Journal of Orthopedics & Rheumatology
Download PDF
Review Article
*Address for Correspondence: P Maxwell Courtney, Hospital of the University of Pennsylvania, Department of Orthopaedic Surgery, 3400 Spruce Street, 2 Silverstein, Philadelphia, PA 19104, Tel: 215-964-1747 ; E-mail: Paul.Courtney@uphs.upenn.edu
Citation: Courtney PM, Melnic CM, Howard M, Makani A, Sheth NP. A Systematic Approach to Evaluating Hip Radiographs-A Focus on Osteoarthritis. J Orthopedics Rheumatol. 2014;2(1): 7.
Copyright © 2014 Courtney PM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 1, Issue: 2
Submission: 09 December 2013 | Accepted: 10 January 2014 | Published: 21 January 2014
Reviewed & Approved by: Dr. Guangju Zhai is an Associate Professor in population and statistical genetics, Discipline of Genetics, Faculty of Medicine at Memorial University of Newfoundland, Canada
A Systematic Approach to Evaluating Hip Radiographs-A Focus on Osteoarthritis
P Maxwell Courtney*, Christopher M Melnic, Mark Howard, Amun Makani, and Neil P Sheth
- Department of Orthopedic Surgery, Hospital of the University of Pennsylvania, University of Pennsylvania, USA
*Address for Correspondence: P Maxwell Courtney, Hospital of the University of Pennsylvania, Department of Orthopaedic Surgery, 3400 Spruce Street, 2 Silverstein, Philadelphia, PA 19104, Tel: 215-964-1747 ; E-mail: Paul.Courtney@uphs.upenn.edu
Citation: Courtney PM, Melnic CM, Howard M, Makani A, Sheth NP. A Systematic Approach to Evaluating Hip Radiographs-A Focus on Osteoarthritis. J Orthopedics Rheumatol. 2014;2(1): 7.
Copyright © 2014 Courtney PM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 1, Issue: 2
Submission: 09 December 2013 | Accepted: 10 January 2014 | Published: 21 January 2014
Reviewed & Approved by: Dr. Guangju Zhai is an Associate Professor in population and statistical genetics, Discipline of Genetics, Faculty of Medicine at Memorial University of Newfoundland, Canada
Abstract
Osteoarthritis of the hip continues to be a common cause of disability affecting millions worldwide. Identifying radiographic changes can help provide an accurate diagnosis and help guide the clinical decision making process. Obtaining proper, reliable radiographic views and having standardized parameters for assessing plain radiographs are essential to the management of hip osteoarthritis. The purpose of this review is to provide Internists, Physiatrists, Rheumatologists, and Orthopedic Surgeons a systematic method for evaluating radiographs to determine the appropriate diagnosis, treatment approach, and timing of referral in the patient with hip osteoarthritis.Keywords
Osteoarthritis; Hip; Radiographs; Systematic approachBackground
Osteoarthritis continues to be the most common arthropathy, affecting more than 20 million patients in the United States alone [1]. The prevalence of hip osteoarthritis ranges from 3-6% in Caucasians, and has remained relatively constant over the past four decades [2], while epidemiological data from Asian, African, and Indian populations report a lower prevalence [3-5]. Men appear to be affected more than women by a factor of 2 to 1 [6]. While only 2% of the population has radiographic evidence of hip osteoarthritis by age 50, the prevalence is over 10% by age 75 [6].Hip osteoarthritis represents a heterogeneous group of conditions resulting in the degeneration of the hyaline cartilage of the joint. This disease has been implicated as a frequent cause of disabling pain in the general population and as the most common cause of disability in developed countries [7,8]. Pre-existing pathology such as Developmental Dysplasia of the Hip (DDH), previous traumatic injury, Slipped Capital Femoral Epiphysis (SCFE), or Avascular Necrosis (AVN) of the femoral head can result in degenerative changes in the hip resulting in secondary osteoarthritis [9]. Primary osteoarthritis is generally considered idiopathic and its etiology continues to be of much debate in the literature. Multiple theories for progression of primary hip osteoarthritis have been proposed including anatomic, genetic, mechanical, and hormonal etiologies [10].
The approach to a patient with osteoarthritis of the hip begins with a thorough history and physical examination. Pain is the most common presenting symptom; however, the progression may be slow, often occurring over several years, and the disease severity does not always correlate to the degree of presenting symptoms. Patients often complain of anterior groin pain, but may also report difficulty with hip range of motion during activities of daily living (e.g. putting on shoes and socks). The treating physician should inquire about previous hip or pelvis trauma as well as any congenital childhood diseases of the hip. A pertinent family and social history are also important as an increased rate of hip osteoarthritis has been linked to heavy labor [11] and a family history of the disease has been found in sibling and twin studies [12,13]. Physical examination of the hip will often reveal limited and painful range of motion. Identification of any leg length discrepancy or soft-tissue contracture (i.e. flexion or adduction) should be documented. An assessment of ambulation is useful for determining trendelenburg (e.g. abductor weakness) or antalgic gait patterns.
The authors suggest weight-bearing radiographs in all patients for initial workup of osteoarthritis of the hip. Anteroposterior (AP) radiographs of the pelvis and hip along with a frog-leg lateral of the affected hip should be considered standard in assessing the adult patient with a painful hip [14]. The purpose of this review is to provide Internists, Physiatrists, Rheumatologists, and Orthopaedic Surgeons a systematic method for evaluating radiographs to determine the appropriate diagnosis, treatment approach, and timing of referral in the patient with hip osteoarthritis.
The third and fourth radiographic lines are the iliopectineal and ilioischial lines, respectively. The iliopectineal line represents th eanterior column of the pelvis, while the ilioischial line, also known as Kohler’s line, represents the posterior column. These lines are important in the identification of variations of the hip with regards to the anatomic relationship of the femoral head and the acetabulum.
In order to obtain a proper frog-leg lateral radiograph of the hip, the patient should be supine with the affected limb flexed at the knee approximately 30 to 40 degrees with the hip abducted 45 degrees [14]. This view allows for visualization of the anterior and posterior aspects of the femoral neck, as well as the lateral aspect of the femoral head and proximal femur [9]. Additional views of the pelvis and hip such as the 45 and 90 degree Dunn view and false profile view can give more information regarding the femur and acetabulum, respectively, but are not routinely ordered during the initial evaluation of hip pain [14].
Radiographic variations that may cause structural instability should also be carefully scrutinized. The lateral center-edge angle is a useful measurement of acetabular coverage of the femoral head [24]. It is calculated as the angle between the line through the center of the femoral head perpendicular to the transverse axis of the pelvis and a line from the center of the femoral head to the most superolateral point of the weight bearing surface of the acetabulum (Figure 7). Values less than 25 degrees may indicate inadequate coverage of the femoral head [14] and are frequently seen with DDH. Anatomic pathology can also occur if there is too much coverage of the femoral head. Protrusio acetabuli is an uncommon defect where the medial aspect of the femoral head is medial to the ilioischial line. The socket is too deep and can cause limitation of range of motion due to femoral neck impingement on the acetabulum. Patients with prior trauma, Rheumatoid Arthritis (RA), and Paget’s disease may present with protrusion [25]. The relationship of the femoral head to the ilioischial line and the integrity of the medial acetabular wall (tear drop) on the AP pelvis radiograph should be evaluated and referral to an Orthopaedic Surgeon (i.e. Adult Hip and Knee Reconstruction Specialist) should be considered in cases of severe protrusio.
Systematic Approach to Hip Radiographs
When evaluating hip arthritis, three weight-bearing radiographs are essential to determine the severity of hip disease, and allow for visualization of the functional joint space. Proper radiographic technique must be utilized in obtaining all hip radiographs. The use of a radiopaque marker of known size (e.g. 25 mm) can be helpful in preoperative templating, should surgical treatment be indicated. Care should be taken to ensure that the marker is placed as close as possible to the femoral head in the anteroposterior plane to avoid magnification error.The first radiograph that should be examined is the AP radiograph of the pelvis. It is important to be able to assess the quality of the image. The lower extremities should be positioned in approximately 15 degrees of internal rotation, which decreases the femoral anteversion (usually 12-15 degrees) and allows for better visualization of the femoral neck [15]. One must ensure proper sagittal and coronal alignment of the radiograph to confirm there is no malrotation of the pelvis. Measurement of the distance from the sacrococcygeal junction to superior symphysis pubis indicates proper sagittal pelvic rotation and is normally between 3 and 5 cm [16]. In addition, the center of the sacrum should be in line with the symphysis pubis and the obturator foramina should be symmetric resulting in proper coronal plane rotation (Figure 1).
Once an adequate AP pelvis radiograph has been obtained, seven key radiographic lines and landmarks should be evaluated: anterior and posterior wall, ilioischial and iliopectineal lines, sourcil, teardrop, and Shenton’s line. While Letournel originally described six of these fundamental radiographic lines for evaluating traumatic fractures of the pelvis, these radiographic landmarks can be extrapolated for assessment of a standard radiograph [17]. First, the anterior and posterior walls of the acetabulum need to be evaluated to determine the anteversion or relative retroversion of the native acetabulum. Typically, the line representing the posterior wall should be lateral to the line representing the anterior wall indicating proper acetabular anteversion. If the lines of the anterior and posterior walls cross, the acetabulum is retroverted. This “cross-over sign” (Figure 2) is implicated in pathologies such as DDH and femoroacetabular impingement (FAI) [9].
The third and fourth radiographic lines are the iliopectineal and ilioischial lines, respectively. The iliopectineal line represents th eanterior column of the pelvis, while the ilioischial line, also known as Kohler’s line, represents the posterior column. These lines are important in the identification of variations of the hip with regards to the anatomic relationship of the femoral head and the acetabulum.
The fifth radiographic landmark is the sourcil (translated as eyebrow from the French language), a radiodense subchondral region of bone in the weight-bearing portion of the acetabulum. The sourcil is important in determining the degree of acetabular dysplasia (femoral head coverage) as well as the degree of remaining acetabular bone stock.
Next, the tear drop should be examined. The normal shape of the tear drop is a “U” and represents the true floor of the acetabulum. It is located at the inferomedial portion of the acetabulum, just superior to the obturator foramen, and denotes the radiographic confluence of the ilium, ischium and pubis. The ilioischial or Kohler’s line is adjacent to the medial wall of the tear drop and positioning of the femoral head medial to this line signifies acetabular bone loss and/or medial femoral head migration within the confines of the acetabulum.
Finally, Shenton’s line is formed along the superior aspect of the obturator foramen and the inferior border of the femoral neck and should be continuous. This line is a useful surrogate for leg length and anatomic comparison to the contralateral hip. Figure 3 demonstrates the normal relationship of these radiographic landmarks on the AP pelvis radiograph while Figure 4 demonstrates the landmarks on an osteoarthritic hip.
After evaluating the AP pelvis radiograph, the AP and lateral radiographs of the hip should be assessed (Figure 5). Obtaining a proper AP hip radiograph requires the same technique to counter the native hip anteversion. Similar to the AP pelvis, the seven key radiographic lines and landmarks should be re-evaluated on the AP hip projection. Additionally, the neck-shaft angle (angle between the femoral neck and the femoral shaft) should be measured, while the cortices of the femoral neck and proximal femoral shaft should be assessed for thickness, bone quality and anatomic variation.
In order to obtain a proper frog-leg lateral radiograph of the hip, the patient should be supine with the affected limb flexed at the knee approximately 30 to 40 degrees with the hip abducted 45 degrees [14]. This view allows for visualization of the anterior and posterior aspects of the femoral neck, as well as the lateral aspect of the femoral head and proximal femur [9]. Additional views of the pelvis and hip such as the 45 and 90 degree Dunn view and false profile view can give more information regarding the femur and acetabulum, respectively, but are not routinely ordered during the initial evaluation of hip pain [14].
Radiographic Evaluation of the Arthritic Hip
Osteoarthritis is a form of non-inflammatory arthritis and the most common cause of end-stage destruction of the hip joint. Patients usually present with swelling, stiffness, and pain. Physical exam can reveal loss of range of motion of the hip as well as pain with resisted hip flexion. Typically, patients with an arthritic hip will exhibit obligate external rotation while flexing the hip due to soft tissue contracture. Initial work-up should include weight bearing AP pelvis, AP hip and frog lateral radiographs. Asymmetric joint space narrowing is the radiographic hallmark of osteoarthritis [18]. The joint space narrowing most commonly is confined to the superior weight-bearing portion of the joint. Less frequently, the joint space narrowing is confined to the infero-medial aspect of the joint [19]. The narrowing seen in osteoarthritis (Figure 6) is associated with reactive sclerosis, marginal osteophytes, subchondral cyst formation and superolateral subluxation of the femoral head [9]. The American College of Rheumatology has used the presence of osteophytes and joint space narrowing as the basis for their classification of osteoarthritis of the hip [20].Careful scrutiny of pelvic and hip radiographs by the clinician is essential in evaluating patients with osteoarthritis of the hip. We recommend an algorithmic approach to analyzing radiographs to help guide diagnosis, treatment and timing of referral to a specialist. The treating physician should first exclude alternate causes of hip pain, which may be evident on the AP pelvis radiograph. Patients with degenerative scoliosis of the lumbosacral spine or a fixed spinal deformity such as Diffuse Idiopathic Skeletal Hyperostosis (DISH) frequently may present with referred hip pain [21]. Pathology of the axial skeleton noted on the AP radiograph should prompt further evaluation of the spine and possible referral to a Physiatrist. Prior lumbosacral fusion with instrumentation should also be noted.
Additional fixed spinal deformities such as Ankylosing Spondylitis (AS) can also result in referred pain to the hip and should prompt referral to a Rheumatologist. Radiographic diagnosis of AS on the pelvic radiograph can be made by identifying subtle sclerosis and calcifications or auto-fusion of the sacroiliac joints [22]. Fixed spinal deformities may also yield increased pelvic obliquity and should be noted on the AP radiograph. Flexion contractures, scoliosis, and leg length discrepancy may also lead to pelvic malalignment in the coronal plane [23].
Attention should then be focused on evaluating the acetabulum, which is best examined on the AP pelvis radiograph. The clinician should note the presence of any previous hardware from prior surgeries. Pelvic osteotomies for dysplasia or acetabular fixation after acute trauma may be contributing to the etiology of the patient’s hip disease. Anatomic variations with regards to the shape and location of the femoral head within the acetabulum should be documented. Patients with osteoporosis or osteopenia may present with significant acetabular bone loss on their radiographs; the location and severity of any bone loss should be noted.
Next, the radiographs should be assessed for a leg length discrepancy. A line connecting the inferior aspect of the ischial tuberosities should intersect the same point on the proximal femur. By measuring the distance from this line to the top of the lesser trochanter on each femur, a difference in leg length can be identified (Figure 7). It is important to understand that soft-tissue contractures about the hip joint may make leg length discrepancy appear more severe; a radiograph is a two-dimensional image of a three-dimensional problem. A comparison to the contralateral hip on the AP pelvis radiograph is a good method to identify the presence of any anatomic variations or asymmetric differences.
Figure 7: A systematic method of evaluating the AP pelvis. No previous hardware is noted. There is no evidence of bone loss. Transischial line and symmetric Shenton’s lines demonstrate that leg lengths are equal. The lateral center-edge angle is normal indicating adequate coverage of the femoral head. There is no protrusio as the femoral head is lateral the ilioischial line. The presence of an inferior acetabular osteophyte and a femoral neck osteophyte (CAM lesion) is noted. The neck length and neck-shaft angle are measured.
When evaluating the radiographs of the acetabulum of any patient with hip pain, the clinician should look for the presence and location of osteophytes. Inferior osteophytes are often seen in later stages of osteoarthritis, however, a lateral acetabular osteophyte, known as a pincer lesion, can result in FAI [26]. Asphericity of the femoral head and neck can result from a CAM lesion and also play a role in FAI. The alpha angle, which is measured as the angle between a line bisecting the femoral neck and a line drawn from the center of the femoral head to the head neck junction, will also be increased in cases of FAI [26]. This can result in early impingement of the femoral neck on the anterior acetabulum with hip flexion. It has been implicated as a cause for early osteoarthritis of the hip [27] and early diagnosis may be critical for the prevention of progressive osteoarthritis of the hip.
The anatomy of the proximal femur can best be appreciated on both the AP hip and frog-leg lateral radiographs. The length of the femoral neck and neck shaft angle should be noted from the AP hip projection. Patients with a reduced neck-shaft angle of less than 120 degrees known as coxa vara can result in shortening of the affected extremity and development of a limp. Causes are usually congenital or developmental, however, patients with metabolic bone disease, prior trauma, or bone tumors can present with coxa vara. Excessive bowing of the proximal femur is usually evident on the frog-lateral projection. Prior hip deformities in childhood can result in a persistent deformity of the proximal femur as an adult [27]. Conditions such as DDH, Perthes’ disease, SCFE, and multiple epiphyseal dysplasia can result in early degenerative arthritis of the hip [9].
Treatment options include physical therapy, anti-inflammatory medication, and activity modification. Holding a cane in the contralateral hand decreases the joint reactive forces across the affected hip and can result in a significant decrease in the amount of hip pain associated with ambulation. Intra-articular corticosteroid injections are not as effective as in the knee due to a smaller effective joint space, however may have a greater response in patients with an infero-medial arthritis pattern. Referral to an Orthopaedic Surgeon for total hip arthroplasty should be made after the patient has failed conservative treatment.
Radiographic Hallmarks of Other Joint Diseases of the Hip
In comparison to osteoarthritis, RA is characterized by symmetric concentric joint space narrowing. Periarticular erosionsand osteopenia as well as protrusio acetabuli can also be appreciated on radiographs. Progression of RA leads to complete destruction of the joint and eventually to bony fusion [28]. Symptoms of RA include the insidious onset of morning stiffness of the hip joint and polyarticular involvement. A thorough physical exam may identify subcutaneous nodules or deformities of the hands and feet. Larger joints such as the hip do not become involved until late in the disease process. Treatment of the underlying pathology with Disease Modifying Antirheumatic Drugs (DMARDs) and anti-inflammatory medications for pain control is the first line of treatment. Referral to a Rheumatologist is also warranted when one is suspicious for inflammatory arthropathy such as RA. Surgical management may be indicated after conservative measures have failed.Avascular Necrosis (AVN) of the hip is a common reason for joint replacement in the young adult. While most causes of AVN are idiopathic, there is a strong association with prior trauma, alcohol abuse, hemoglobinopathies, steroid use, and anti-retroviral medications. Patients present with insidious onset of pain, but physical exam findings are often normal with maintenance of range of motion. Radiographs are usually normal early in the disease process, but the common final pathway of AVN is decreased blood flow which ultimately leads to bone ischemia and death of the femoral head [29-33]. The characteristic radiographic changes follow a stepwise progression (Figure 8). At first, cystic and sclerotic changes are seen, followed by subchondral collapse, referred to as the crescent sign. As the process progresses, the femoral head becomes flattened and the joint space narrows [19]. Patients with normal radiographs, persistent hip pain, and with significant risk factors for AVN should be evaluated with an MRI. They should be referred early to an Orthopaedic Surgeon for consideration of hip preserving surgical procedures or arthroplasty.
Several other developmental and congenital conditions can result in arthropathy of the hip. Lysosomal storage diseases such as Gaucher’s Disease can result in osteopenia and may lead to AVN of the hip. DDH is the most common orthopaedic disorder of newborns and encompasses a spectrum of disease. If not treated adequately in infancy and childhood, radiographic evidence of arthritis appears early. Patients usually have a shallow or underdeveloped dysplasic acetabulum with superior subluxation or dislocation of the hip (Figure 9). This high hip center can result in increased joint reactive forces across the hip and significant leg length discrepancies as well [34]. Patients with a history of SCFE and multiple epiphyseal dysplasia can also result in early degenerative disease of the hip requiring joint replacement at a young age. Referral to an Orthopaedic Surgeon for surgical options should be considered in all patients with secondary arthritis resulting from a developmental or congenital condition.
Figure 9: AP radiograph of the pelvis in a 54-year-old female with a history of developmental dysplasia of the hip. Note the disruption in Shenton’s line, subluxed hip joint, and high hip center of rotation. Joint spaces are completely obliterated bilaterally.
Conclusion
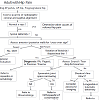
Physicians in many specialties including Internal Medicine, Family Medicine, Rheumatology, Physiatry, and Orthopaedic Surgery will frequently encounter the adult patient with hip pain. Initial radiographic evaluation should include weight bearing AP radiographs of the pelvis and hip, as well as a frog leg lateral view of the affected hip. We recommend a systematic approach to evaluating each radiograph (Figure 10). First, assess the quality of the radiograph and identify the standard radiographic landmarks on each view. Carefully look for any spinal pathology, pelvic obliquity, or leg length discrepancy. Any previous hardware from prior surgical procedures should be noted. Identify any anatomical variations in the acetabulum and/or proximal femur, note the presence and location of any osteophytes, and look for areas of bone loss. A structured review of radiographs provides a reliable diagnostic and clinical decisionmaking process for treatment of osteoarthritis of the hip.References
- Pereira D, Peleteiro B, Araújo J, Branco J, Santos RA, et al. (2011) The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage 19: 1270-1285.
- Lawrence RC, Hochberg MC, Kelsey JL, McDuffie FC, Medsger TA Jr, et al. (1989) Estimates of the prevalence of selected arthritis and musculoskeletal diseases in the United States. J Rheumatol 16: 427-441.
- Hoaglund FT, Shiba R, Newberg AH, Leung KYK (1985) Diseases of the hip: A comparative study of Japanese Oriental and American white patients. J Bone Joint Surg Am 67: 1376-1383.
- Hoaglund FT, Yau AC, Wong WL (1973) Osteoarthritis of the hip and other joints in southern Chinese in Hong Kong. J Bone Joint Surg Am 55: 545-557.
- Lawrence JS and Sebo M (1980) The Geography of Gsteoarthrosis: In, Nuki G (ed): The Aetiopathogenesis of Osteoarthrosis 155-183.
- Dagenais S, Garbedian S, Wai EK (2009) Systematic review of the prevalence of radiographic primary hip osteoarthritis. Clin Orthop Relat Res 467: 623-637.
- Andrianakos AA, Kontelis LK, Karamitsos DG, Aslanidis SI, Georgountzos AI, et al. (2006) Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece. The ESORDIG Study. J Rheumatol 33: 2507-2513.
- Ingvarsson T (2000) Prevalence and inheritance of hip osteoarthritis in Iceland. Acta Orthop Scand Suppl 298: 1-46.
- Campbell SE (2005) Radiography of the Hip: Lines, Signs, and Patterns of Disease. Seminars in Roentgenology 40: 290-319.
- Reijman M, Hazes JM, Pols HA, Bernsen RM, Koes BW, et al. (2005) Role of radiography in predicting progression of osteoarthritis of the hip: prospective cohort study. BMJ 330: 1183.
- Hochberg MC, Lethbridge-Cejku M (1997) Epidemiologic considerations in the primary prevention of osteoarthritis: In, Hamerman D (edn): Osteoarthritis: Public Health Implications for an Aging Population. 169-186.
- Chitnavis J, Sinsheimer JS, Clipsham K, Loughlin J, Sykes B, et al (1997) Genetic influences in endstage osteoarthritis: Sibling risks of hip and knee replacement for idiopathic osteoarthritis. J Bone Joint Surg Br 79: 660-664.
- Spector TD, Cicuttini F, Baker J, Loughlin J, Hart D (1996) Genetic influences on osteoarthritis in women: A twin study. BMJ 312: 940-943.
- Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, et al. (2008) A Systematic Approach to the Plain Radiographic Evaluation of the Young Adult Hip. J Bone Joint Surgery Am 90: 47-66.
- Greenspan A (2000) Lower limb I: pelvic girdle and proximal femur: In, Greenspan A (edn): Orthopedic Radiology: A Practical Approach (edn 3). Philadelphia, PA, Lippincott, Williams, and Wilkins.
- Siebenrock KA, Kalbermatten DF, Ganz R (2003) Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res (407): 241-248.
- Letournel E (1980) Acetabulum fractures: classification and management. Clin Orthop Relat Res 151: 81-106.
- Conrozier T, Tron AM, Mathieu P, Vignon E (1995) Quantitative assessment of radiographic normal and osteoarthritic hip joint space. Osteoarthritis Cartilage 3: 81-87.
- Steinberg ME, Brighton CT, Corces A, Hayken GD, Steinberg DR, et al. (1989) Osteonecrosis of the femoral head; results of core decompression and grafting with electrical stimulation. Clin Orthop Relat Res 249: 199-208.
- Altman R, Alarcón G, Appelrouth D, Bloch D, Borenstein D, et al. (1991) The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 34: 505-514.
- Aebi M (2005) The adult scoliosis. Eur Spine J14: 925-948.
- Jacobson JA, Girish G, Jiang Y, Resnick D (2008) Radiographic evaluation of arthritis: inflammatory conditions. Radiology 248: 378-389.
- Winter RB, Pinto WC (1986) Pelvic obliquity: Its causes and its treatment. Spine 11: 225-234.
- Beck M, Kalhor M, Leunig M, Ganz R (2005) Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 87: 1012-1018.
- Van De Velde S, Fillman R, Yandow S (2006) The aetiology of protrusio acetabuli. Literature review from 1824 to 2006. Acta Orthop Belg 72: 524-529.
- Tannast M, Siebenrock KA, Anderson SE (2007) Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol 188: 1540-1552.
- Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, et al. (2003) Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res 417: 112-120.
- Burgener F, Kormano M, Pudas T. (2006)Bone and Joint Disorders: Differential Diagnosis in Conventional Radiology. New York: Thieme: 131-132.
- Arlet J (1992) Nontraumatic avascular necrosis of the femoral head: past, present, and future. Clin Orthop Relat Res 277: 12-21.
- Mont MA, Hungerford D (1995) Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 77: 459-474.
- Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, et al. (2003) Osteonecrosis of the hip: management in the 21st century. Instr Course Lect 52: 337-355.
- Aaron R (1998) Osteonecrosis: etiology, pathophysiology and diagnosis, in The Adult Hip, Callaghan JJ, Rosenberg AG, and Rubash H, Edns, Lippencott-Raven, Philadelphia, PA, USA.
- Seamon J, Keller T, Saleh J, Cui Q (2012) The Pathogenesis of Nontraumatic Osteonecrosis. Arthritis.
- Bozic KJ, Freiberg AA, Harris WH (2004) The high hip center. Clin Orthop Relat Res 420: 101-105.