deposited in the articular cartilage resulting in chondrocalcinosis, and the fibrocartilagenous structures of the knee become calcified and can become evident radiographically. Calcification of the menisci is usually seen, and the lateral meniscus is most commonly involved. On the lateral radiograph, calcification of the gastrocnemius tendon may also be appreciated [40]. Degenerative changes in CPPD affect the patellofemoral joint more frequently than the other compartments (Figures 8 and 9) [36].
Conclusion
Our systematic approach outlines a method for evaluating the patient with knee pain and suspected osteoarthritis. As such a prevalent condition, and one seen by nearly all medical specialties, our system provides a helpful guide regarding which radiographs to order, the correct technique to obtain to proper radiographic projections, what key features to evaluate on each view, and in general terms when to refer to a specialist. Initial radiographs should include four views: a (1) weight bearing AP, a (2) weight bearing 45 degree PA, a (3) standing lateral, and a (4) Merchant view. Each radiograph should first be evaluated for quality and then for pathology. An analysis, performed in a stepwise fashion (Figure 1), allows the treating physician to fully assess the radiographs of the osteoarthritic knee in a reproducible fashion.References
- Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, et al. (2003) EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 62: 1145-1155.
- Peat G, McCarney R, Croft P (2001) Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis 60: 91-97.
- Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF (1988) Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med 109: 18-24.
- Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, et al. (1987) The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 30: 914-918.
- Doherty M (2001) Risk factors for progression of knee osteoarthritis. Lancet 358: 775-776.
- Jordan JM, Linder GF, Renner JB, Fryer JG (1995) The impact of arthritis in rural populations. Arthritis Care Res 8: 242-250.
- Ringdahl E, Pandit S (2011) Treatment of knee osteoarthritis. Am Fam Physician 83: 1287-1292.
- Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, et al. (2000) Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 133: 635-646.
- Spector TD and MacGregor AJ (2004) Risk factors for osteoarthritis: genetics. Osteoarthritis Cartilage 12: S39-44.
- Kerkhof HJ, Bierma-Zeinstra SM, Arden NK, Metrustry S, Castano-Betancourt M, et al. (2013) Prediction model for knee osteoarthritis incidence, including clinical, genetic and biochemical risk factors. Ann Rheum Dis.
- Hunter DJ, Guermazi A, (2012) Imaging techniques in osteoarthritis. PM R 4: S68-S74.
- Ding C, Zhang Y, Hunter D (2013) Use of imaging techniques to predict progression in osteoarthritis. Curr Opin Rheumatol 25: 127-135.
- Bruyere O, Honore A, Rovati LC, Giacovelli G, Henrotin YE, et al. (2002) Radiologic features poorly predict clinical outcomes in knee osteoarthritis. Scand J Rheumatol 31: 13-16.
- Altman RD, Gold GE (2007) Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage 15: A1-56.
- Altman RD, Hochberg M, Murphy WA Jr, Wolfe F, Lequesne M (1995) Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage 3: 3-70.
- Merle-Vincent F, Vignon E, Brandt K, Piperno M, Coury-Lucas F, et al. Superiority of the Lyon schuss view over the standing anteroposterior view for detecting joint space narrowing, especially in the lateral tibiofemoral compartment, in early knee osteoarthritis. Ann Rheum Dis 66: 747-753.
- Cromer MS, Bourne RM, Fransen M, Fulton R, Wang SC (2013) Responsiveness of quantitative cartilage measures over one year in knee osteoarthritis: Comparison of radiography and MRI assessments. J Magn Reson Imaging.
- Conrozier T, Vignon E (1996) Quantitative radiography in osteoarthritis: computerized measurement of radiographic knee and hip joint space. Baillieres Clin Rheumatol 10: 429-433.
- Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM (1988) The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am 70: 1479-1483.
- Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56: 1391-1396.
- Kellgren JH and Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16: 494-502.
- Krasnokutsky S, Samuels J, Abramson SB (2007) Osteoarthritis in 2007. Bull NYU Hosp Jt Dis 65: 222-228.
- Cicuttini FM, Baker J, Hart DJ, Spector TD (1996) Association of pain with radiological changes in different compartments and views of the knee joint. Osteoarthritis Cartilage 4: 143-147.
- Spector TD, Hart DJ, Byrne J, Harris PA, Dacre JE, et al. (1993) Definition of osteoarthritis of the knee for epidemiological studies. Ann Rheum Dis 52: 790-794.
- Messieh SS, Fowler PJ, Munro T (1990) Anteroposterior radiographs of the osteoarthritic knee. J Bone Joint Surg Br, 1990. 72: 639-640.
- Resnick D and Vint V (1980) The "Tunnel" view in assessment of cartilage loss in osteoarthritis of the knee. Radiology 137: 547-548.
- Insall J and Salvati E (1971) Patella position in the normal knee joint. Radiology 101: 101-104.
- Greenspan A (2011) Orthopedic imaging : a practical approach. 5th Edition, Philadelphia: Lippincott Williams & Wilkins.
- Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, et al. (2002) Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis 61: 617-622.
- Cheung PP, Gossec L, Dougados M (2010) What are the best markers for disease progression in osteoarthritis (OA)? Best Pract Res Clin Rheumatol 24: 81-92.
- Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, et al. (2009) Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum 61: 459-467.
- Conrozier T, Favret H, Mathieu P, Piperno M, Provvedini D, et al. (2004) Influence of the quality of tibial plateau alignment on the reproducibility of computer joint space measurement from Lyon schuss radiographic views of the knee in patients with knee osteoarthritis. Osteoarthritis Cartilage 12: 765-770.
- Vignon E, Piperno M, Le Graverand MP, Mazzuca SA, Brandt KD, et al. (2003) Measurement of radiographic joint space width in the tibiofemoral compartment of the osteoarthritic knee. Comparison of standing anterioposterior Lyon schuss views. Arthritis Rheum 48: 378-384.
- Buckland-Wright C (2006) Which radiographic techniques should we use for research and clinical practice? Best Pract Res Clin Rheumatol 20: 39-55.
- Hawker G, Wright J, Coyte P, Paul J, Dittus R, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am 80: 163-173.
- Jacobson JA, Girish G, Jiang Y, Sabb BJ (2008) Radiographic evaluation of arthritis: degenerative joint disease and variations. Radiology 248: 737-747.
- Jacobson JA, Girish G, Jiang Y, Resnick D (2008) Radiographic evaluation of arthritis: inflammatory conditions. Radiology 248: 378-389.
- Kan JH (2013) Juvenile idiopathic arthritis and enthesitis-related arthropathies. Pediatr Radiol 43: S172-180.
- Arnold WD, Hilgartner MW (1977) Hemophilic arthropathy. Current concepts of pathogenesis and management. J Bone Joint Surg Am 59: 287-305.
- Yang BY, Sartoris DJ, Resnick D, Clopton P (1996) Calcium pyrophosphate dihydrate crystal deposition disease: frequency of tendon calcification about the knee. J Rheumatol 23: 883-888.