Journal of Orthopedics & Rheumatology
Download PDF
Case Report
*Address for Correspondence: Andrew T. Pennock, Department of Orthopedics, Rady Children’s Hospital, 3030 Children’s Way, Suite 410, San Diego, CA 92123, USA, E-mail: apennock@rchsd.org
Citation: Phillips LG, Edmonds EW, Pennock AT. Proximal Tibia Physeal Fracture with Entrapped Medial Collateral Ligament Tear: A Report of 2 Cases and Review of Literature. J Orthopedics Rheumatol. 2013;1(1): 3.
Copyright © 2013 Phillips LG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 1, Issue: 1
Submission: 30 October 2013 | Accepted: 09 November 2013 | Published: 14 November 2013
Reviewed & Approved by: Fawzy A. Saad, Derpartment of Orthopaedic Surgery, Albert Einstein College of Medicine, USA
Proximal Tibia Physeal Fracture with Entrapped Medial Collateral Ligament Tear: A Report of 2 Cases and Review of Literature
Lee G. Phillips, Eric W. Edmonds, Andrew T. Pennock*
- Department of Orthopedics, Rady Children’s Hospital, 3030 Children’s Way, Suite 410, San Diego, CA 92123, USA
*Address for Correspondence: Andrew T. Pennock, Department of Orthopedics, Rady Children’s Hospital, 3030 Children’s Way, Suite 410, San Diego, CA 92123, USA, E-mail: apennock@rchsd.org
Citation: Phillips LG, Edmonds EW, Pennock AT. Proximal Tibia Physeal Fracture with Entrapped Medial Collateral Ligament Tear: A Report of 2 Cases and Review of Literature. J Orthopedics Rheumatol. 2013;1(1): 3.
Copyright © 2013 Phillips LG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Orthopedics & Rheumatology | ISSN: 2334-2846 | Volume: 1, Issue: 1
Submission: 30 October 2013 | Accepted: 09 November 2013 | Published: 14 November 2013
Reviewed & Approved by: Fawzy A. Saad, Derpartment of Orthopaedic Surgery, Albert Einstein College of Medicine, USA
Abstract
Knee injuries are common in young athletes, with the Medial Collateral Ligament (MCL) being the most frequently injured structure. Proximal tibia physeal fractures, on the other hand, are relatively uncommon, comprising less than 1% of all physeal fractures in the skeletally immature [1]. There are few reports discussing soft tissue interposition in physeal fractures about the knee. We present 2 cases of MCL entrapment within a displaced Salter Harris 1 proximal tibia fracture, both of which were treated surgically. One patient subsequently developed a premature physeal closure with an associated leg length discrepancy. We believe these cases should heighten clinician awareness of this injury pattern and emphasize the importance of advanced imaging in the evaluation of skeletally immature patients with significant medial sided knee injuries.Introduction
As the youth population becomes increasingly involved in competitive athletics, knee injuries have become a frequent reason to seek orthopedic care. The MCL is the most common ligament to be injured in the knee, especially with sports like football, soccer, skiing, and ice hockey [2]. The mechanism of injury typically involves a valgus force that stresses the medial sided structures of the knee, including the deep and superficial fibers of the MCL, in addition to the proximal tibial physis and the distal femoral physis. Differentiating an MCL injury from a physeal fracture may be challenging and advanced imaging may be necessary to distinguish these different diagnoses. Clinically, this is relevant because the management of a physeal fracture about the knee may differ from the management of an isolated MCL injury. Combined injuries to both the MCL and the physis are extremely rare, with only a few cases being reported in the literature. The purpose of this report is to present two patients who presented to our clinic with proximal tibia physeal fractures with the superficial MCL entrapped within the fracture site. Our focus is on the clinical, radiographic, and surgical findings of this unique injury pattern, as well as a review of the pertinent literature.Case report 1
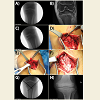
A 13 year-old male patient presented with left knee pain 4 days removed from a football injury. He was struck on the lateral aspect of his left knee, sustaining a valgus force. The patient noted significant swelling but denied feeling a pop, mechanical symptoms, or instability. The patient was treated in a knee immobilizer until presenting to clinic. On exam, he was noted to have significant medial knee pain, swelling, and poor range of motion. Widening was noted on valgus stress testing but further ligamentous examination was limited due to patient pain. Radiographs revealed slight widening of the medial tibial physis and a buckle fracture of the proximal fibular metaphysis (Figure 1A). An MRI was obtained, which revealed a Salter Harris 1 fracture of the proximal tibia with complete avulsion of the superficial fibers of the MCL (Figure 1B). The MCL was reflected proximally and entrapped within the proximal tibial physis. Given this finding, the patient was taken for operative treatment where open reduction was performed. During this procedure, valgus stress allowed the MCL to be extracted and subsequently repaired using a single suture anchor (Figure 1C-F). The physeal fracture was then reduced and stabilized with crossed K-wires (Figure 1G). The patient was placed into a cast for 4 weeks post-operatively until the pins were removed. His post-operative rehabilitation began at the 4 week visit when he was placed into a knee brace and began PT-supervised gentle range of motion (Figure 1H).Figure 1: A) Intra-operative fluoroscopic image showing widening of the medial proximal tibialphysis. B) Pre-operative PD MRI showing Salter Harris 1 fracture of the proximal tibialphysis and tibial avulsion of the superficial MCL with entrapment in the physis. C) Intra-operative fluoroscopic image with valgus stress showing further widening of the medial physis and medial joint opening. D) MCL entrapped in the proximal tibialphysis. E) Torn MCL extracted from the fracture. F) MCL repaired with single suture anchor. G) AP intra-operative fluoroscopic image with crossed K-wires and suture anchor for MCL repair. H) AP radiograph at follow-up..
Case report 2
A 13 year-old male injured his right knee playing football when he was tackled from the side by another player. The helmet struck him on the lateral side of the knee with a valgus force. He had pain and swelling and was initially treated with a knee immobilizer. In clinic, he had medial knee pain, significant swelling, limited motion, and a ligamentous exam that was severely limited due to patient discomfort. Radiographs revealed widening of the medial proximal tibial physis (Figure 2A). An MRI was obtained and showed a Salter Harris 1 fracture of the proximal tibial physis with entrapment of the superficial MCL (Figure 2B).The patient was taken to the operating room for open reduction, removal of the MCL from the physis, and crossed k-wire fixation (Figure 2C). Post-operatively, he was treated in a long leg cast for 3 weeks until the pins were removed. He was then transitioned to a knee brace and physical therapy commenced at the 6 week mark for range of motion.Radiographs obtained at 6 months were concerning for a premature physeal closure and a CT scan was subsequently obtained which confirmed a central physeal closure (Figure 2D). Given his advanced bone age, the decision was made to follow his premature physeal closure clinically. At skeletal maturity his leg length discrepancy measured 1.7 cm,left greater than right, with his tibia shorter by 9mm and his femur shorter by 8mm (Figure 2E). At his 2-year follow-up, the patient remains asymptomatic and has returned to full sport, including football and rugby.
Figure 2: A) Injury AP radiograph showing widening of the medial physis. B) Pre-operative PD MRI showing Salter Harris 1 fracture of the proximal tibialphysis with MCL entrapment in the physis. C) AP intra-operative fluoroscopic image with crossed K-wires. D) CT scan obtained 6 months post-op showing central physeal closure. E) Scanogram for bone length obtained at final follow-up.
Discussion
The two cases presented in this report share many common features both with their presentation and treatment. Both patients were males in their early teenage years injured playing football by a valgus mechanism. They presented to clinic with pain and swelling out of proportion to the typical MCL injury patient. Radiographs revealed widening of the medial proximal tibial physis and MRI confirmed the MCL fibers being interposed within the fracture site. In the operating room, under open direct visualization, it was noted that the MCL was entrapped in the physis. Once this was removed, anatomic reduction was achieved and held with crossed K-wires. While both fractures healed with no evidence of late instability, long-term follow-up on one patient revealed a premature physeal closure. At skeletal maturity, the patient’s leg length discrepancy was less than 2 cm and asymptomatic, so no further treatment was pursued.Previous reports have discussed physeal fracture with interposed soft tissue, usually periosteum. For distal tibia physeal fracture, a residual gap following closed reduction represented interposed periosteum in all cases subsequently treated with open reduction [3]. Whan et al. described the first case in the literature of interposed periosteum in a proximal tibia physeal fracture that was confirmed on pre-operative imaging [4]. The effects of interposed soft tissue within the physis remains controversial as it pertains to possible premature physeal closure.
Two reports in the literature exist of skeletally immature patients with MCL injuries that became entrapped within the peri-articular structures of the knee. Desai et al. presented a 9 year-old boy injured while jumping on a trampoline. His knee exam was notable for valgus instability and his MRI showed that his MCL was entrapped within in the joint beneath the medial meniscus. Open direct repair confirmed these findings and yielded a good outcome [5]. The second case, reported by McAnally et al., describes a 13 year-old male with a valgus injury to the knee. On exam, the patient had valgus laxity and radiographs showed widening of the proximal medial tibial physis. MRI and operative findings confirmed a physeal fracture with torn and interposed medial collateral ligament [6]. When treating a proximal tibia physeal injury, residual gapping at the fracture site after an attempted closed reduction should alert the clinician that interposed periosteum or MCL fibers may be present at the fracture site. We present the cases of two such patients including presentation, imaging, and management.
This injury pattern should be considered in patients with a proximal tibia physeal injury, widening of the medial physis, and valgus instability. MRIs in our two cases were diagnostic for pre-operatively identifying this lesion. If undiagnosed, this injury pattern may be a cause for persistent valgus instability after healing of the physeal fracture. Despite the fact that these injuries were treated with removal of the interposed MCL and anatomic reduction of the fracture, one of our patients developed a premature physeal closure. Appropriate counseling of the patient and family regarding the risk of premature physeal closure is warranted, even if the lesion is appropriately identified and treated. After treatment, serial radiographs should be obtained at 6 and 12 months to assess for evidence of physeal closure. If a premature physeal closure is suspected, a CT scan can be obtained to confirm and localize the closure. For proximal tibia physeal fractures, the reported rates of premature closure range from 10-20% [7]. It is likely the rates are similar, if not higher, for this injury pattern, given the more significant injury to the joint. With the proximal tibial physis contributing approximately 6mm of longitudinal growth per year, aphyseal closure in early adolescence may cause significant leg length discrepancy or angular deformity over time. It is important that this be discussed with the family and followed with serial radiographs.
References
- Edwards PH Jr and Grana WA (1995) Physeal Fractures About the Knee. J Am Acad Orthop Surg 3: 63-69.
- Phisitkul P, James SL, Wolf BR and Amendola A (2006) MCL injuries of the knee: current concepts review. Iowa Orthop J 26: 77-90.
- Barmada A, Gaynor T and Mubarak SJ (2003) Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop 23: 733-739.
- Whan A, Breidahl W and Janes G (2003) MRI of trapped periosteum in a proximal tibial physeal injury of a pediatric patient. AJR Am J Roentgenol 181: 1397-1399.
- Desai R, Parikh S and Laor T (2010) Intra-articular entrapment of the medial collateral ligament. Orthopedics 33: 687.
- McAnally JL, Eberhardt SC, Mlady GW, Fitzpatrick J and Bosch P (2008) Medial collateral ligament tear entrapped within a proximal tibial physeal separation: imaging findings and operative reduction. Skeletal Radiol 37: 943-946.
- Herring J (2002) Lower Extremity Injuries: Proximal Tibial Physis Fractures. Tachdjian’s Pediatric Orthopaedics, Saunders company, Philadephia.