Journal of Neurology and Psychology
Download PDF
Case Report
*Address for Correspondence: Ghazala Hayat, M.D., FAAN, Department of Neurology & Psychiatry, St. Louis University Health Sciences Center, 1438 S Grand, St. Louis, MO 63104, USA, Tel: 314- 977-4860; Fax: 314- 977-4876; E-mail: hayatm2@slu.edu
Citation: Hayat G, Selhorst JB. Moving Fingers Moving Toes: A Heterogeneous Entity. J Neurol Psychol. 2014;2(1): 5.
Copyright © 2013 Hayat G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Volume: 2, Issue: 1
Submission: 28 February 2014 | Accepted: 19 April 2014 | Published: 24 April 2014
Reviewed & Approved by: Dr. Gang Zhang, Department of Neurology, University of Texas Medical School at Houston, USA
Case 2
Moving Fingers Moving Toes: A Heterogeneous Entity
Ghazala Hayat* and John B Selhorst
- Department of Neurology & Psychiatry, St. Louis University Health Sciences Center, St. Louis, MO, USA
*Address for Correspondence: Ghazala Hayat, M.D., FAAN, Department of Neurology & Psychiatry, St. Louis University Health Sciences Center, 1438 S Grand, St. Louis, MO 63104, USA, Tel: 314- 977-4860; Fax: 314- 977-4876; E-mail: hayatm2@slu.edu
Citation: Hayat G, Selhorst JB. Moving Fingers Moving Toes: A Heterogeneous Entity. J Neurol Psychol. 2014;2(1): 5.
Copyright © 2013 Hayat G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology and Psychology | ISSN: 2332-3469 | Volume: 2, Issue: 1
Submission: 28 February 2014 | Accepted: 19 April 2014 | Published: 24 April 2014
Reviewed & Approved by: Dr. Gang Zhang, Department of Neurology, University of Texas Medical School at Houston, USA
Abstract
Painful legs and moving toes is a rare movement disorder. It can be associated with peripheral neuropathy, trauma, radiculopathy or autonomic disturbances. Variants of the phenomenon involving fingers and arms, with or without pain were described. The electrophysiological studies show several patterns, such as repetitive spontaneous discharges and complex alternating patterns in agonist and antagonist muscles.We describe two patients who presented with progressive, painless, involuntary movements of fingers and toes. The movements were also present during sleep. There was no significant history of trauma or other neurological disease. Myokymic discharges in doublets, triplets and multiplets were seen on electromyography. We postulate that in a subgroup of patients moving fingers and toes is a focal neuromyotonia and autoimmunity may play a role in its pathogenesis.
Keywords
Spinal cord injury; Sleep quality; Pittsburgh Sleep Quality IndexAbbreviations
BMP: Basic Metabolic Panel; CAP: Complex Alternating Pattern; CBC: Complete Blood Count; CT: Computed Tomography; EMG: Electromyography; GABA: Gamma Amino Butyric Acid; MRC: Medical Research Council; MRI: Magnetic Resonance Imaging; NCV: Nerve Conduction Study; PLMT: Painful Legs and Moving Toes; SEP: Simple Erratic Pattern.Introduction
Continuous or semi-continuous movements of toes and finger are a rare disorder which presents with or without pain [1-6]. Painful legs and moving toes (PLMT) was first described in 1971 [1]. It was characterized by semi-rhythmic spontaneous and continuous contractions of the toe flexors, extensors, abductors and adductors. A similar disorder was described in the upper extremities as painful arms and moving fingers [2]. In 1993 a syndrome of painless legs and moving toes was reported [6]. In that particular case there was no history of preceding trauma or peripheral neuropathy; condition usually seen associated with PLMT. With or without associated pain, the electrophysiological studies show different types of repetitive spontaneous discharges and complex alternating patters in agonists and antagonist muscles [4,7].We describe two patients who presented with movements of fingers and toes. They did not present with pain or other associated neurological disorders. The electrodiagnostic studies revealed myokymic discharges in doublets, triplets and multiplets. Myokymic discharges can be seen as a manifestation of neuromyotonia. We postulate that a mechanism similar to neuromyotonia may lead to these discharges. Autoimmunity plays a role in a subgroup of neuromyotonia patients and raises the possibility that immunemodulating therapy could be beneficial.
Case Reports
Case 1A 47-year-old woman presented with a ten-year history of gradual progression of abduction and adduction movements of the left index finger. The movement was constant, including during sleep. There was no associated pain. She was able to suppress the movements voluntarily, only for few seconds. She did not report any history of trauma, weakness or sensory abnormalities in the affected limb. Three years prior to presentation she developed involuntary flexion and extension of the second through fourth toes in the right foot. The movements were also continuous, painless and persistent during sleep. Her past medical history was negative for neurological disorders.
Physical examination: Normal mental status and cranial nerves. Motor strength was 5/5 MRC (Medical Research Council scale) in the upper and lower extremities. Continuous semi rhythmic movements of flexion – extension and abduction – adduction of second through fourth toes in the right foot were noted. There was also adduction – abduction movements of the left index finger. Reflexes were symmetrical, with flexor plantar responses. Sensory examination was normal for pain, touch, temperature and vibratory modalities. Gait and coordination were normal.
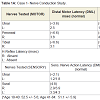
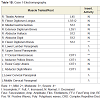
Laboratory investigation: Complete blood count (CBC) and basic metabolic panel (BMP) were within normal limits. Magnetic resonance imaging (MRI) scans of the cervical and lumbosacral spines were normal. Assay for potassium channel antibodies was negative. Nerve conduction velocities (NCV) were normal except for absent bilateral H reflex responses (Table 1A). Electromyography (EMG) showed insertional irritability of the left middle and lower cervical and right lumbosacral paraspinal muscles (Table 1B). The EMG of the left first dorsal interosseus (Figure 1A) and right flexor digitorum brevis (Figure 1B) muscles revealed semi-rhythmic discharges in doublets, triplets and multiplets. The discharge frequency was 3-4 Hz with intraburst frequency ranging between 40-80/second. The amplitude was between 200μV-4mV.
Case 2
A 31 year-old woman presented with a ten-year history of involuntary and continuous movements of her left toes. It began in the second through fourth toes and eventually involved all five. She denied pain, tingling or burning sensation. In addition, she complained of a “dimple” over her left buttock. Her past medical history was unremarkable for trauma or any significant neurological disorders.
Physical examination: Normal mental status and cranial nerves. Motor examination revealed normal tone, bulk and 5/5 (MRC scale) strength in the upper and lower extremities. Reflexes were symmetrical with flexor plantar responses. There was mildly diminished sensation to pin prick over the lateral side of the left leg. A circumscribed 5 cm depression was found over the left buttock. There was no discoloration of the skin or tenderness. There was mild diminished sensation to pin prick, light touch and cold stimuli around the area.
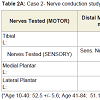
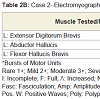
Laboratory investigation: CBC and BMP were normal. Rheumatologic evaluation was negative. The MRI scans of the brain, ankle and foot were normal. The MRI and Computed tomography (CT) myelogram of the lumbosacral spine were unremarkable. The spinal fluid results showed normal cell count and protein levels. The electrophysiological studies revealed normal NCV (Tables 2A and 2B). The EMG was significant for myokymic discharges in multiplets affecting the left extensor digitorum brevis, left abductor hallucis and left flexor hallucis brevis. The discharges fired at a frequency of 2-3 Hz and lasted approximately 200 msecs. The intraburst frequency varied between 70-80/second. The patient did not respond to a trial of carbamazepine and declined further therapy.
Discussion
In 1971, Spillane et al. described six patients with painful legs and moving toes [1]. The symptoms ranged between four and nine years and included severe pain. The movements consisted of slow clawing and straightening, fanning and circular movements of the toes, involving flexion, extension and adduction. Electrophysiological studies were inconclusive. In one patient 8 to 9 repetitive multiplet discharges at a rate of 30/second was noted [1]. Sural nerve biopsy in one patient with pain and spontaneous clawing movements revealed segmental demyelination and short internodal segments [1]. Lumbar sympathetic chain blockade with local anesthetic relieved the pain in four patients.Schott suggested that trauma initiated the syndrome [3]. The severity of trauma varied from minor injury to surgical intervention. He postulated that pain and focal involuntary movements were caused by peripheral nerve injury, but also suggested that subsequently the central nervous system became involved. He proposed that minor peripheral trauma induced a spreading, irritative central discharge, possibly in the lower spinal cord, that variously involved sensory, motor and autonomic fibers.
Montagna et al. described three patients with continuous and involuntary movements of toes with painful legs and clinical evidence of peripheral neuropathy [4]. Electrodiagnostic studies revealed bursts of spontaneous discharges of motor units at a frequency of 0.5 Hz. These bursts were noted to alternate in the extensor digitorum brevis and abductor digiti minimi muscles. The authors also noticed disruption of sleep patterns and some resemblance with the movement disorder restless legs syndrome [4].
In 1993 a patient was described with a painless but otherwise similar involuntary, semi continuous movement of toes for over 33 years [6]. EMG showed disproportion between the time of contraction and relaxation phases.
Schoenen et al. studied six patients and classified them into two groups: The electrophysiological studies in the first group had simple erratic pattern (SEP) consisting of discharges with low amplitude (100μV to 2mV) and frequency of 4-6 Hz [7]. They occurred in erratic fashion, most often synchronously in antagonist muscles. The second group showed complex alternating pattern (CAP), which consisted of alternating bursts of motor activity. The amplitude of the discharges was higher (1 to 3 mV), and the duration longer compared to SEP group. The authors suggested that different mechanisms were involved in painful legs and moving toes. Those patients with SEP represented peripheral pathology with spontaneous activity, myokymia or fasciculations. Patients with CAP had central nervous system disorder as a cause, with EMG findings similar to dyskinesias.
Alvarez et al. reviewed 14 cases out of the database at Mayo Clinic Arizona, from 1996-2006; they found 14 cases of PLMT [8]. The age range was 25-84 years (mean 69 years), 6 men and 8 women. Most of the patients had bilateral movements 12/14. Most of the patients had burning pain prior to abnormal movements and had diagnosis of neuropathy or plexopathy. The electrophysiological studies were indicative of dystonia and chorea [8].
Our patients are similar to those with painful legs and moving toes although neither patient has pain or a history of peripheral nerve injury. The first patient has absent H-reflexes and insertional irritability of cervical and lumbar paraspinal muscles on EMG. That correlates with previous theories of a peripheral nerve disorder as a possible cause. However, the second patient did not show any electrophysiological signs of peripheral nerve disease, which raises the thought of a CNS oscillator. A combination of both mechanisms cannot be excluded. Nevertheless, both our patients had myokymic discharges with a painless movement disorder.
Neuromyotonia, a condition with excess muscle fiber activity usually presents with diffuse involvement and continuous, irregular “worm-like” movements. The pathogenesis of neuromyotonia is not yet established, although autoimmunity is postulated in many cases [9]. This is also seen with exposure to toxins, radiation, paraneoplastic, hereditary, inflammatory neuropathies. On electrophysiological studies, neuromyotonia is characterized by doublet, triplet and multiplet discharges firing irregularly with high intraburst frequency (40-200/second). Newsom-Davis et al. implicated an antibodymediated autoimmune mechanism, affecting the peripheral nerve K+ channels [9]. This leads to interference with the function of K+ channels which normally stabilize the membrane potential and regulates repetitive firing. EMG study in neuromyotonia reveals myokymic discharges, neuromyotonic discharges, fibrillations and fasciculations.
Our two patients with painless moving toes and fingers and three patients described by Schoenen had single motor unit discharges that can be secondary to induction at a peripheral site. The pathophysiological mechanism in the patients is probably peripheral with some suprasegmental and central influence. Verhagen and Horstink suggested that peripheral sensory dysfunction of group II and III afferent fibers interact with supraspinal pathways leading to the syndrome [5]. However, the authors could not rule out segmental discharges of motor neurons. Zielasek et al. have shown neuromyotonic discharges in mice with hereditary myelinopathies [11]. They postulate different sites of involvement on acquired neuromyotonia, i.e. distal motor nerve, nodal, proximal at neuron level or even in the central nervous system. This may explain heterogeneity of electrophysiological presentation in patients with “moving toes and fingers”. Modarres et al. described two patients with isolated finger flexion and neuromyotonic discharges in the EMG [12]. They suggest that the symptom is a form of focal neuromyotonia. Our patients showed EMG pattern of doublets, triplets and multiplets, also seen with neuromyotonia. There was also involvement of more than one limb.
Muscle relaxants, such as baclofen, antiepileptic drugs such as phenytoin, carbamazepine and sodium valproate have been used to treat neuromyotonia effectively. However, our patients did not respond to these therapies favorably. Sympathetic blocks have reduced pain and abnormal movements in some patients. Botulinum toxin A and GABAergic therapy has shown some relief [8,13,14]. Unfortunately, our patients refused further trials.
Varied etiologies at peripheral and central nervous system levels are suggested for moving fingers moving toes disorders. As electrophysiological discharges can be consistent with neuromyotonia in a subset of patients; autoimmunity may play a role in a subgroup of patients with moving fingers moving toes disorder. As this condition is rare, large studies are not possible to elucidate the role of autoimmunity.
References
- Spillane JD, Nathan PW, Kelly RE, Mardsen CD (1971) Painful legs and moving toes. Brain 94: 541-546.
- Funakawa I, Mano Y, Takayanagi T (1987) Painful hand and moving fingers. J Neurol 234: 342-343.
- Schott GD (1981) Painful legs and moving toes: the role of trauma. J Neurol Neurosurg Psychiatry 44: 344-346.
- Montagna P, Cirignotta F, Sacquegna T, Martinelli P, Ambrosetto G, et al. (1983) Painful legs and moving toes associated with polyneuropathy. J Neurol Neurosurg Psychiatry 46: 399-403.
- Verhagen WI, Horstink MW, Notermans SL (1985) Painful arm and moving fingers. J Neurol Neurosurg Psychiatry 48: 384-385.
- Walters AS, Hening WA, Shah SK, Chokroverty S (1993) Painless legs and moving toes: a syndrome related to painful legs and moving toes. Mov Disord 8: 377-379.
- Schoenen J, Gonce M, Delwaide PJ (1984) Painful legs and moving toes: a syndrome with different physiopathologic mechanisms. Neurology 34: 1108-1112.
- Alvarez MV, Driver-Dunckley EE, Caviness JN, Adler CH, Evidente VG (2008) Case series of painful legs and moving toes: Clinical and electrophysiological observations. Mov Disord 23: 2062-2066.
- Newsom-Davis J, Mills KR (1993) Immunological association of acquired neuromyotonia (Isaac’s syndrome). Report of five cases and literature review. Brain 116: 453-469.
- Nathan PW (1978) Painful legs and moving toes, evidence of the site of lesion. J Neuro Neurosurg Psychiatry 41: 934-939.
- Zielasek J, Martini R, Suter U, Toyka K (2000) Neuromyotonia in mice with hereditary myelinopathies. Muscle Nerve 23: 696-701.
- Modarres H, Samuel M, Schon F (2000) Isolated finger flexion: a novel form of focal neuromyotonia. J Neurol Neurosurg Psychiatry 69: 110-113.
- Singer C, Papapetropoulos S (2007) A case of painless arms/moving fingers responsive to botulinum toxin A injections. Parkinsonism Relat Disord 13: 55-56.
- Papapetropoulos S, Argyriou AA (2008) Painful limbs/moving extremities. Acta Neurol Scand 117: 224-230.