Journal of Nutrition & Health
Download PDF
Research Article
Obesity, Metabolic Syndromeand Related Risk Behaviorsamong Thai Medical Students of Thammasat University
Patcharapa Thaweekul* and Paskorn Sritipsukho
- 1Department of Pediatrics, Faculty of Medicine, Thammasat University, Pathumthani, Thailand
*Address for Correspondence: Patcharapa Thaweekul, Department of Pediatrics, Faculty of Medicine, Thammasat University, 95 Paholyothin Road, Klong-luang, PathumThani 12120, Thailand, Tel: (+6681) 583-6848, (+662) 926-9514; Fax: (+662) 926-9513; E-mail: maybemay@yahoo.com; thaweekul@gmail.com
Citation: Thaweekul P, Sritipsukho P. Obesity, Metabolic Syndrome and Related Risk Behaviors among Thai Medical Students of Thammasat University. J Nutri Health. 2017;3(1): 5.
Copyright © 2017 Thaweekul P et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Nutrition and Health | ISSN: 2469-4185 | Volume: 3, Issue: 1
Submission: 14 March, 2017 | Accepted: 15 April, 2017 | Published: 25 April, 2017
Introduction
Obesity and metabolic syndrome are the major health problems among children, adolescents and adults all over the world. According to the World Health Organization (WHO) report in 2008, more than one third of adults (35%) were overweight (BMI ≥25 kg/m2). The worldwide prevalence of obesity has nearly doubled between 1980 and 2008 [1]. In Thailand, the prevalence of obesity in adulthood is increasing from 13.0% in men and 23.2% in women in 1991 to 22.4% and 34.3% in 2004 respectively [2]. The increasing prevalence of obesity is related to the increase of metabolic syndrome, a cluster of central obesity, insulin resistance, hypertension and dyslipidemia. Metabolic syndrome is a known risk factor for the cardiovascular disease and diabetes in the adolescents and adults.
Adolescent obesity is a strong precursor of obesity and related morbidity in adulthood [3,4]. The previous study during transitional period from the adolescence to young adulthood revealed that young adults gain weight faster than other period of adulthoods [5]. The transition to college of adolescents is an important period of risk for being overweight [6]. Various lifestyles of the college students areimportant risk factors of developing obesity and related metabolic diseases [7,8]. Instead of being the future healthcare professional, the medical students have many risk behaviors of developing obesity during the long period of the 6-year medical curriculum. The inappropriate food consumption, abnormal eating habits, lack of sleep and exercise were identified to be the vulnerable factors to develop obesity among them [9,10].
To the best of our knowledge, no studies demonstrated the alteration of nutritional status during the training in medical program. The present study was conducted to determine the prevalence and risk behaviors of obesity and related metabolic disorders among the final-year medical students of Thammasat University. The change in nutritional status during the studying program was also focused.
Materials and Methods
This institution-based, cross-sectional study was conducted among the sixth-year medical students of Thammasat University during the academic year 2014. The Ethic Committee of Thammasat University approved the protocol. Written informed consent was obtained from all participants.
The voluntary medical students were asked to complete the self-report questionnaires. The questionnaires contained the demographic data (such as the student ID, sex and birth date) and various metabolic risk behaviors including fast food and beverages consumption, fruit and vegetable intake, breakfast skipping, night eating, snacks, exercise, screen time and sleep duration. The weight, height and waist circumference were obtained. Three systolic and diastolic blood pressures were measured after 5-minutes rest. Blood samples were taken after an overnight, 12-hour fast to measure lipid profile (total cholesterol, high-density lipoprotein [HDL-C], lowdensity lipoprotein cholesterol [LDL-C] and triglycerides [TG]) by the enzymatic methods. Fasting plasma glucose (FPG) was measured by hexokinase method. The body weight and height of the medicalstudents in the first year were collected from the medical report at the entry.
The body mass index (BMI) is defined as the weight in kilograms divided by the square of the height in meters (kg/m2). According to WHO cut-off points for Asian, the medical students with overweight and obesity were divided into 3 groups based on their BMI: overweight, 23-24.9 kg/m2; obesity grade I, 25-29.9 kg/m2; obesity grade II ≥30 kg/m2 [11]. Normal weight students defined as BMI 17-22.9 kg/m2. The participants with the BMI less than 17 kg/m2 were defined as underweight. Abdominal obesity was diagnosed in the participants who had the waist circumference more than 80 cm in females or 90 cm in males [12]. Abnormal metabolic parameters were defined according to the International Diabetes Federation (IDF) consensus definition of the metabolic syndrome as follows: triglycerides > 150 mg/dL; HDL-C< 50 mg/dL in females or < 40 in males and FPG > 100 mg/dL [12]. According to the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), the abnormal blood cholesterol was determined as borderline high or high when the total cholesterol was 200-239 mg/dL and ≥240 mg/dL, respectively. The LDL-C was determined as borderline high or high when the LDL-C was 130-159 mg/dL and ≥160 mg/dL, respectively [13]. Hypertension was defined as the systolic and diastolic blood pressure ≥130 and 85 mmHg, respectively [12].
According to IDF consensus, the students were defined to have the metabolic syndrome when central obesity presented plus any two of the four additional factors. These four factors are: 1) raised TG level: ≥150 mg/ dL; 2) reduced HDL-C: 40 mg/dL in males and 50 mg/dL in females; 3) raised blood pressure (systolic BP ≥130 or diastolic BP ≥85 mmHg or treatment of previously diagnosed hypertension; 4) raised FPG ≥100 mg/dL or previously diagnosed type 2 diabetes [12].
Statistical analysis
Demographic and biochemical data were report as means ± SD, unless indicated otherwise. The prevalence of the abnormal metabolic profiles and the presence of the risk behaviors were reported as number (percent). The student t-test or Analysis of Variance (ANOVA) was used to test for the differences in the physical characteristics and biochemical parameters among the medical students with overweight/obesity; normal weight and/or underweight. The presence of various risk behaviors among both groups were compared using Chi-square test. P-value < 0.05 is considered to be significant.
Results
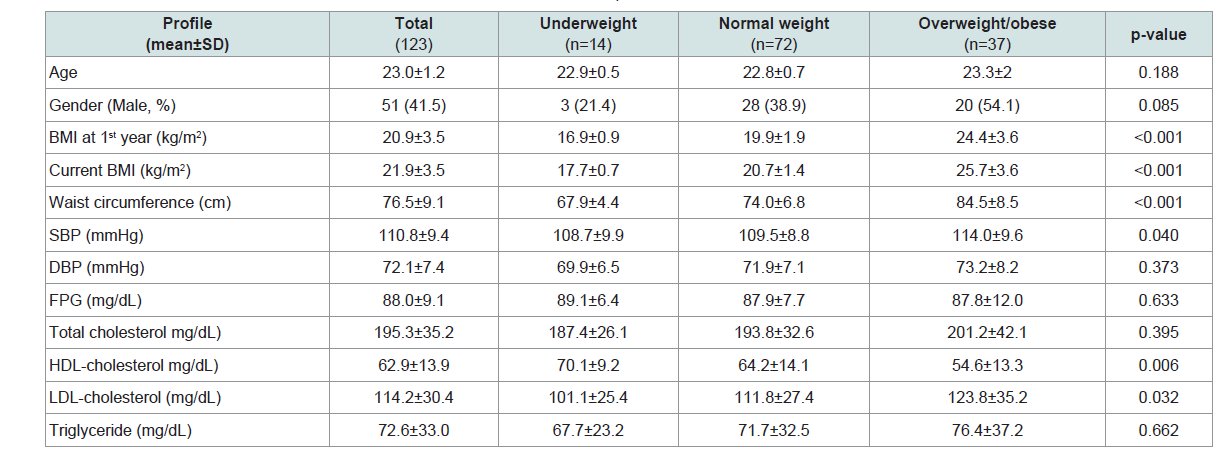
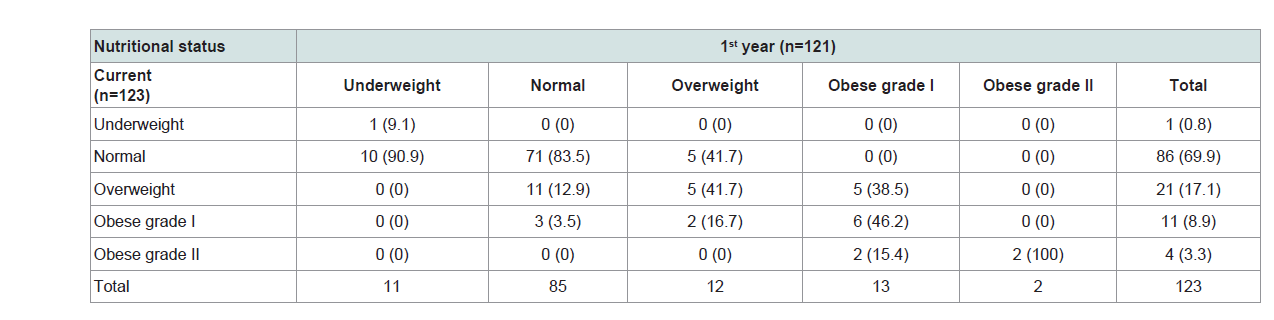
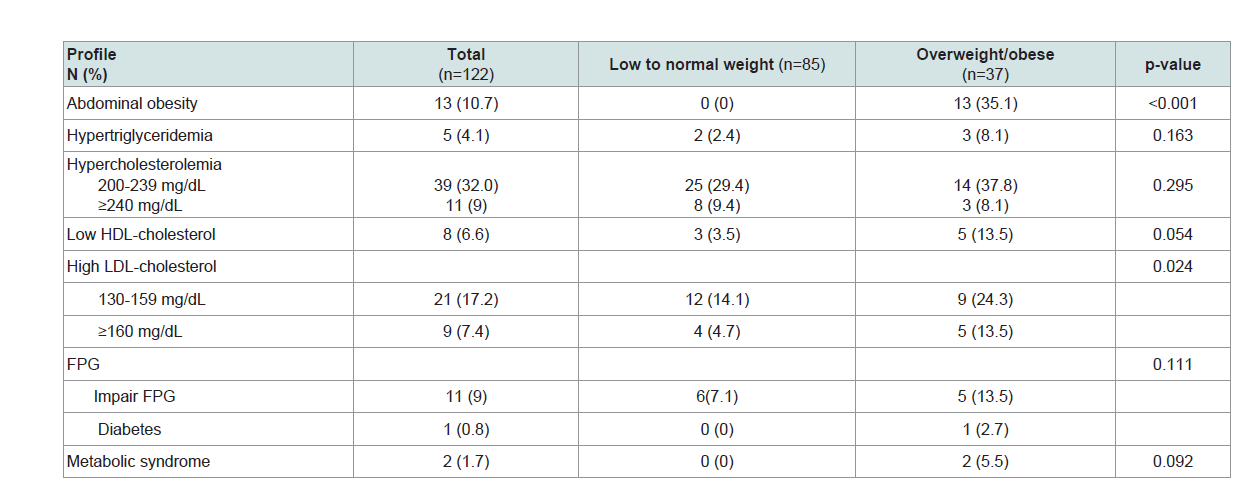
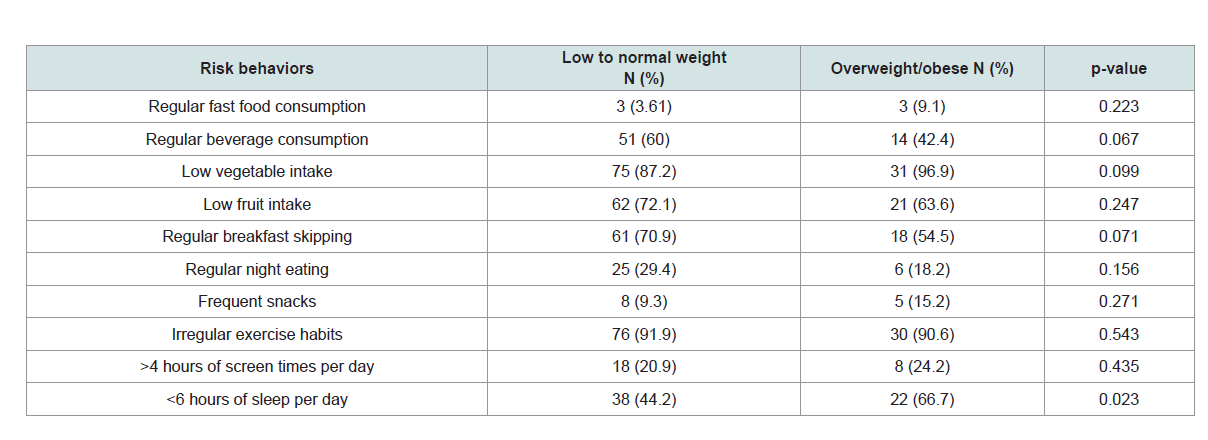
One hundred and twenty-three participants completed the questionnaires and were enrolled in the study. The demographic data of the students with underweight, normal weight and overweight/obesity are shown in Table 1. The mean BMI of the medical students in the first and the final year were 20.9±3.5 and 21.9±3.5 kg/m2, respectively. There are statistically significant differences in waist circumference, systolic blood pressure, HDL-C and LDL-C levels among the three groups. The prevalence of overweight and obesity at the entry to medical school was 22.0% and increased to 29.3% in the final year. Contrary, the prevalence of underweight among the medical students decreased from 8.9% in the first year to 0.8% in the final year. The nutritional statuses among the medical students in the first and final year are shown in Table 3. The current BMI was significantly correlated with the BMI at the entry as shown in Figure 1 (R2 = 0.72, p< 0. 001). The prevalence of abnormal metabolic factors in the students with overweight/obesity tended to be higher than the normal weight and underweight group, with statistically significance in only the serum LDL-C, as shown in Table 3. There were two students diagnosed as metabolic syndrome, according to IDF criteria. Sleep deprivation was significantly frequent in the medical students with overweight/obesity as compared to the normal weight students. The risk behaviors of the students with normal weight and overweight/obesity are shown in Table 4.
Table 2: Nutritional status of the medical students according to the nutritional status during the first year.
Table 3: The prevalence of abnormal metabolic profiles between the low to normal weight and the overweight/obese students.
Discussion
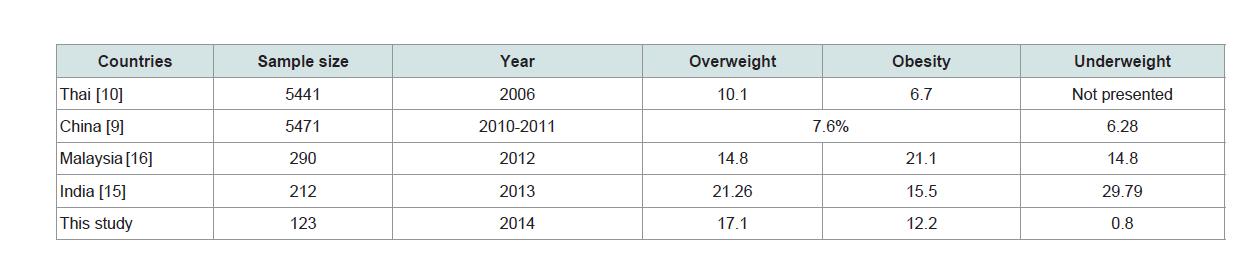
The college students are in the important period for the detection, prevention and intervention of obesity and related metabolic disorder. The medical students, despite being health educated, have many metabolic-risk lifestyles predisposing to adolescent obesity. The prevalence of overweight and obesity in this present study were 17.1% and 12.2%, respectively, which was slightly lower than overall rate of overweight/obesity of the general Thai population. As compared to the Fifth Thai National Nutrition Survey in the year 2003, the prevalence of overweight and obesity in the young adults were 13.9% and 21.7%, respectively [14]. A National survey of 5441 Thai Medical students in the year 2006 reported the prevalence rate of 10.1 and 6.7% which were much lower than the general Thai population and this present study [10]. The prevalence of overweight and obesity among the Asian medical students as compared to their general populations are inconsistent. There are some studies reports the higher prevalence of overweight and obesity among the medical students in India [15] and Malaysia [16]. The lower prevalence is reported from the medical students in China and Thailand including from this present study. The comparative data of the prevalence rate of overweight/obesity among the Asian medical students are shown in Table 5.
Table 5: The comparative data of prevalence rate of overweight/obesity among the Asian medical students.
As tracking the bodyweight from the entry of the medical school to the final year, the prevalence of overweight increased from 9.8% to 17.1%. The prevalence of obesity in the final year students was nearly the same as in the first year. The BMI in the final year was correlated with the BMI at the entry. More than half of the students with overweight and all of the students with obesity since the first year were still overweight or obese at the final year. The BMI increased more significant in male medical students as compared to female students (1.76±1.74 and 0.43±1.82 kg/m2, respectively; p <0.001). The prevalence of overweight and obesity was also reported to be higher in male than female students in many previous studies [9,17-19]. The more increasing BMI among the male students may be due to the fact that the female students are more likely to perceive themselves as overweight and more often try to control or lose their weights [20]. The prevalence of malnutrition in medical students was also decreased rom 8.9% in first year to 0.8% in the final year. This corresponded with the increasing prevalence of overweight in the students in thefinal year.
Metabolic syndrome was diagnosed in two female students and none of the males. The prevalence of metabolic syndrome among the students with overweight/obesity from this present study was 14.29%. Many abnormal metabolic parameters, which are atherosclerotic and cardiovascular risks, were identified among all student groups, even in the students with underweight. The prevalence of high LDL-C in the students with overweight/obesity was significantly higher than the students who had low/normal weight. Metabolic parameters should be done especially in the medicals students with overweight/obesity to early identify the cardiovascular risk in this population.
Of all the life-style factors, sleep deprivation was more frequent behavior in the students with overweight/obesity when compared to the normal weight students. Previous studies reported that students who have fewer hours of sleep were significantly more likely to be overweight or obese [9,21]. This strong association may be due to the increase in ghrelin and decrease in leptin levels [22]. This present study could not demonstrate the difference of other risk behaviors among the low to normal weight and the overweight/obese students. This may due to small sample size in this study. However, more than half of the medical students have various metabolic-risk behaviors such as unhealthy eating habits: breakfast skipping, low fruits and vegetable consumption; limit exercise and sleep deprivation.
Conclusion
As the trend toward of becoming overweight during the final year of the medical students, they should be annually assessed for their nutritional status and evaluated their metabolic parameters, especially the students with overweight/obesity. Lifestyle modification should be advised to the students who are overweight/obese at the entry to decrease their body weights. Male students have higher risk of increase their BMI and should be closely monitored. Medical schools should promote healthy behavior to increase the healthy eating and exercise habits and reduce the risk behaviors among them.
References
- WHO (2008) Global health observatory (GHO) data: Obesity. World Health Organization.
- Aekplakorn W, Mo-Suwan L (2009) Prevalence of obesity in Thailand. Obes Rev 10: 589-592.
- Magarey AM, Daniels LA, Boulton TJ, Cockington RA (2003) Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes Relat Metab Disord 27: 505-513.
- Toschke AM, Rückinger S, Reinehr T, von Kries R (2008) Growth around puberty as predictor of adult obesity. Eur J Clin Nutr 62: 1405-1411.
- Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM (2004) Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr 80: 569-575.
- Vella-Zarb RA, Elgar FJ (2009) The 'freshman 5': a meta-analysis of weight gain in the freshman year of college. J Am Coll Health 58: 161-166.
- Spencer L (2002) Results of a heart disease risk-factor screening among traditional college students. J Am Coll Health 50: 291-296.
- Desai MN, Miller WC, Staples B, Bravender T (2008) Risk factors associated with overweight and obesity in college students. J Am Coll Health 57: 109-114.
- Chen J, Yi H, Liu Z, Fan Y, Bian J, et al. (2013) Factors associated with being overweight among Inner Mongolia medical students in China. BMJ Open 3: e003900.
- Ekpanyaskul C, Sithisarankul P, Wattanasirichaigoon S (2013) Overweight/Obesity and related factors among thai medical students. Asia Pac J Public Health 25: 170-180.
- World Health Organization Regional Office for the Western Pacific, International Diabetes Institute, International Association for the Study of Obesity, International Obesity Task Force (2000) The Asia-Pacific perspective: redefining obesity and its treatment. Health Communication Australia, Sydney.
- Alberti KG, Zimmet P, Shaw J (2006) Metabolic syndrome--a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 23: 469-480.
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2001) Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 285: 2486-2497.
- Department of Health, Ministry of Public Health (2003) Report on the 5th Thai national Nutrition Survey. Ministry of Public Health, Nonthaburi, Thailand.
- Sharma S, Raina SK, Bhardwaj AK, Chander V, Kumar D, et al. (2013) Utility of consensus statement in assessment of obesity: a study among undergraduate medical students from rural Northwest India. J Fam Med Prim Care 2: 274-276.
- Gopalakrishnan S, Ganeshkumar P, Prakash MV, Christopher, Amalraj V (2012) Prevalence of overweight/obesity among the medical students, Malaysia. Med J Malaysia 67: 442-444.
- Kamien M, Power R (1996) Lifestyle and health habits of fourth year medical students at the University of Western Australia. Aust Fam Physician Suppl 1: S26-S29.
- Nisar N, Qadri MH, Fatima K, Perveen S (2008) Dietary habits and life style among the students of a private medical university Karachi. J Pak Med Assoc 59: 98-101.
- Carter AO, Elzubeir M, Abdulrazzaq YM, Revel AD, Townsend A (2003) Health and lifestyle needs assessment of medical students in the United Arab Emirates. Med Teach 25: 492-496.
- Ackard DM, Peterson CB (2001) Association between puberty and disordered eating, body image, and other psychological variables. Int J Eat Disord 29: 187-194.
- Noland H, Price JH, Dake J, Telljohann SK (2009) Adolescents' sleep behaviors and perceptions of sleep. J Sch Health 79: 224-230.
- Taheri S, Lin L, Austin D, Young T, Mignot E (2004) Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 1: e62.