Journal of Geriatrics and Palliative Care
Download PDF
Research Article
*Address for Correspondence: Danforn Lim,PO Box 3256, Blakehurst, NSW 2221 Australia, E-mail: celim@unswalumni.com
Citation: Ho K, Lim CED, Cheng NCL, Zaslawski C. ACEPAC Study - Australian Chinese patient’s Experiences of Palliative Care Services. J Geriatrics Palliative Care 2014;2(2): 8.
Copyright © 2014 Danforn Lim et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN: 2373-1133 | Volume: 2, Issue: 2
Submission: 01 April 2014| Accepted: 23 June 2014 | Published: 26 June 2014
Reviewed & Approved by: Dr. Tamas Fulop, Professor of Medicine and Geriatrics and Senior Researcher at University of Sherbrooke, Quebec, Canada
Attitudes and experiences in pain and opioids prescription
Attitudes and experiences in opioid rotation and tolerance
What Do The Junior Doctors Know About Pain Management And Opioids Use? : An Australian Study
Suyi Siow1, Chi Eung Danforn Lim1,2*, Nga Chong Lisa Cheng2, Christopher Zaslawski2, Jennifer Wiltshire3 and Rebecca Strutt3
- 1 South Western Sydney Clinical School, University of New SouthWales Australia
- 2 School of Medical and Molecular Biosciences, University ofTechnology Sydney, Sydney Australia
- 3Department of Palliative Medicine, Liverpool Hospital, SydneyAustralia
*Address for Correspondence: Danforn Lim,PO Box 3256, Blakehurst, NSW 2221 Australia, E-mail: celim@unswalumni.com
Citation: Ho K, Lim CED, Cheng NCL, Zaslawski C. ACEPAC Study - Australian Chinese patient’s Experiences of Palliative Care Services. J Geriatrics Palliative Care 2014;2(2): 8.
Copyright © 2014 Danforn Lim et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Geriatrics and Palliative Care | ISSN: 2373-1133 | Volume: 2, Issue: 2
Submission: 01 April 2014| Accepted: 23 June 2014 | Published: 26 June 2014
Reviewed & Approved by: Dr. Tamas Fulop, Professor of Medicine and Geriatrics and Senior Researcher at University of Sherbrooke, Quebec, Canada
Abstract
Background: Pain continues to remain an issue in the general population even though studies have demonstrated that adequate pain management is possible with the use of opioids. This could be related to unwarranted opiophobia among patients and healthcare professionals, which hampers administration of opioids for effective pain relief. The purpose of this study is to investigate the knowledge of Australian junior doctors concerning pain management and opioid use.Methods: A questionnaire study was carried out over a total of 32 medical interns and residents. Statistical analysis was conducted to test for significance of data.
Results: Overall, Australian junior doctors were equipped with basic knowledge to effective pain management e.g. that opioids are not exclusive to use in cancer patients (100.0%); analgesics and opioids can be combined in the treatment of pain (96.8%); in the management of pain it is important to differentiate between nociceptive and neuropathic pain (93.8%). Also, 93.8% of respondents agree that they always take a comprehensive pain history, 62.5% find providing good pain control complex and 56.3% find patients’ fear of addiction a barrier to effective use of opioids in practice. More than half of the junior doctors expressed interest in additional education related to pain management and the most popular subject indicated was opioid rotation (86.4%).
Conclusion: Although basic knowledge amongst junior doctors was sufficient, there are several key areas that could be improved on. These include combination of opioid drugs in pain management, opioid rotation, dosage calculation and the fear to start opioid administration. A properly designed education plan should have been developed by the teaching hospitals to ensure a systematic transfer of pain management knowledge to junior doctors.
Keywords
Pain management; Opioid; Knowledge; Junior doctorIntroduction
Pain is a multidimensional and complex response to cellular damage. Perception of pain is influenced by many factors, such as age, culture, past experience and mental state, rendering it difficult to be measured objectively. Patients’ self-report on pain and their manifested behaviour is believed to be the best assessment method [1]. In Australia, one in five people of all ages were found to live with chronic pain. In people above 65 years old, the prevalence is one in three [2]. Among cancer patients, onethird would have already experienced pain prior to diagnosis and the percentage increases to 65-85% as the cancer progresses [3].In order to regulate the standard of pain management, the analgesic ladder was developed in 1986 by the World Health Organization (WHO) [3]. In Australia, the National Health and Medical Research Council (NHMRC) has taken similar steps by setting clinical guidelines for acute pain management. A National Pain Strategy targeting patients suffering from acute, chronic and cancer pain was implemented to facilitate a proper pain management network across the Australian healthcare system [4,5].
However, there is still evidence of the inadequate treatment of pain. Half of the patients continue to be found to be under-treated despite the fact that adequate pain relief has been demonstrated to be possible among no less than 70% of patients [3,6-8]. Such findings generate considerable concern because clinical studies have shown that consequences of inadequate pain relief are detrimental to the physical condition, emotional status and social interaction of patients [7].
The continuing existence of under-treatment of pain can be due to the negative perceptions concerning pain treatments among patients. Examples are myths of opioid addiction, the side effects of medication and the reluctance to report pain unless the pain was intolerable [3,6,9-11]. In addition to that, other studies suggest that professional beliefs and attitudes to pain management might be another issue underpinning the current problem. Some studies suggested that certain doctors are reluctant to prescribe opioids or even if they do, they fail to foresee potential side effects or provide adequate dosage [6,11-13]. Subsequent findings also revealed that there are certain myths and beliefs held collectively by doctors and persist despite being scientifically invalidated. Examples of such are that: pain is inevitable and should be tolerated; opioid, instead of barbiturates, is choice for palliative sedation; increasing opioids accelerates death; side effects of opioids such as nausea and drowsiness are unavoidable [6,11-14]. Such poor pain management practices reflect a lack of knowledge about opioid pharmacology, basic pain assessment skills and an unnecessary fear of addiction among practitioners albeit the availability of evidence-based guidelines on pain relief [6,7,14-21]. This gap in knowledge stems from an inadequate emphasis on pain management during undergraduate and postgraduate training [7,19,22-24]. An American study demonstrated that a mandatory palliative care rotation has improved the skills of residents in assessing and managing pain symptoms (range in improvement from 26% to 67%, p < 0.05) because sufficient time was set aside to acquire and reinforce clinical skills [25]. This observation may substantiate the move to change the current residency training system in Australia whereby palliative care rotation is elective and not compulsory. This is to ensure that junior doctors are given proper guidance and clinical opportunities to effective pain management.
In Australia, there are specialist palliative care services addressing the problem of both acute and chronic pain covering most regions [26]. However, there is still a shortage of specialists in pain management thus requiring general practitioners (GPs), the primary carers of the Australian population, to shoulder the load. Unfortunately, despite the significant role that GPs ought to play in pain relief, many continue to express a disinclination to care for patients who are in pain due to lack of confidence and experiences in managing pain. The consequence of such attitudes can be drastic as pain is commonly manifested among patients who are terminally ill and they would prefer GPs to take care of them at home [16,23,26-28]. Therefore it is imminent to educate junior doctors in terms of both knowledge and having the right attitudes to serve a growing population greatly in need of pain relief as they may venture in future general practice.
The primary objective of this study was to identify the level of proficiency of Australian junior doctors on opioid pharmacology, calculation, tolerance and addiction. The knowledge tested includes basic opioid understanding that should be familiar to all doctors. The gaps in their knowledge are also addressed. The secondary objective was to highlight the need of a compulsory palliative care term through comparing the level of knowledge between participants who have undergone haematology and oncology or palliative training postings and those who have not undergone these postings.
Methods
RecruitmentEthics approval was obtained from the University of New South Wales Human Research Ethics Committee and South Western Sydney Human Research Ethics Committee. A crosssectional survey was then conducted in Liverpool Hospital, South Western Sydney in October 2012. Participants recruited were medical interns and residents in the hospital. Informed consent was obtained before the commencement of the study. A questionnaire was given to them and collected upon completion. An online survey form was also emailed to potential subjects. All participants’ information was kept confidential and de-identified. Non-responders were given at least 2 phone call reminders. A total of 40 survey forms were handed out to medical interns and residents and 32 of them completed the questionnaire.
Survey
The questionnaire was adapted from a published study from a Dutch research group after consent was obtained from the authors14. The questionnaire was then modified to suit the Australian context particularly removing questions about shortening of life, as euthanasia is illegal in Australia. There are mainly 3 types of questions in the questionnaire: knowledge statements with two options “true” and “false”, attitude statements with five options “ completely disagree”, “disagree more than agree”, “neutral”, “agree more than disagree” and “completely agree”, experience and opinion statements with four options “never”, “seldom”, “sometimes”, and “often”. Participants were also required to fill in their background details and grade their knowledge about pain management on a scale of 1-10 prior to and after completing the survey.
Analysis
All completed questionnaires were analysed using SPSS version 20.0. Differences in answers between those who have undergone haematology and oncology or palliative training and those who have not were calculated using Pearson’s chi-square test with a significance level of p<0.05. Fisher’s exact test was applied when the sizes of cell are less than five. Also, the mean score between the two groups were compared using a nonparametric Mann-Whitney U test. A Cronbach’s lpha test was conducted to measure the overall reliability of the questionnaire. The option “don’t know” in the knowledge statement category was considered as having answered the question wrongly. The option “fully agree” was merged into the category “agree” when analysing the attitudes of physicians to pain and when prescribing opioids. The correlation between the self-graded score after completing the questionnaire and whether the responder has undergone postings was calculated.
Results
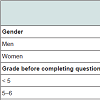
Background characteristicsThe background characteristics of participants are presented in Table 1. Doctors who have undergone haematology and oncology or palliative care postings graded themselves higher in both settings-prior to and after completion of questionnaire. Overall, both groups graded their knowledge on opioids and pain management lower at the end of the survey with more significant decrease in the group who did not go through the postings. The self-graded knowledge scale had a high reliability, Cronbach’s alpha = 0.93. The relationship between whether one has undergone postings and perceived knowledge upon completion of survey was investigated using Pearson product-moment correlation coefficient.
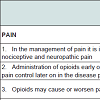
The responses of doctors to the knowledge statements are summarised in Table 2. The questions asked are listed with the correct answer bolded. A Mann-Whitney U Test was conducted. The numbers of correct answers scored were higher among participants who have undergone haematology and oncology or palliative training postings (Median = 7.29) than those who have not undergone any postings (Median = 5.50), U = 58.50, z = -2.14, p<0.05 and it represents a medium-sized effect r = 0.38. The questions which most respondents answered incorrectly are “Opioids may cause or worsen pain” with 34.3% correct answers, “life threatening respiratory depression is a real danger when titrating morphine against pain” with 18.7% correct answers, “simultaneous prescription of a weak opioid and a strong opioid is contraindicated” with 15.6% correct answers, and “drug management of nausea in treatment with opioids is evidencebased” with 3.1% correct answers.
Attitudes and experiences in pain and opioids prescription
The attitudes and experiences of doctors in pain and opioid prescription are demonstrated in Table 3. The majority of the practitioners (93.8%) agreed that they always take a comprehensive pain history. More than half of them (62.5%) reported finding good pain control complex. It is also shown that participants who did not undergo any postings tended to delay the prescription of opioids as long as possible and felt that nursing staff were reluctant to administer even after they prescribed the opioids.
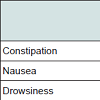
The side effects reported by participants are listed in Table 4. Side effects that are most commonly picked up are constipation (96.9%), nausea (90.6%), drowsiness (71.9%) and delirium (56.3%). It is also observed that doctors who have undergone haematology and oncology or palliative care postings are more likely to report pruritus and life threatening respiratory depression as side effects.
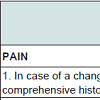
Attitudes and experiences in opioid rotation and tolerance
There is no significant difference (p>0.05) in opioid rotations attitudes between the two groups of doctors as demonstrated in Table 5. The majority of them rotate opioids in various circumstances. However, it is observed that those who have not gone through postings found calculating opioid dosages more difficult than those who have gone through the postings. All of the doctors who went through the postings reported noticing that tolerance can develop in the usage of opioids as compared to 86.4% of the participants from the group without postings. It is also noticed that 56.3% of doctors find patients’ fear of addiction is a barrier to usage of opioids in practice.
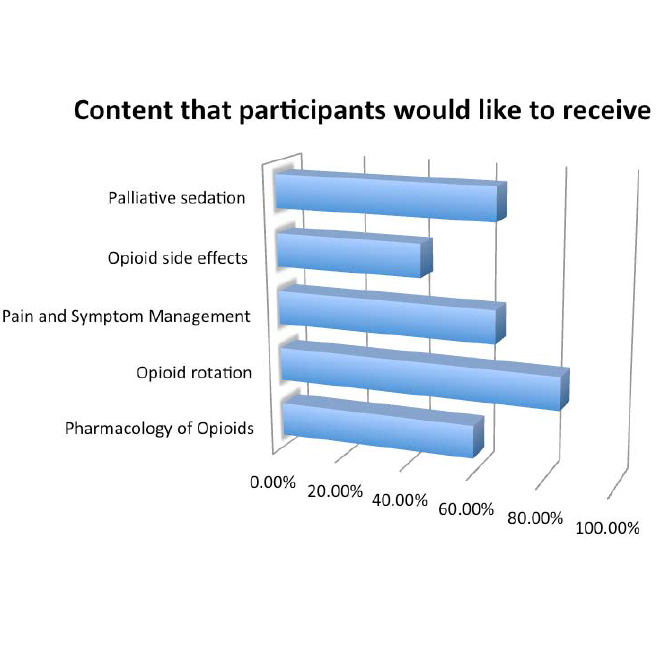
The majority of the participants (56.2%) felt that there was inadequate education on opioids and pain management as shown in Table 6. Among these people, more doctors from the group who have undergone postings (70%) felt that there was not enough education as compared to those who have not (47.6%). The preferred modes of education are lecture style sessions (68.8%) followed by other written sources (e.g. handbooks) and peer group teaching (37.5%). Participants also indicated the subjects in which they are interested to receive addition education as demonstrated in Figure 1. More than 50% of them showed interest in opioid rotation, palliative sedation, pain and symptom management, and pharmacology of opioids.
Discussion
It is challenging to study the level of knowledge among doctors with regards to pain management because there is no absolute right or wrong response to each question. Inconsistent training programs and learning experience have rendered doctors to have diverse pain management skills. Therefore, they may have good reasons to believe that their actions and management skills are suitable and correct based on their limited past clinical experiences. It is thus not appropriate to set a minimum number of questions to be answered correctly to determine the adequacy of a clinician. Results collected here can be postulated to reflect the general misconceptions held by junior doctors so that actions an be developed to rectify any knowledge gap.In our study, an average of 6 out of 11 statements (54%) concerning junior doctors’ knowledge was answered accurately. Other similar studies that investigated physicians’ knowledge based on questionnaires demonstrated a wide range of scores, ranging from 24% to 63% [17,29,30]. However, it is difficult to compare the overall scores of our study with these studies because the questionnaires are not standardized across all studies and the investigated participants have different qualifications and clinical experiences. Also, these studies are conducted across different countries where pain management guidelines and educational curriculum vary.
A few issues have been identified as lacking when the responses were analysed. Approximately two-thirds of the doctors were not aware that opioids might cause or worsen pain. Even though this is a rare effect, there is a growing body of evidence indicating that abnormal pain sensitivity does occur in patients who received opioid therapy. Instead of claiming that these patients have become pharmacologically tolerant to opioids and hence requiring more dosage to achieve the same analgesic effect, opioid-induced hyperalgesia could be the underlying reason for continuous pain complaints. Thus, clinicians should learn to distinguish opioid-induced pain sensitivity to tolerance, as different approaches are taken in managing these two side effects. In this case, increasing opioid dosage may even cause more pain to patients [31-33].
Also, less that one third (15.6%) of the doctors were aware that simultaneous prescription of a weak opioid and a strong opioid is contraindicated. However, there is a significant difference (p = 0.024) between the responses of the two groups of physicians with the group who has undergone postings performing better. This is not a true contra-indication per se in that no adverse reactions will occur; nevertheless, when adding tramadol, a weak opioid to morphine, a strong opioid, there is no reduction in pain whereas side effects increased [34,35].
As compared to Rurup’s study from which this questionnaire was modified from, the participants (three in four) were more aware that decreased renal function raises plasma concentration of morphine [14]. This result can be explained by the fact that Australia has constructed a statutory model that legislates continuing medical education in pain management as mandatory making pain relief an obligation for doctors [36]. The outcome of this legislation could have heightened the awareness of Australian doctors regarding complications of opioid therapy, resulting in a relatively competitive performance compared to their international counterparts.
Results showed that the majority of the junior doctors (96.9%) failed to realize that medicine treatment for nausea in opioid therapy is not completely evidence-based. Therapeutic recommendations are in fact established based on long years of anecdotal and clinical experience rather than a set of established guidelines [37].
Junior doctors who did not go through haematology and oncology or palliative care postings (p<0.05) were found to be less likely to report respiratory depression as a side effect. Such under-reporting among doctors can be attributed to the fact that opioid-induced respiratory depression is rare and doctors do not normally consider this as an impediment to necessary pain control. However, clinicians have to be aware that all opioids agonists will have some depressant effects on the brain-stem respiratory centre and most cases of death from opioid overdose are nearly always caused by respiratory arrest [38,39]. Literature suggests that there are mixed agonist-antagonist drugs, which have been developed so that they can act as an agonist for analgesic effects and antagonist for respiratory depression [40]. Also, if opioids are administered carefully with gradual dosage increments, respiratory depression could be avoided.
Constipation is the most common complication that has to be dealt with as revealed in this study whereby 96.9% of physicians reported it as a side effect. This is an outcome of improved education to raise doctors’ awareness in managing opioid side effects considering that constipation had been heavily underdiagnosed in the past [41]. Subsequently, a bowel regimen has been recommended with disimpaction deemed necessary should patients have no bowel movements for a few days.
Nausea and vomiting are not uncommon as demonstrated in this study with 90.6% physicians reporting it; nevertheless, tolerance to this side effect develops rapidly and therefore rendering specific therapy unnecessary [40]. However, doctors should be aware that should nausea persist even with antiemetic therapy, then a change in the route of opioid administration is warranted [42].
Opioid-induced delirium has been suggested to be a result of accumulation of morphine metabolites in advanced cancer patients [43]. Similar studies continue to demonstrate that delirium is frequently misdiagnosed and under-diagnosed [44]. This observation is, however, different from the results in our study with more than half of the junior doctors reporting it. However, there is still a significant difference between the two groups with fewer doctors from the group without postings recognising it up as a side effect (p =0.028). Possible reasons could be related to less clinical exposure and experience with patients on opioid therapy and thus highlighting the importance of a palliative care related posting.
A significant number of interns and residents have expressed interest in additional education in opioid rotation (84.1%), an echo of what the literature reveals [45,46]. Opioid rotation refers to a change from one opioid to another in order to enhance the response to analgesic therapy or reduce side effects despite sufficient dose was given [47]. Clinicians surveyed often find themselves not acquainted with opioid rotation. Even though there are equianalgesic dose tables that have been established, the ratios provided largely refers to the situation where a single dose is administrated and hence are not suitable in the context of long term opioid use [48]. Besides, relative potency of the drug varies across individuals depending on their condition and tolerance [47] and therefore, this requires experience and clinical judgement from the clinicians. This explains those physicians who have yet to undergone palliative care-related postings finding opioid calculation more difficult. Future studies also need to be conducted to refine the equianalgesic dose in addressing the potential of bidirectional change in relative potency when switching opioids so that clinical outcomes related to opioid rotation could be improved [47-50].
Almost all of the junior doctors (90.6%) noticed tolerance when prescribing opioids. Opioid tolerance refers to a state of reduced responsiveness to the pharmacologic effect of an opioid due to prior exposure or genetically determined insensitivity to the drug [51]. Acquired tolerance can be divided into three types: pharmacokinetic, pharmacodynamics and learned tolerance. Pharmacokinetic tolerance refers to alterations in the metabolism and distribution of a drug following repeated administrations of that drug causing a decreased concentration in the blood. Pharmacodynamic tolerance refers to adaptive changes adopted by the body’s systems after being exposed to the drug, such as a reduction in the numbers of receptors, so that a higher concentration of drug needs to be given to maintain similar response. Learned tolerance refers to a drug-induced effect reduction as an outcome of compensatory mechanisms that are developed [38]. Although tolerance has been recognised by the majority of the junior doctors, the study did not manage to identify their subsequent actions in addressing this side effect. Findings have demonstrated that tolerance can be overcome through opioid rotation. As such, doctors’ concerns about tolerance should neither justify delay in commencing opioid administration nor limit dose increase in a patient suffering from pain.
Addiction is defined as a “chronic disorder characterised by the excessive use of a substance causing psychological, physical and social harm to the user and continued use despite that harm” [38]. It is revealed in this study that more than half of those surveyed (56.3%) agreed that patients’ fear of addiction hampers them from prescribing opioids, resulting in underutilisation of opioid drugs and thus causing unnecessary pain. Such opiophobia can also be due to an overestimation of the adverse effects of opioid toxicity and a lack of systematic education among professionals [38]. Doctors have to be aware that addiction caused by opioid therapy is extremely rare in patients with no previous history of addictive disorders [52]. It is nevertheless naive to say that opioid therapy will not lead to addiction among other patients because such problems do arise often enough during chronic treatment to be of considerable concern [53]. However, clinicians should be reminded that they are already armed with much information that could help them with treating pain in a way that reduces the risk of addiction. By employing a structured treatment regime with subsequent follow up, clinicians will be able to identify problematic opioid use and treat any potential addiction once it is recognised. Doctors need to see that they are not abandoning their patients who are fearful and in need of pain relief but rather, they should assume the responsibility of explaining the benefits and minimal risks of opioid use with careful monitoring [52,53].
Also, with more than half of the participants (56.2%) indicating that education on pain management is inadequate further highlights the lack of formal pain management curricula in place in the Australian healthcare education system. However, some of the participants surveyed might have been trained overseas. Hence, they might not best represent the result of a revamped local undergraduate medical curriculum in which more emphasis on palliative care has been given [54].
This study also presents an observation whereby more junior doctors from the group who have undergone haematology and oncology or palliative care postings felt the need for additional education on pain as compared to those who have not undergone any postings. Reasons can be due to their prior clinical experiences in handling larger numbers patients suffering from both acute and chronic pain during these postings. Such first-hand accounts exposed their absolute lack of proficiency in managing pain therefore causing them to feel an urgency to expand their knowledge. This is as opposed to their counterparts who have yet to experience and acknowledge their inefficient expertise in pain management.
The preferred methods of teaching among participants are lecture style sessions, written sources peer group teaching, and development of clinical protocols. A few previous studies have also suggested that training programs can comprise more popular learning ways such as consultant and registrar teachings, clinical skills teaching and structural tutorials which is in line with the results of this study [55-58].
Strengths and limitations of the study
This study has managed to identify the gaps in knowledge among Australian junior doctors and the results can be useful in structuring an education curriculum on pain management targeting undergraduate and postgraduate students or practitioners.
The limitations of this study are its moderate response and the small study sample size from being conducted in a single hospital facility. As such, the study might not be representative of the general population of practitioners across Australia. It is no doubt that a larger scale of population study among doctors is thus warranted. Also, the participants volunteered would have been more interested in palliative medicine making them more agreeable to participate in the questionnaire which might give a slight biasness to the study.
Another limitation is that only a limited number of themes have been explored. Subsequent actions taken by doctors to address these problems such as opioid side effects were not adequately investigated. Furthermore, some knowledge statements are ambiguous and are subjected to individuals’ interpretation. The correct response to the question of whether concurrent management of nausea in opioid therapy is evidencebased can be debatable because there are indeed best practices for managing opioid-induced nausea even though there are insufficient clinical trials to test their true efficacy [34].
Conclusion
Junior doctors who have gone through haematology and oncology or palliative care postings seem to be performed more effectively in pain management than those who have not. Nevertheless, there are still gaps in medical knowledge on pain management. A few areas that were identified are: combination of opioid drugs in pain management, opioid rotation, dosage calculation and fear to start opioid administration. One possible reason to explain such a phenomenon is time constraint among teachers including senior consultants or specialists and students in hospital, thus resulting in an ineffective transfer of knowledge among junior doctors. It is therefore necessary to establish a systematic education system focusing on pain management that can resolve the many issues and doubts faced by healthcare practitioners when it comes to managing pain. Also, further efforts in educating the general public about the effectiveness and applicability of opioid therapy should be placed in order to correct their unwarranted fear of opioids.References
- Manias E, Bucknall T, Botti M (2004) Assessment of patient pain in the postoperative context. West J Nurs Res 26: 751-769.
- Blyth FM, March LM, Brnabic AJM, Jorm LR, Williamson M, et al. (2001) Chronic pain in australia: A prevalence study. Pain 89: 127-134.
- Yates PM, Edwards HE, Nash RE, Walsh AM, Fentiman BJ, et al. (2002) Barriers to effective cancer pain management: A survey of hospitalized cancer patients in australia. J Pain Symptom Manage 23: 393-405.
- Pain Australia. Australia's national pain strategy (Updated 2012)
- National Health and Medical Research Council. Acute pain management: Scientific evidence (Updated 2010)
- Oldenmenger WH, Sillevis Smitt PAE, van Dooren S, Stoter G, van der Rijt CCD (2009) A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: A critical appraisal. Eur J Cancer 45: 1370-1380.
- Ury WA, Rahn M, Tolentino V, Pignotti MG, Yoon J, et al. (2002) Can a pain management and palliative care curriculum improve the opioid prescribing practices of medical residents? Journal of General Internal Medicine. J Gen Intern Med 17: 625-631.
- Apfelbaum JL, Chen C, Mehta SS, Gan TJ (2003) Postoperative pain experience: Results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg 97: 534-540.
- Boström B, Sandh M, Lundberg D, Fridlund B (2004) Cancer-related pain in palliative care: Patients' perceptions of pain management. J Adv Nurs 45: 410-419.
- Portenoy RK, Lesage (1999) Management of cancer pain. Lancet 353: 1695-1700.
- Cleeland CS1, Gonin R, Hatfield AK, Edmonson JH, Blum RH, et al. (1994) Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 330: 592-596.
- Gallagher R, Hawley P, Yeomans W (2004) A survey of cancer pain management knowledge and attitudes of british columbian physicians. Pain Res Manag 9: 188-194.
- Hanks GW, Conno F, Cherny N, Hanna M, Kalso E, et al. (2001) Morphine and alternative opioids in cancer pain: The EAPC recommendations. Br J Cancer 84: 587-593.
- Mette L Rurup, Christiaan A Rhodius, Sander D Borgsteede, Manon SA Boddaert, Astrid GM Keijser, et al. (2010) The use of opioids at the end of life: The knowledge level of dutch physicians as a potential barrier to effective pain management. BMC Palliative Care 9:23.
- Ponte CD, Johnson-Tribino J (2005) Attitudes and knowledge about pain: An assessment of west virginia family physicians. Fam Med 37: 477-480.
- Rhee JJ-, Zwar N, Vagholkar S, Dennis S, Broadbent AM, et al. (2008) Attitudes and barriers to involvement in palliative care by australian urban general practitioners. J Palliat Med 11: 980-985.
- Elliott TE, Murray DM, Elliott BA, Braun B, Oken MM, et al. (1995) Physician knowledge and attitudes about cancer pain management: A survey from the minnesota cancer pain project. J Pain Symptom Manage 10: 494-504.
- Clark JM, Lurie JD, Claessens MT, Reed VA, Jernstedt GC, Goodlin SG, et al. (2003) Factors associated with palliative care knowledge among internal medicine house staff. J Palliat Care 19: 253-257.
- Sloan PA, Donnelly MB, Schwartz RW, Sloan DA (1996) Cancer pain assessment and management by housestaff. Pain 67: 475-481.
- Von Gunten CF, Twaddle M, Preodor M, Neely KJ, Martinez J, et al. (2005) Evidence of improved knowledge and skills after an elective rotation in a hospice and palliative care program for internal medicine residents. Am J Hosp Palliat Care 22: 195-203.
- Vainio A (1995) Treatment of terminal cancer pain in france: A questionnaire study. Pain 62: 155-162.
- Zanolin ME, Visentin M, Trentin L, Saiani L, Brugnolli A, et al. (2007) A questionnaire to evaluate the knowledge and attitudes of health care providers on pain. J Pain Symptom Manage 33: 727-736.
- Boakes J, Gardner D, Yuen K, Doyle S (2000) General practitioner training in palliative care: An experiential approach. J Palliat Care 16: 11-19.
- Kim M, Park H, Park EC, Park K (2011) Attitude and knowledge of physicians about cancer pain management: Young doctors of south korea in their early career. Jpn J Clin Oncol 41: 783-791.
- Von Gunten CF, Mullan PB, Harrity S, Diamant J, Heffernan E, et al. (2003) Residents from five training programs report improvements in knowledge, attitudes and skills after a rotation with a hospice program. J Cancer Educ 18: 68-72.
- Mitchell GK, Reymond EJ, McGrath BP (2004) Palliative care: Promoting general practice participation. Med J Aust 180: 207-208.
- Aabom B, Kragstrup J, Vondeling H, Bakketeig LS, Stovring H (2006) Does persistent involvement by the GP improve palliative care at home for end-stage cancer patients? Palliat Med 20: 507-512.
- Yuen KJ, Behrndt MM, Jacklyn C, Mitchell GK (2003) Palliative care at home: General practitioners working with palliative care teams. Med J Aust 179: S38-S40.
- Sapir R, Catane R, Strauss-Liviatan N, Cherny NI (1999) Cancer pain: Knowledge and attitudes of physicians in israel. J Pain Symptom Manage 17: 266-276.
- Mortimer JE, Bartlett NL (1997) Assessment of knowledge about cancer pain management by physicians in training. J Pain Symptom Manage 14: 21-28.
- Mao J (2006) Opioid-induced abnormal pain sensitivity. Curr Pain Headache Rep 10: 67-70.
- Mao J (2002) Opioid-induced abnormal pain sensitivity: Implications in clinical opioid therapy. Pain 100: 213-217.
- Ballantyne JC (2006) Opioids for chronic nonterminal pain. South Med J 99: 1245-1255.
- Borgsteede SD, Rhodius CA, De Smet PAGM, Pasman HRW, Onwuteaka-Philipsen BD, et al. (2011) The use of opioids at the end of life: Knowledge level of pharmacists and cooperation with physicians. Eur J Clin Pharmacol 67: 79-89.
- Marcou TA, Marque S, Mazoit J, Benhamou D (2005) The median effective dose of tramadol and morphine for postoperative patients: A study of interactions. Anesth Analg 100: 469-474.
- Brennan F, Carr DB, Cousins M (2007) Pain management: A fundamental human right. Anesth Analg 105: 205-221.
- Laugsand EA, Kaasa S, Klepstad P (2011) Management of opioid-induced nausea and vomiting in cancer patients: Systematic review and evidence-based recommendations. Palliat Med 25: 442-453.
- Collett B (1998) Opioid tolerance: The clinical perspective. Br J Anaesth 81: 58-68.
- Cepeda MS, Farrar JT, Baumgarten M, Boston R, Carr DB, et al. (2003) Side effects of opioids during short-term administration: Effect of age, gender, and race. Clin Pharmacol Ther 74: 102-112.
- Kanner R (2009) Chapter 34-opioid analgesics. In: Pain management secrets (third edition).
- Mancini IL, Hanson J, Neumann CM, Bruera ED (2000) Opioid type and other clinical predictors of laxative dose in advanced cancer patients: A retrospective study. J Palliat Med 3: 49-56.
- Lawlor PG, Bruera E (1998) Side-effects of opioids in chronic pain treatment. Curr Opin Anaesthesiol 11: 539-545.
- Ashby M, Fleming B, Wood M, Somogyi A (1997) Plasma morphine and glucuronide (M3G and M6G) concentrations in hospice inpatients. J Pain Symptom Manage 14: 157-167.
- Breitbart W, Bruera E, Chochinov H, Lynch M (1995) Neuropsychiatric syndromes and psychological symptoms in patients with advanced cancer. J Pain Symptom Manage 10: 131-141.
- Cleeland CS, Janjan NA, Scott CB, Seiferheld WF, Curran WJ (2000) Cancer pain management by radiotherapists: A survey of radiation therapy oncology group physicians. Int J Radiat Oncol Biol Phys 47: 203-208.
- Turk DC, Brody MC, Okifuji EA (1994) Physicians' attitudes and practices regarding the long-term prescribing of opioids for non-cancer pain. Pain 59: 201-208.
- Knotkova H, Fine PG, Portenoy RK (2009) Opioid rotation: The science and the limitations of the equianalgesic dose table. J Pain Symptom Manage 38: 426-439.
- Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E (2001) Equianalgesic dose ratios for opioids: A critical review and proposals for long-term dosing. J Pain Symptom Manage 22: 672-687.
- Fine PG, Portenoy RK (2009) Establishing "best practices" for opioid rotation: Conclusions of an expert panel. J Pain Symptom Manage 38: 418-425.
- Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL (2009) Opioid equianalgesic tables: Are they all equally dangerous? J Pain Symptom Manage 38: 409-417.
- Cox BM (1994) Opiate drug tolerance: An introduction. Regul Pept 54: 71-72.
- Portenoy RK, Savage SR (1997) Clinical realities and economic considerations: Special therapeutic issues in intrathecal therapy - tolerance and addiction. J Pain Symptom Manage 14: S27-S35.
- Ballantyne JC, LaForge KS (2007) Opioid dependence and addiction during opioid treatment of chronic pain. Pain 129: 235-255.
- Cairns W, Yates PM (2003) Education and training in palliative care. Med J Aust 179: S26-S28.
- Dent AW, Crotty B, Cuddihy HL, Duns GC, Benjamin J, et al. (2006) Learning opportunities for australian prevocational hospital doctors: Exposure, perceived quality and desired methods of learning. Med J Aust 184: 436-440.
- Gleason AJ, Daly JO, Blackham RE (2007) Prevocational medical training and the australian curriculum framework for junior doctors: A junior doctor perspective. Med J Aust 186: 114-116.
- Neate SL, Dent AW, Weiland TJ, Farish S, Jolly BC, et al. (2008) Barriers to continuing medical education in australian prevocational doctors. Australian Health Review 32: 292-300.
- Roberts CM, Caan W, Young J, Weatherstone R (2007) How hospital trainees prefer to learn. Br J Hosp Med 68: 267-269.