Journal of Clinical & Medical Case Reports
Download PDF
Case Report
*Address for Correspondence: Tristan Charles John Pettit, MB ChB, FRACP, Paediatric Oncologist, Christchurch Hospital, Christchurch, New Zealand; E-mail: tristan.pettit@cdhb.health.nz
Citation: Andre M, Walls T, Haider N, Pettit TCJ. Asymptomatic Presentation of Mediastinal Actinomycosis in a Pediatric Patient with Acute Lymphoblastic Leukemia. J Clin Med Case Reports. 2015;2(1): 3.
Copyright 2015 © Pettit et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Medical Case Reports | ISSN: 2332-4120 | Volume: 2, Issue: 1
Submission: 14 December 2014 | Accepted: 29 January 2015 | Published: 03 February 2015
Asymptomatic Presentation of Mediastinal Actinomycosis in a Pediatric Patient with AcuteLymphoblastic Leukemia: Case Report and Discussion
Margaret Andre1, Tony Walls2, Nadeem Haider1 and Tristan Charles John Pettit1*
- 1Christchurch Hospital, Christchurch, New Zealand
- 2University of Otago, Christchurch, New Zealand
*Address for Correspondence: Tristan Charles John Pettit, MB ChB, FRACP, Paediatric Oncologist, Christchurch Hospital, Christchurch, New Zealand; E-mail: tristan.pettit@cdhb.health.nz
Citation: Andre M, Walls T, Haider N, Pettit TCJ. Asymptomatic Presentation of Mediastinal Actinomycosis in a Pediatric Patient with Acute Lymphoblastic Leukemia. J Clin Med Case Reports. 2015;2(1): 3.
Copyright 2015 © Pettit et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use,distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Medical Case Reports | ISSN: 2332-4120 | Volume: 2, Issue: 1
Submission: 14 December 2014 | Accepted: 29 January 2015 | Published: 03 February 2015
Abstract
We report a nine year old male with Philadelphia positive Precursor B Acute Lymphoblastic Leukemia who was diagnosed with mediastinal actinomycosis following failed central line placement. The patient had a normal chest X-Ray at diagnosis, had a good response to initial chemotherapy, but subsequently developed a widened mediastinum with vascular compression. The differential diagnosis for this included infection, leukemia relapse, a second malignancy and vascular and congenital abnormalities. Actinomycosis is associated with hematogenous spread and invasion of neighbouring structures, and should be considered in the differential diagnosis of any child with a mediastinal mass.Keywords
Asymptomatic mediastinal actinomycosis; Thoracic mass; Acute lymphoblastic leukemiaIntroduction
This is the first reported case of mediastinal actinomycosis developing during induction chemotherapy for Philadelphia Positive Precursor B Acute Lymphoblastic Leukemia (Ph+ ALL) in a pediatric patient. This was an unusual presentation in that he was asymptomatic at the time and was incidentally found to have a widened mediastinum following failed central venous access device insertion. Acute lymphoblastic leukaemia is known to be the most common type of cancer in childhood constituting approximately 25% of cases in patients below 15 years of age [1]. The Philadelphia chromosome, a translocation on long arms of chromosomes 9 and 22, t(9;22) (q34;q11), is present in 3-4% of pediatric acute lymphoblastic leukaemia cases [2]. This translocation forms a fusion gene, BCRABL1 which is a target for tyrosine kinase inhibitors (TKIs) such as dasatanib. The addition of TKIs to the treatment of Ph+ALL has been associated with significantly improved outcomes.Case Description
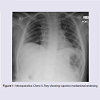
A nine year old Caucasian male was referred to our pediatric oncology service with a provisional diagnosis of acute leukemia following a three week history of lethargy, intermittent fevers and night sweats. Physical examination at presentation revealed pyrexia, pallor and mild hepatomegaly but no findings indicative of an infective focus of fever. C-Reactive Protein (CRP) level was within normal limits. A full blood count showed an elevated white cell count of 161 x 109/L with numerous blast cells seen on the blood film. A bone marrow aspirate showed marked hypercellularity with the white blood cell differential showing 91% blast cells. Morphologically, the blast cells had scant basophilic cytoplasm, no granules and oval nucleiwith prominent nucleoli. immunophenotyping showed a clonal population of immature B cells with positivity for CD 9, CD10, CD19, CD34 and D45. Cerebrospinal fluid obtained during diagnostic lumbar puncture was negative for blasts. The patient was diagnosed with Precursor B Acute Lymphoblastic Leukemia (Pre B ALL). Routine Chest X-Ray (CXR) performed during initial diagnostic work-up, did notreveal any mediastinal abnormality. Initial oral health assessment revealed mild dental caries. A peripherally inserted central catheter (PICC) was placed during the initial diagnostic procedure. The patient was classified as “high risk” due to high white cell count at diagnosis. Induction phase chemotherapy was commenced following the high risk Children’s Oncology Group (COG) protocol AALL1131. Initial fevers settled quickly, and with negative blood cultures the antibiotics (piperacillin/tazobactam) were ceased after five days. Cytogenetic analysis of the bone marrow sample revealed an abnormal clone with t(9;22) (q34;q11.2). Fluorescent in situ Hybridisation (FISH) analysis confirmed the presence of the standard BCR/ABL1 fusion gene in 90% of the interphase nuclei analysed. Thus, the patient’s diagnosis was modified to Ph+ ALL and the treatment was realigned to the dasatinib based COG AALL1122 protocol for Ph+ ALL from day 8. The bone marrow suppression resulted in a prolonged severe neutropaenia (neutrophil count < 0.5 x10 9 /L) from day 15 of induction, lasting 22 days. The patient was found to have mild oral mucosal breakdown during this phase of reatment. He had a single episode of asymptomatic pyrexia associated with severe neutropaenia for which he was treated with a 48 hr course of wide spectrum antibiotics as per local guidelines (Tazocin). Blood cultures and inflammatory markers were negative. An ultrasound (USS) guided Dual Lumen Hickman central line insertion via the right internal jugular vein was attempted on day 42 of treatment. Timing for this procedure was based on blood count recovery and pairing it with repeat bone marrow assessment following completion of induction therapy. Obstruction at the level of the superior vena cava was encountered and the central line was unable to be passed beyond this location. An intraoperative CXR (Figure 1) showed superior mediastinal widening and a subsequent CT chest (Figure 2) confirmed the presence of right paratracheal and subcarinal soft tissue enlargementsuggestive of lymphadenopathy. Epstein Barr virus, cytomegalovirus, and toxoplasmosis serology was negative and there was no history of exposure to tuberculosis. An USS guided transbronchial needle aspiration of the mass was performed. Microscopy showed polymorphic neutrophils and no malignant cells. Gram stain and direct aerobic and anaerobic cultures were negative, but the enrichment (broth) culture of the aspirate grew Actinomyces species which was further identified as A. odontolyticus by DNA sequencing of the 16S rRNA gene. An antibiotic sensitivities panel was unable to be produced in view of the molecular technique used. The diagnosis of mediastinal actinomycosis was established. The patient was commenced on daily ceftriaxone in view of universal sensitivity of the species to beta-lactam antibiotics and the convenience of a once daily delivery pattern. A follow up CXR showed significant reduction in size of the mediastinal widening four weeks later. The patient completed a six month course of treatment at which point a CT chest showed complete resolution of the mediastinal mass.Discussion
Actinomyces is known to be a commensal organism in the oralcavity, gastrointestinal tract and female genitourinary tract [3].They are gram-positive, microaerophilic, filamentous, anaerobic.bacteria [3,4,6]. The most common sites of actinomycosis includecervicofacial (55%), abdominopelvic (20%), thoracic (15%), and rarerforms are noted in skin, brain, pericardium and limbs (10%) [3,5]. Actinomycosis is known to present in a slow and progressive fashion,often crossing tissue planes and presenting with a mass lesion [3,7]. Actinomyces odontolyticus frequently colonizes the oral cavity [8] and is important in the pathogenesis of dental caries. It is commonly associated with hematogenous spread [4]. Poor oral hygiene is an established risk factor for actinomycosis [4,5,9]. Dental caries and inflamed gingivae act as a site of residence for commensal organisms such as A. odontolyticus, and following oral mucosal breakdown, local or haematogenous spread can occur. Dental caries or chemotherapy related oral mucosal breakdown could explain the mechanism of entry for our patient, with subsequent hematogenous spread to the mediastinal lymph nodes. The differential diagnosis of a mediastinal mass in children includes benign and malignant neoplasms, vascular abnormalities, congenital anomalies and infection [10]. Our patient’s mediastinal widening had evolved during the six week interval between diagnosis and time of central line placement. In this context, the presence of a congenital or vascular abnormality seemed unlikely. We considered a relapse of the patient’s leukemia but felt this was also highly unlikely given he had quickly cleared blast cells from his peripheral blood and his day 28 bone marrow aspirate showed morphological remission. This scenario would be more likely with T cell lymphoblastic leukemia, which is associated with a mediastinal mass in up to 70% at diagnosis [11]. Infectious lymphadenopathy was also considered. The most common infectious causes of mediastinal lymphadenopathy in children are tuberculosis, histoplasmosis and nfectious mononucleosis [10]. The risk of tuberculosis was assessed as low due to patient’s ethnic background, no significant past medicalhistory and absence of exposure to high risk contacts. The patient’s cytomegalovirus and Epstein-Barr virus status was investigated and was negative. A second malignant diagnosis was also considered. Concurrent mediastinal neuroblastoma has been described in pediatric patients with ALL [12] and acute myeloid leukemia (AML) [13]. A five year old child with Ewing Sarcoma of the radius had ALL diagnosed following the initial staging bone marrow aspirate [14], and retroperitoneal teratoma has also been noted as a concurrent diagnosis in an infant with AML [15]. Immunosuppression is a known risk factor for the development of actinomycosis [3,4,7]. Our patient had received six weeks of induction chemotherapy including high dose steroids and had experienced a prolonged period of neutropaenia. Although it had resolved six days prior to the attempted Hickman line insertion procedure, duration of neutropenia has previously been described as the most important risk factor for infectious complications in the treatment of acute leukemia [16]. Actinomycosis during treatment for ALL has been described previously [6,9]. There have been no previous reports of actinomycosis presenting as a mediastinal mass in this group. One case report described a 17 year old female with T cell ALL who had left sided consolidation and a pleural effusion 8 days following commencement of induction chemotherapy [6]. She had a left sided pneumonia with pleural effusion. The pleural aspirate yielded Actinomyces viscosus, a rare member of the Actinomyces genus. Delayed identification of actinomycosis can lead to serious consequences. Complications of thoracic actinomycosis can include empyema, hemoptysis, rib destruction and chronic sinus discharge [3,7]. Specifically, mediastinal disease can progress locally into the heart, with pericarditis, myocarditis and endocarditis being possible consequences [4]. A further unique aspect of this case is that the finding of mediastinal widening was identified only following failed central venous access device (CVAD) placement due to vascular obstruction. This mode of CVAD insertion failure is rare, in two pediatric reviews of CVAD placement at time of ALL diagnosis (n=287 patients), there was no cases of unsuccessful placement secondary to vascular compression [18,19]. Radiographic exclusion of mediastinal widening is routinely undertaken as part of the diagnostic process for acute leukaemia. Our patient had no mediastinal widening on the CXR taken at diagnosis. Six weeks later, at the time of CVAD insertion, there was no clinical indication to repeat the CXR preoperatively. The incidental nature of the identification of the mediastinal actinomycosis allowed appropriate treatment to occur before the infection had a chance to spread beyond the mediastinal lymph nodes. Mediastinal widening is a key clinical sign in paediatric oncology. In children who are immunosuppressed but remain in remission a widened mediastinum is most likely to be due to an infectious agent. Actinomycosis can present with mediastinal disease and needs to be considered in the differential diagnosis of any child with a thoracic mass.References
- (2014) Childhood acute lymphoblastic leukemia treatment (PDQ®): General information about childhood Acute Lymphoblastic Leukemia (ALL). National Cancer Institute.
- Bernt KM, Hunger SP (2014) Current concepts in pediatric Philadelphia chromosome-positive acute lymphoblastic leukemia. Front Oncol 4: 54.
- Petroianni A, Conti V, Terzano C (2011) A thoracic mass infiltrating chest wall. Eur Rev Med Pharmacol Sci 15: 345-348.
- Wong VK, Turmezei TD, Weston VC (2011) Actinomycosis. BMJ 343: d6099.
- de la Espina MA, Lopez-Menendez C, Ruiz-Martinez R, Molino-Trinidad C (2001) Pulmonary actinomycosis with thoracic soft tissue mass: a rare onset form. Eur J Radiol 37: 195-199.
- Dolai TK, Kumar R, Chakrabarti P, Das A, Mahapatra M, et al. (2008) Actinomycetes species infection in a patient of T-cell acute lymphoblastic leukemia (ALL) presenting with loculated pleural effusion. Pediatr Hematol Oncol 25: 477-480.
- Yeung VH, Wong QH, Chao NS, Leung MW, Kwok WK (2008) Thoracic actinomycosis in an adolescent mimicking chest wall tumor or pulmonary tuberculosis. Pediatr Surg Int 24: 751-754.
- Chao CT, Liao CH, Lai CC, Hsueh PR (2011) Liver abscess due to Actinomyces odontolyticus in an immunocompetent patient. Infection 39: 77-79.
- Hovi L, Saarinen UM, Donner U, Lindqvist C (1996) Opportunistic osteomyelitis in the jaws of children on immunosuppresive chemotehrapy. J Pediatr Hematol Oncol 18: 90-94.
- Ranganath SH, Lee EY, Restrepo R, Eisenberg RL (2012) Mediastinal masses in children. AJR Am J Roentgenol 198: W197-216.
- Saraswatula A, McShane D, Tideswell D, Burke GA, Williams DM, et al. (2009) Mediastinal masses masquerading as common respiratory conditions of childhood: a case series. Eur J Pediatr 168: 1395-1399.
- ZhuD’Angelo P, Grigoli A, Sementa AR, Tropia S, Alaggio R, et al. (2012) Simultaneous diagnosis of acute lymphoblastic leukemia and peripheral neuroblastic tumor in a child. J Pediatr Hematol 34: 72-75
- Di Cataldo A, Mazzocco K, Magro G, Mirabile E, Lo Nigro L, et al. (2011) Simultaneous tumors: acute myeloid leukemia infiltrating mediastinal ganglioneuroblastoma. Pediatr Blood Cancer 56: 298-300.
- 13. Masjosthusmann K, Bielack SS, Köhler G, Florax A, Schiborr M, et al. (2005) Concomitant Ewing sarcoma and acute lymphoblastic leukemia in a 5-year-old girl. Pediatr Blood Cancer 45: 846-849.
- Park SS, Park HS, Lee CH, Lee EY, Lim YT (2006) A case of concurrent acute myelogenous leukaemia and retroperitoneal teratoma in an infant. Clin Pediatr Hematol Oncol 13: 55-59.
- Chanock SJ, Pizzo PA (1997) Infectious complications of patients undergoing therapy for acute leukemia: current status and future prospects. Semin Oncol 24: 132-140.
- Barikbin P, Grosser K, Hahn G, Fischer R, Suttorp M (2007) Thoracic actinomycosis imitating a malignant chest wall tumor. Diagnosis: pulmonary actinomycosis. J Pediatr Hematol Oncol 29: 345-346.
- Gonzalez G, Davidoff AM, Howard SC, Pui CH, Rao BN, et al. (2012) Safety of central venous catheter placement at diagnosis of acute lymphoblastic leukemia in children. Pediatr Blood Cancer 58: 498-502.
- Carr E, Jayabose S, Stringel G, Slim M, Ozkaynak MF, et al. (2006) The safety of central line placement prior to treatment of pediatric acute lymphoblastic leukemia. Pediatr Blood Cancer 47: 886-888.