Journal of Obesity and Bariatrics
Download PDF
Research Article
*Address for Correspondence: Sebastian Heinrich, MD, Department of Anesthesia, University Hospital Erlangen, Krankenhausstr 12, 91054 Erlangen, Germany, E-mail: sebastian.heinrich@kfa.imed.uni-erlangen.de
Citation: Heinrich S, Horbach T, Stubner B, Prottengeier J, Irouschek A, et al. Benefits of Heated and Humidified High Flow Nasal Oxygen for Preoxygenation in Morbidly Obese Patients Undergoing Bariatric Surgery: A Randomized Controlled Study. J Obes Bariatrics. 2014;1(1): 7.
Copyright © 2014 Heinrich S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Obesity and Bariatrics | Volume: 1, Issue: 1
Submission: 12 December 2014 | Accepted: 19 December 2014 | Published: 24 December 2014
Methods: 33 morbidly obese patients undergoing laparoscopic bariatric surgery were randomly assigned to receive one of the following preoxygenation procedures for seven minutes: high flow heated humidified nasal oxygen (HFHHNO), continuous positive airway pressure (CPAP) or oxygen insufflation via a face mask (STAND) which is the standard procedure for preoxygenation. Repetitive arterial blood gas analysis at 0, 1, 3, 5, 7 and 8:30 minutes were used to monitor the arterial oxygen partial pressure (PaO2).
Results: From homogenous median PaO2 baseline values (STAND 88 mmHg, CPAP 87 mmHg, HFHHNO 77 mmHg) the PaO2 values of all three groups increased significantly within one minute of preoxygenation. After three minutes of preoxygenation, the STANDgroup reached a median arterial oxygen partial pressure level of 337 mmHg (25% quartile: 295 mmHg/75% quartile: 390 mmHg), the CPAP group of 353 mmHg (293 mmHg/419 mmHg) and the HFHHNO-group of 380 mmHg (339 mmHg/443 mmHg). Irrespective of the preoxygenation method, arterial oxygen partial pressure did not reach significantly higher levels at any time compared with the 3 minute mark.
Conclusions: Standard preoxygenation was inferior in terms of sustained arterial oxygen partial pressure. High flow heated humidified nasal oxygen could provide a rapid, safe and easy to use preoxygenation prior to general anesthesia and arterial oxygen partial pressure might be higher after HFHHNO preoxygenation compared to standard or CPAP breathing.
Keywords: Morbid obesity; Bariatric surgery; Anesthesia for morbidly obese patients; Preoxygenation; CPAP- breathing
STAND-group
Standard preoxygenation was performed by oxygen insufflation via a face mask using the standard anesthesia ventilators of the institutions with 100% oxygen flow of 12 liter/minute. Figure 1a illustrates the setup for standard preoxygenation.CPAP-group
Face mask CPAP ventilation was applied from a mobile intensive care unit ventilator (OxylogTM 3000, Drager® Lubeck, Germany) using a pressure level of 7 cm H2O and a FiO2 of 1.0. Figure 1b illustrates the setup for CPAP breathing. HFHHNO-group
High flow heated (34 °C) and humidified nasal oxygen is given with the OptiFlow System (Fisher & Paykel®, Aukland New Zealand) using a flow of 50 liter/minute and an inspiratory oxygen fraction (FiO2) of 1.0. Patients in our study were asked not to speak during anesthesia induction and keep the mouth closed. Figure 1C illustrates the setup for HFHHNO breathing.At both locations, the study was performed by the same investigators. Preoperative phase
Preoperative anesthesia assessment was provided according to the standard operating procedures (SOP) for bariatric surgery. To assess the risk of difficult airway situations the patients were asked to open their mouth and visibility of the soft palate was scored using the four-scale Mallampati classification. Mallampati 4, as well as a history of difficult airway would have led to exclusion of the study. In line with the existing SOP, benzodiazepines for premedication were avoided. According to the SOP every patient undergoing bariatric surgery is treated like having a sleep apnea syndrome. Testing for sleep apnea syndromes like polysomnography or STOP BANG questionnaire was not part of the clinical routine nor was it part of the study measures. As part of the preoperative study preparation, a spirometric test to assess functional vital capacity (FVC) and the Tiffenau index (FEV1/FVC) was performed using the USB Spirobank (MIR Medical International Research, Waukesha, USA). The results were adjusted to age, height, gender and finally given as relative values to the standard normative values which were stored in the internal database of the spirometer.
Anesthesia induction
Standard monitoring including pulse oximetry (SpO2), 5-lead ECG and non-invasive blood pressure was applied for all patients. In our institution, arterial catheterization before anesthesia induction is part of the standard approach for induction of general anesthesia for bariatric surgery. According to the SOPs, patients were positioned in 30o head up. After local anesthesia, catheterization of a radial artery was performed. Simultaneously to the arterial blood gas samples, the SpO2-values of the patients were recorded. The first arterial blood gas (ABG) analysis and SpO2-value were recorded while the patient was breathing room air. The flow chart of all study measures is shown in Figure 2. 1-2 μg/kg total body weight fentanyl was administered five minutes after starting preoxygenation. After seven minutes of preoxygenation, induction of anesthesia was performed as rapid sequence induction (thiopentone 5 mg -7.5 mg per kg lean body weight; suxamethonium 1 mg per kg total body weight). As the choice of neuro-muscular blocking agent for RSI in overweight patients influences the desaturation [19], suxamethonium was the mandatory agent in this study. In three cases (1x STAND group, 2x CPAP group) specific contraindications of suxamethonium lead to the use of rocuronium.After loss of consciousness the face masks of CPAP and STAND group were removed, whereas the HFHHNO nasal cannula was left in position and the patients of all three groups were intubated. After intubation at 8:30 min the last ABG sample was taken before the mechanical ventilation started.
Statistics
The ABG samples were analyzed immediately with a point of care blood gas analyzer (ABL 800, Radiometer®, Denmark) to avoid any falsification by delayed analyses.Patient data as well as the ABG results were transferred into an Excel (Microsoft® Redmond, USA) database. Statistica (StatSoft® Tulsa, USA) was used for further statistical processing. Statistical testing was performed using Wilcoxon test, Man-Whitney-U test and Chi-square test. Statistical significance level was assumed for p values lower than 0.05. To avoid time series alpha error accumulation by comparing the PaO2 values at different time points, the significance level was corrected with the Bonferroni method to pAhead of starting the study a sample size calculation based on a pilot trial with four patients undergoing standard preoxygenation was performed. The mean PaO2 of these patients with standard preoxygenation was approximately 300 mmHg with a standard deviation of 80 mmHg. To achieve an adequate elongation of safe apnea margin with the two devices a mean PaO2 of 400 mmHg was assumed for the sample size calculation. Given means of PaO2 with 300 and 400 mmHg and a standard deviation of 80 mmHg, an alpha error of 5% and a power of 0.8 the sample size calculation revealed a minimum sample size of 11 patients.
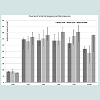
The results of the preoperative spirometry are given in Table 1. The FVC of the STAND group is significantly higher than those of the CPAP group (96% vs. 84%; p=0.03) and by trend higher than the HFHHNO group (96% vs. 83%; not significant). Either the spirometry results of the CPAP and the HFHHNO group nor those of the STAND or the HFHHNO group showed any statistically significant difference.The course of the arterial oxygen partial pressure (PaO2) is shown in Table 2 and Figure 3. In the STAND-group the PaO2 levels increased significantly from 0 min to 1 min (p=0.003). From 1 min to 3 min and from 3 min to 5 min the oxygen partial pressure increased without reaching statistical significance. From 5 min to 7 min and from 7 min to 8:30 min the PaO2 levels decrease significantly. The median saturation of patients in the standard preoxygenation group at 0 min was 98% and increased to 100% after 1 min, 3 min, 5 min and after 7 min of standard preoxygenation. The median saturation after the intubation at 8:30 min was still 100%.PaO2 values of the patients in the CPAP-group showed a significant increase from 0 min to 1 min (p=0.003) and from 1 min to 3 min (p=0.05). From 3 min to 5 min the PaO2 decreases and rises again from 5 min to 7 min but without reaching statistical level respectively. The drop of PaO2 between 7 min and 8:30 min (p=0.004) is statistically significant. The median saturation course in the CPAP group presented as follows: 96 % at 0 min, increase to 100 % after 1 min, 3 min, 5 min, and after 7 min and 99% after the intubation at 8:30 min.The HFHHNO-group showed the following course of PaO2 values: Significant increase from 0 min to 1 min (p=0.003), slight increase from 1 min to 3 min, from 3 min to 5 min and a decrease from 5 min to 7 min and a significant drop from 7 min to 8:30 min (p=0.007). The median oxygen saturation in patients receiving high flow heated humidified nasal oxygen was at the baseline 98%, and after 1 min, 3 min, 5 min and 7 min median pulsoxymetric oxygen saturation was 100% and it was still 100% after the intubation at 8:30 min.In the STAND-group, the PaO2 values reached a peak after one minute of preoxygenation and slightly decreased at the following time points. Whereas the highest PaO2 values of the CPAP-group are reached after seven minutes of preoxygenation, the peak of the HFHHNO-group was at five minutes but with no clinical difference to the seven minutes value.The rise from 1 min to the peak of the PaO2 values did not reach statistically significant levels in any of the preoxygenation groups.Before the preoxygenation procedure, the baseline oxygen levels of the three groups are comparable. The differences between the oxygen partial pressure of the three groups were also not statistically different after one minute of preoxygenation. After 3 min of preoxygenation, the HFHHNO-group has the highest PaO2 value compared with the CPAP-group and the STAND-group, but the p-values are under the preassigned significance level. The superiority of continuous positive airway pressure preoxygenation (CPAPgroup) compared with a standard preoxygenation setting (STANDgroup) did also not reach statistically significant levels after 3 min. After 5 min of preoxygenation patients of the HFHHNO-group had a significant higher PaO2 value compared with the STAND-group (p=0.048). The difference between the HFHHNO-group and the CPAP-group does not reach the preassigned statistical significance level as well as the difference between the CPAP-group and the STAND-group. At 7 min the HFHHNO-group reached significantly increased PaO2 values compared with the STAND-group (p=0.023). The difference between the HFHHNO-group and the CPAP-group is not statistically significant, as well as the difference between CPAPgroup and STAND-group. After 8:30 min patients of the HFHHNOgroup still had an increased PaO2 value compared with the CPAPgroup (p=0.49) and the STAND-group (p=0.25) but the difference was not statistically significant. The difference between CPAP-group and STAND-group is also not statistically significant (p=0.39).Except the basic PaO2 value at 0 min, patients of the HFHHNOgroup had the highest PaO2 values at any time.
Adverse events
During anesthesia induction, no adverse event necessitating study exclusion was reported. The 30o head up position had no effect on the hemodynamics and none of the patients needed vasopressor support during the study phase of preoxygenation and intubation. Prior to the realization of the study, epistaxis was expected to be a possible complication of high flow heated humidified nasal oxygen application. However, epistaxis did not occur during the interventionperiod. Despite regurgitation and aspiration of gastric content is a widely feared but rare complication [20] of face mask- CPAP ventilation, it did not occur in any of the study patients.
Benefits of Heated and Humidified High Flow Nasal Oxygen for Preoxygenation in Morbidly Obese Patients Undergoing Bariatric Surgery: A Randomized Controlled Study
Sebastian Heinrich1*, Thomas Horbach2, Benedikt Stubner1, Johannes Prottengeier1,Andrea Irouschek1 and Joachim Schmidt1
- 11Department of Anesthesia, University Hospital Erlangen, Krankenhausstr, Erlangen, Germany
- 2Surgical Department, Community Hospital Schwabach, Regelsbacher Straße, Schwabach, Germany
*Address for Correspondence: Sebastian Heinrich, MD, Department of Anesthesia, University Hospital Erlangen, Krankenhausstr 12, 91054 Erlangen, Germany, E-mail: sebastian.heinrich@kfa.imed.uni-erlangen.de
Citation: Heinrich S, Horbach T, Stubner B, Prottengeier J, Irouschek A, et al. Benefits of Heated and Humidified High Flow Nasal Oxygen for Preoxygenation in Morbidly Obese Patients Undergoing Bariatric Surgery: A Randomized Controlled Study. J Obes Bariatrics. 2014;1(1): 7.
Copyright © 2014 Heinrich S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Obesity and Bariatrics | Volume: 1, Issue: 1
Submission: 12 December 2014 | Accepted: 19 December 2014 | Published: 24 December 2014
Abstract
Background: Due to loss of functional residual capacity, morbidly obese patients are threatened by hypoxemia during anesthesia induction. To prevent hypoxemia, optimal preoxygenation is mandatory for safe anesthesia induction in morbidly obese patients.The aim of this study was to assess the effect of three different preoxygenation procedures in his patient group. Secondary objective was to investigate, if extension of preoxygenation time from 3 minutes to 5 or 7 minutes leads to increased oxygen partial pressure levels.Methods: 33 morbidly obese patients undergoing laparoscopic bariatric surgery were randomly assigned to receive one of the following preoxygenation procedures for seven minutes: high flow heated humidified nasal oxygen (HFHHNO), continuous positive airway pressure (CPAP) or oxygen insufflation via a face mask (STAND) which is the standard procedure for preoxygenation. Repetitive arterial blood gas analysis at 0, 1, 3, 5, 7 and 8:30 minutes were used to monitor the arterial oxygen partial pressure (PaO2).
Results: From homogenous median PaO2 baseline values (STAND 88 mmHg, CPAP 87 mmHg, HFHHNO 77 mmHg) the PaO2 values of all three groups increased significantly within one minute of preoxygenation. After three minutes of preoxygenation, the STANDgroup reached a median arterial oxygen partial pressure level of 337 mmHg (25% quartile: 295 mmHg/75% quartile: 390 mmHg), the CPAP group of 353 mmHg (293 mmHg/419 mmHg) and the HFHHNO-group of 380 mmHg (339 mmHg/443 mmHg). Irrespective of the preoxygenation method, arterial oxygen partial pressure did not reach significantly higher levels at any time compared with the 3 minute mark.
Conclusions: Standard preoxygenation was inferior in terms of sustained arterial oxygen partial pressure. High flow heated humidified nasal oxygen could provide a rapid, safe and easy to use preoxygenation prior to general anesthesia and arterial oxygen partial pressure might be higher after HFHHNO preoxygenation compared to standard or CPAP breathing.
Keywords: Morbid obesity; Bariatric surgery; Anesthesia for morbidly obese patients; Preoxygenation; CPAP- breathing
Background
World Health Organization estimates that more than 300 million people are affected by the so called “globesity epidemic” [1]. Bariatric surgery is effective to lose weight, improve comorbidities and prevent secondary organ failure [2].Relevant anesthesiological considerations have to be taken into account when performing anesthesia for bariatric surgery. Morbidly obese patients have a reduced functional residual capacity with consecutive increased incidence of atelectasis and ventilation perfusion mismatch leading to hypoxemia by shunting [3-7]. Preoxygenation is of distinguished interest in morbidly obese patients to enhance the safety margin for induction of general anesthesia and placement of the endotracheal tube. To prevent pulmonary aspiration, general anesthesia induction for morbidly obese patients is used to be performed as rapid sequence induction [8]. However there is an ongoing debate if RSI in fastened, elective patients morbid obesity without predictors of difficult airway is justified by the present evidence [9]. Compared to non-obese patients, face mask ventilation and endotracheal intubation are more frequently difficult, time consuming, and establishing an endotracheal airway requires more often fiber optic intubation [7, 9-12]. In this context, an ideal preoxygenation to extend apnea tolerance during anesthesia induction is essential to avoid live threatening airway incidents. Continuous positive airway pressure (CPAP) applied for preoxygenation leads to reduced atelectasis formation and prolonged duration of nonhypoxic apnea in both, obese and non- obese patients by increasing the pulmonary oxygen reserves [13-15]. A precluding factor to use face mask CPAP ventilation for preoxygenation ahead of bariatric surgery could be the close fitting of the CPAP face mask, which is basically necessary and might negatively interfere with preexisting anxiety disorders like claustrophobia occurring in many patients with morbid obesity [16,17].A recent study showed, that nasally given high flow heated and humidified oxygen (HFHHNO) might also provide a CPAP level that is related to the grade of mouth opening [18]. This highly mobile technical solution is easy to use and less unpleasant than face mask CPAP. However HFHHNO has never been studied for preoxygenation purposes in morbidly obese patients. The aim of this study was to assess arterial oxygen partial pressure (PaO2) at defined time points during the preoxygenation in morbidly obese patients, compared between high flow heated humidified nasal oxygen versus preoxygenation with face mask continuous positive airway pressure (CPAP) and standard preoxygenation with oxygen insufflation via face mask (STAND) over at least seven minutes duration in a randomized controlled study. As secondary objective, we addressed the issue whether prolonged preoxygenation of five or seven minutes leads to increased PaO2levels in morbidly obese patients.Patients and Methods
After obtaining institutional research ethics board approval from the University Hospital of Erlangen- Nuremberg and written informed consent, 33 consecutive morbidly obese patients scheduled for laparoscopic bariatric surgery in the University Hospital Erlangen and the associated teaching Community Hospital Schwabach were recruited to the study (identifier: German Clinical Trial Register No.: drks00005475). All study patients were scheduled for elective bariatric surgery which implicates a BMI of at least 35 kg/m² when obesity related comorbidities are preexisting or a BMI of 40 kg/m² when comorbidities are absent.Exclusion criteria were any acquired or congenital severe pulmonary disorder leading to continuous need of supplemental oxygen. Severe psychiatric disorders or language barrier making informed consent impossible or previously confirmed or assumed difficult airway were further exclusion criteria.The patients were randomly assigned to the three preoxygenation groups: standard preoxygenation via a face mask (STAND-group), CPAP preoxygenation (CPAP-group) and high flow heated humidified nasal oxygen (HFHHNO-group). Randomization and assignment to the groups were carried out by the study coordinator using drawing lots.STAND-group
Standard preoxygenation was performed by oxygen insufflation via a face mask using the standard anesthesia ventilators of the institutions with 100% oxygen flow of 12 liter/minute. Figure 1a illustrates the setup for standard preoxygenation.CPAP-group
Face mask CPAP ventilation was applied from a mobile intensive care unit ventilator (OxylogTM 3000, Drager® Lubeck, Germany) using a pressure level of 7 cm H2O and a FiO2 of 1.0. Figure 1b illustrates the setup for CPAP breathing.
High flow heated (34 °C) and humidified nasal oxygen is given with the OptiFlow System (Fisher & Paykel®, Aukland New Zealand) using a flow of 50 liter/minute and an inspiratory oxygen fraction (FiO2) of 1.0. Patients in our study were asked not to speak during anesthesia induction and keep the mouth closed. Figure 1C illustrates the setup for HFHHNO breathing.At both locations, the study was performed by the same investigators.
Preoperative anesthesia assessment was provided according to the standard operating procedures (SOP) for bariatric surgery. To assess the risk of difficult airway situations the patients were asked to open their mouth and visibility of the soft palate was scored using the four-scale Mallampati classification. Mallampati 4, as well as a history of difficult airway would have led to exclusion of the study. In line with the existing SOP, benzodiazepines for premedication were avoided. According to the SOP every patient undergoing bariatric surgery is treated like having a sleep apnea syndrome. Testing for sleep apnea syndromes like polysomnography or STOP BANG questionnaire was not part of the clinical routine nor was it part of the study measures. As part of the preoperative study preparation, a spirometric test to assess functional vital capacity (FVC) and the Tiffenau index (FEV1/FVC) was performed using the USB Spirobank (MIR Medical International Research, Waukesha, USA). The results were adjusted to age, height, gender and finally given as relative values to the standard normative values which were stored in the internal database of the spirometer.
Anesthesia induction
Standard monitoring including pulse oximetry (SpO2), 5-lead ECG and non-invasive blood pressure was applied for all patients. In our institution, arterial catheterization before anesthesia induction is part of the standard approach for induction of general anesthesia for bariatric surgery. According to the SOPs, patients were positioned in 30o head up. After local anesthesia, catheterization of a radial artery was performed. Simultaneously to the arterial blood gas samples, the SpO2-values of the patients were recorded. The first arterial blood gas (ABG) analysis and SpO2-value were recorded while the patient was breathing room air. The flow chart of all study measures is shown in Figure 2.
Statistics
The ABG samples were analyzed immediately with a point of care blood gas analyzer (ABL 800, Radiometer®, Denmark) to avoid any falsification by delayed analyses.Patient data as well as the ABG results were transferred into an Excel (Microsoft® Redmond, USA) database. Statistica (StatSoft® Tulsa, USA) was used for further statistical processing. Statistical testing was performed using Wilcoxon test, Man-Whitney-U test and Chi-square test. Statistical significance level was assumed for p values lower than 0.05. To avoid time series alpha error accumulation by comparing the PaO2 values at different time points, the significance level was corrected with the Bonferroni method to pAhead of starting the study a sample size calculation based on a pilot trial with four patients undergoing standard preoxygenation was performed. The mean PaO2 of these patients with standard preoxygenation was approximately 300 mmHg with a standard deviation of 80 mmHg. To achieve an adequate elongation of safe apnea margin with the two devices a mean PaO2 of 400 mmHg was assumed for the sample size calculation. Given means of PaO2 with 300 and 400 mmHg and a standard deviation of 80 mmHg, an alpha error of 5% and a power of 0.8 the sample size calculation revealed a minimum sample size of 11 patients.
Results
The detailed characteristics of the 33 participants are listed in Table 1. As the CPAP- and the HFHHNO-intervention group had an equal gender distribution (4 female (33%), 7 male (67%)), the STAND-Group included predominately female patients (10 female (91%), 1 male (9%)). This is due to the randomization irrespective of gender. Over all, the study cohort consists of 15 male (45%) and 18 (55%) female patients. BMI was not significantly different between the three groups. ASA physical health status showed no significant differences between the STAND-group: ASA II n=4, ASA III n=7, the CPAP-group: ASA II n=3, ASA III n=8 and the HFHHNO-group: ASA II n=6, ASA III n=5. The visibility of the soft palate of all patients was categorized Mallampati I or Mallampati II.Adverse events
During anesthesia induction, no adverse event necessitating study exclusion was reported. The 30o head up position had no effect on the hemodynamics and none of the patients needed vasopressor support during the study phase of preoxygenation and intubation. Prior to the realization of the study, epistaxis was expected to be a possible complication of high flow heated humidified nasal oxygen application. However, epistaxis did not occur during the interventionperiod. Despite regurgitation and aspiration of gastric content is a widely feared but rare complication [20] of face mask- CPAP ventilation, it did not occur in any of the study patients.
Discussion
The results of this study show that preoxygenation with high flow heated humidified nasal oxygen provides significantly increased arterial oxygen partial pressure levels compared with the standard preoxygenation procedure in morbidly obese patients. To our knowledge, this novel method of preoxygenation and its use in morbidly obese patients has never been reported before. Several methods to improve preoxygenation in morbidly obese patients have been reported through the last years. 25° head up positioning achieves 23% longer sustained arterial oxygen tension level in morbidly obese patients [21]. Laryngeal mask airway prior to laryngoscopic guided intubation showed beneficial effects to overcome the apnea period [22,23]. While the benefits of noninvasive positive airway pressure (CPAP) ventilation in morbidly obese patients are well known [13,14,24,25], there is no widespread use in clinical routine, mainly because a non-invasive ventilation CPAP mode is currently not part of the most standard anesthesia ventilators [26].Our results demonstrate that high flow heated humidified nasal oxygen compared with CPAP could provide comparable or even better oxygen partial pressure levels.Previous studies report of a sustained superiority of face mask CPAP ventilation compared with standard preoxygenation [13]. In our study CPAP preoxygenation showed no statistically significant increase compared to the STAND group.High flow heated humidified nasal oxygen led to a trend providing higher oxygen partial pressure values than CPAP breathing. A possible explanation for this result might be less dead space ventilation of the OptiFlow™ System compared with a facemask CPAP system. However based on our data we could only find that HFHHNO preoxygenation tends to result in higher PaO2 values compared with face-mask CPAP preoxygenation. Irrespective of the preoxygenation mode it is remarkable that arterial oxygen partial pressure is not constantly increasing. In the STAND-group, the PaO2 peak level was even reached after one minute of preoxygenation. The apparent explanation seems to be that early formation of oxygen induced resorption atelectasis [27]. However, recently published studies show, that neither a higher oxygen fraction of inspired oxygen during anesthesia induction nor the oxygen fraction during the mechanical ventilation during the operation has influence on the functional residual capacity of the lung [28,29]. Therefore, there might be a specific explanation related to the patient group characteristics, as a potentially higher susceptibility for atelectasis.After cessation of preoxygenation and endotracheal intubation, sustainment of PaO2-levels in the HFHHNO-group was more prolonged when compared to the CPAP- and the STAND-group. Higher PaO2 levels at 7 minutes in the HFHHNO-group might be causative for this result. In the study setting, all preoxygenation devices were removed after loss of consciousness in all three groups. To take full advantage of the OptiFlow™ system, it is conceivable to leave the system in place during the laryngoscopy for apneic oxygenation. In contrast, face masks for CPAP breathing and oxygen insufflation have to be removed to get access to mouth for endotracheal intubation. Ramachandran and colleagues demonstrated that apneic oxygenation using nasally placed oxygen insufflation catheder results in a significantly longer duration of SpO2 values higher than 95% as well as a higher minimum of SpO2 during prolonged laryngoscopy in morbidly obese patients [30].However, when using the HFHHNO device there is no control of the effectively provided positive airway pressure. This might limit the estimation of the potential for protection of atelectasis as well as the clinical effect. The positive airway pressure with this device highly depended on the cooperation of the patient to close the mouth in an appropriate way.Postoperative hypoxemia due to apnea-hypopnea syndrome is a feared postoperative complication of patients suffering from morbid obesity [31,32]. Compared to CPAP-application, the OptiFlow™ system could easily be used for transfer to the postoperative care unit and during postoperative care without providing an additional ventilator. Postoperative HFHHNO could probably prevent from hypoxemia in patients suffering from apnea-hypopnea syndrome by providing continuous positive airway pressure similar to other CPAP- breathing methods [33].Limitations
Our study has certain limitations. Randomization of our study led to a non-balanced gender distribution especially in the standard group. As there is little knowledge addressing gender differences in preoxygenation of morbidly obese patients no estimation could be made regarding the impact to the results. However preoperative spirometry shows better results in the STAND group (1 male, 10 female patients) which might be caused by the more gluteal fat distribution in female patients. Regarding age, ASA score, BMI and basic oxygen partial pressure value the groups showed no significantdifferences.An investigator controlled assignment of the patients might have resulted in more homogenous patient groups, but bears a latent risk of investigator triggered bias. In favor of avoiding such a bias, the randomized design was chosen, but taking gender imbalance into account. The induction of atelectasis by using a FiO2 of 1.0 is controversially discussed in the literature [27]. Probably the use of FiO2 1.0 in our study might have led to increased formation of resorption atelectasis even in the short preoxygenation time, and the use of a lower FiO2 for example 0.8 might have led to other results. A higher adjusted CPAP level of more than 10 cm H2O in the CPAP group might also have changed the results. However we adjusted the CPAP level at 7 cm H2O cm because the HFHHNO device is reported to achieve CPAP levels of 5-7 cm. In favor of a better comparability between the CPAP and the HFHHNO group and a better tolerance of the face mask by the patients we decided to adjust the CPAP level at 7 cm H2O.Conclusions
However, high flow heated humidified nasal oxygen is a suitable and easy to use method to improve preoxygenation in morbidly obese patients compared with face mask CPAP breathing. The course of PaO2 levels is superior to those of the CPAP- and the STANDgroups during the whole preoxygenation procedure and after the intubation. As the open system of the OptiFlow™ device does not require close fitting CPAP face mask, high flow heated humidified nasal oxygen must not be removed for intubation and might allow apneic preoxygenation during laryngoscopy. In case of regurgitation, the mouth and pharynx is easily accessed.As a main result, in our patient collective, irrespective to the method of preoxygenation, an extended preoxygenation time longer than three minutes did not substantially increase (CPAP and HFHHNO-group) or decreases (STAND) arterial oxygen levels. Taking the results of this study into account, high flow heated humidified nasal oxygen using the OptiFlow™ system presented the highest paO2 values and tended to result in higher PaO2 levels compared with CPAP ventilation.Acknowledgements
The authors gratefully acknowledge funding by the ELAN- Funds of the University of Erlangen- Nuremberg. The valuable support of the anesthesia care teams of the hospitals in Erlangen and in Schwabach is highly appreciated. We acknowledge support by Deutsche Forschungsgemeinschaft and Friedrich-Alexander- Universität Erlangen-Nürnberg within the funding programme Open Access Publishing.p>References
- World Health Organization. Department of Nutrition for Health and Development (2000) Turning the tide of malnutrition: responding to the challenge of the 21st century.
- Christou NV, Sampalis JS, Liberman M, Look D, Auger S, et al. (2004) Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 240: 416-423.
- Jense HG, Dubin SA, Silverstein PI, O'Leary-Escolas U (1991) Effect of obesity on safe duration of apnea in anesthetized humans. Anesth Analg 72: 89-93.
- Guimaraes C, Martins MV, Moutinho Dos Santos J (2012) Pulmonary function tests in obese people candidate to bariatric surgery. Rev Port Pneumol 18: 115-119.
- Domi R, Laho H (2012) Anesthetic challenges in the obese patient. J Anesth 26: 758-765.
- Kira S, Koga H, Yamamoto S, Takeshima N, Hasegawa A, et al. (2007) Anesthetic management of laparoscopic adjustable gastric banding in Japanese patients with morbid obesity. J Anesth 21: 424-428.
- Suzuki A, Terao M, Aizawa K, Sasakawa T, Henderson JJ, et al. (2009) Pentax-AWS airway Scope as an alternative for awake flexible fiberoptic intubation of a morbidly obese patient in the semi-sitting position. J Anesth 23: 162-163.
- Freid EB (2005) The rapid sequence induction revisited: obesity and sleep apnea syndrome. Anesthesiol Clin North America 23: 551-564.
- Kristensen MS (2010) Airway management and morbid obesity. Eur J Anaesthesiol 27: 923-927.
- Williamson JA, Webb RK, Szekely S, Gillies ER, Dreosti AV (1993) The Australian Incident Monitoring Study. Difficult intubation: an analysis of 2000 incident reports. Anaesth Intensive Care 21: 602-607.
- Brodsky JB, Lemmens HJ, Brock-Utne JG, Vierra M, Saidman LJ (2002) Morbid obesity and tracheal intubation. Anesth Analg 94: 732-736.
- Benumof JL (2001) Obstructive sleep apnea in the adult obese patient: implications for airway management. J Clin Anesth 13: 144-156.
- Delay JM, Sebbane M, Jung B, Nocca D, Verzilli D, et al (2008) The effectiveness of noninvasive positive pressure ventilation to enhance preoxygenation in morbidly obese patients: a randomized controlled study. Anesth Analg 107: 1707-1713.
- Futier E, Constantin JM, Pelosi P, Chanques G, Massone A, et al. (2011) Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology 114: 1354-1363.
- Zoremba M, Kalmus G, Begemann D, Eberhart L, Zoremba N, et al. (2011) Short term non-invasive ventilation post-surgery improves arterial blood-gases in obese subjects compared to supplemental oxygen delivery - a randomized controlled trial. BMC Anesthesiol 11:10.
- Martinez EP, Gonzalez ST, Vicente MM, van-der Hofstadt Roman CJ, Rodriguez-Marin J (2012) Psychopathology in a sample of candidate patients for bariatric surgery. Int J Psychiatry Clin Pract 17: 197-205.
- Pervanidou P, Bastaki D, Chouliaras G, Papanikolaou K, Laios E, et al. (2013) Circadian cortisol profiles, anxiety and depressive symptomatology, and body mass index in a clinical population of obese children. Stress 16: 34-43.
- Parke R, McGuinness S, Eccleston M (2009) Nasal high-flow therapy delivers low level positive airway pressure. Br J Anaesth 103: 886-890.
- Tang L, Li S, Huang S, Ma H, Wang Z (2011) Desaturation following rapid sequence induction using succinylcholine vs. rocuronium in overweight patients. Acta Anaesthesiol Scand 55: 203-208.
- Gay PC (2009) Complications of noninvasive ventilation in acute care. Respir Care 54: 246-257.
- Dixon BJ, Dixon JB, Carden JR, Burn AJ, Schachter LM, et al. (2005) Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology 102: 1110-1115.
- Sinha A, Jayaraman L, Punhani D (2013) ProSeal LMA increases safe apnea period in morbidly obese patients undergoing surgery under general anesthesia. Obes Surg 23: 580-584.
- Abdi W, Dhonneur G, Amathieu R, Adhoum A, Kamoun W, et al. (2009) LMA supreme versus facemask ventilation performed by novices: a comparative study in morbidly obese patients showing difficult ventilation predictors. Obes Surg 19: 1624-1630.
- Wong DT, Adly E, Ip HY, Thapar S, Maxted GR, et al. (2011) A comparison between the BoussignacTM continuous positive airway pressure mask and the venturi mask in terms of improvement in the PaO2/F(I)O2 ratio in morbidly obese patients undergoing bariatric surgery: a randomized controlled trial. Can J Anaesth 58: 532-539.
- Coussa M, Proietti S, Schnyder P, Frascarolo P, Suter M, et al. (2004) Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg 98: 1491-1495.
- Jaber S, Tassaux D, Sebbane M, Pouzeratte Y, Battisti A, et al. (2006) Performance characteristics of five new anesthesia ventilators and four intensive care ventilators in pressure-support mode: a comparative bench study. Anesthesiology 105: 944-952.
- Agarwal A, Singh PK, Dhiraj S, Pandey CM, Singh U (2002) Oxygen in air (FiO2 0.4) improves gas exchange in young healthy patients during general anesthesia. Can J Anaesth 49: 1040-1043.
- Staehr AK, Meyhoff CS, Henneberg SW, Christensen PL, Rasmussen LS (2012) Influence of perioperative oxygen fraction on pulmonary function after abdominal surgery: a randomized controlled trial. BMC Res Notes 5: 383.
- Kanaya A, Satoh D, Kurosawa S (2013) Higher fraction of inspired oxygen in anesthesia induction does not affect functional residual capacity reduction after intubation: a comparative study of higher and lower oxygen concentration. J Anesth 27: 385-389.
- Ramachandran SK, Cosnowski A, Shanks A, Turner CR (2010) Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of nasal oxygen administration. J Clin Anesth 22: 164-168.
- Kurrek MM, Cobourn C, Wojtasik Z, Kiss A, Dain SL (2011) Morbidity in patients with or at high risk for obstructive sleep apnea after ambulatory laparoscopic gastric banding. Obes Surg 21: 1494-1498.
- Shimura R, Tatsumi K, Nakamura A, Kasahara Y, Tanabe N, et al. (2005) Fat accumulation, leptin, and hypercapnia in obstructive sleep apnea-hypopnea syndrome. Chest 127: 543-549.
- American Society of Anesthesiologists Task Force on Management of the Difficult Airway (2003) Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 98: 1269-1277.