Journal of Addiction & Prevention
Download PDF
Research Article
*Address for Correspondence Jan Copeland, Director, Cannabis Information and Support, PO Box 257, St Ives, New South Wales 2052, Australia, Tel: +61 414 385 153; E-mail: ProfJ@CiSCopeland.com
Citation: Gates P, Todd S, Copeland J. Survey of Australian’s knowledge, Perception and Use of Cannabis for Medicinal Purposes. J Addiction Prevention. 2017;5(1): 10.
Copyright © 2017 Gates P, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 5, Issue: 1
Submission: 14 March, 2017 | Accepted: 13 April, 2017 | Published: 20 April, 2017
Survey of Australian’s knowledge, Perception and Use of Cannabis for Medicinal Purposes
Peter Gates1, Stephanie Todd1 and Jan Copeland1,2*
- 1National Cannabis Prevention and Information Centre, University of New South Wales, Sydney, New South Wales, Australia
- 2Cannabis Information and Support, Sydney, New South Wales, Australia
*Address for Correspondence Jan Copeland, Director, Cannabis Information and Support, PO Box 257, St Ives, New South Wales 2052, Australia, Tel: +61 414 385 153; E-mail: ProfJ@CiSCopeland.com
Citation: Gates P, Todd S, Copeland J. Survey of Australian’s knowledge, Perception and Use of Cannabis for Medicinal Purposes. J Addiction Prevention. 2017;5(1): 10.
Copyright © 2017 Gates P, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Addiction & Prevention | ISSN: 2330-2178 | Volume: 5, Issue: 1
Submission: 14 March, 2017 | Accepted: 13 April, 2017 | Published: 20 April, 2017
Keywords
Marijuana; Cannabis; Medicinal use; Recreational useAbstract
Objective: Changes to national and some state’s policy on the cultivation and prescription of cannabis for medicinal purposes will soon directly impact Australian medical practitioners. We investigate differences in demographics, use patterns and the perceptions held by individuals who use cannabis for medicinal or recreational purposes and non-users.Method: Online survey advertised on the newsfeed of Australian Facebook users aged 18 years or over between March and May of 2016. A total sample of 1578 completed the survey, 199 (12.61%) were non-cannabis users, 489 (31.99%) were recreational-only users, 82 (5.20%) were medicinal-only users, and 808 (51.20%) used both recreationally and medicinally. Detailed questions regarded demographics, health, substance use, and knowledge and perceptions of medicinal cannabis use and policy in Australia.
Results: The sample most commonly perceived cannabis to effectively treat pain and mental health conditions. Most medicinal users also reported frequently smoking cannabis for non-medicinal purposes. Overall, participant knowledge did not accurately reflect the current evidence base for medicinal cannabis. Differences by cannabis use motivation are discussed.
Conclusions: This survey highlights important differences between non-users and current medicinal and non-medicinal cannabis users in demographics, patterns of cannabis use and regarding knowledge and perceptions of medicinal cannabis. The mismatch between the state of evidence to inform safe and effective clinical practice and beliefs of medicinal cannabis users must be addressed and may negatively impact clinical rapport and patient outcomes.
Introduction
The majority of the public support the legalisation of cannabis use for medicinal purposes in Australia, although often in the absence of a strong evidence base for its efficacy [1-5]. According to the representative 2013 National Drug Strategy Household Survey, just over two thirds of the Australian population supported a “change in legislation permitting the use of marijuana for medical purposes” and 75.3% supported “a clinical trial for people to use marijuana to treat medical conditions” [6]. Such weight of opinion can be a powerful motivation for political change as has been reflected in the recent legalisation of medicinal cannabis use in approximately half of the US [7]. Similarly, public sentiment in Australia has prompted recent changes in regional policies. For example, in 2014, the New South Wales Government Terminal Illness Cannabis Scheme (TICS) was established to prevent the prosecution of certain terminally ill individuals using cannabis under a registered doctor’s advice [8]. Since this time the Australian Federal Parliament has also passed amendments to the Narcotic Drugs Act 1967 to allow for the cultivation of cannabis for medicinal or scientific purposes with prescription access via registered General Practitioners as early as 2017. Despite this, some believe that movements toward the legalisation of cannabis use for medical purposes are premature as there is not yet a solid evidence base to guide safe and effective clinical practice where prescription without TGA regulation is required in recent policy changes [9-13].There are two primary motivations held by those who support the medicinal use of cannabis [14]. Firstly, there is the belief that cannabis is proven to be an effective and safe medicine, and as such, should be available for use. Secondly, there is the belief that, regardless of unproven effectiveness, it is a human right of a suffering person to have access to all possible treatment options and that regulation will reduce harms associated with the black market. The legitimacy of these beliefs has been the subject of some intensive study. To address the existing evidence relating to the drug’s efficacy and safety, comprehensive reviews of controlled clinical trials began in the late 90s and there has been a resurgence of interest in the last few years [9-13,15-17]. Such reviews have consistently cited a lack of supportive evidence - in particular for the smoked Cannabis plant and for the use of cannabis preparations to treat health conditions other than pain and spasticity or for paediatric seizure management where current therapies fail [10,12,18]. The strong literature on the risks of physical, mental and psycho-social harms associated with regular cannabis use is also well known [19].
In this climate of debate it becomes paramount to identify a regulatory model which would best appease all parties with the least potential for a negative impact on public health. Such a model would have the primary goal of giving medicinal users access to a safe and evidence based product; however this system is in competition with already accessible unregulated cannabis use. The current changes in the US and other places offer the opportunity to observe several different models of regulation that are being implemented [20-22]. The current regulatory models can be defined by how easily an individual can become a medicinal user (whether by registration or by mandatory physician statement and what health conditions are approved), the quantity of cannabis that can be legally accessed (quantity of plant as well as number of patients per caregiver) and the capacity of the state to monitor and regulate any diversion into illegal markets (whether growing is allowed and number of permitted dispensaries). As Australia has begun to make regulatory options, it is necessary to determine both the beliefs and opinions the public shares in relation to medicinal cannabis use as well as how it should be regulated [23,24]. Surprisingly, only a single initial survey of Australian medicinal cannabis users has been published and is now over a decade old [25]. That survey found that the participants had used cannabis for many years to treat a number of different conditions - most commonly chronic pain (57%) and depression (56%).
Only five general population surveys have been conducted outside of Australia on this question [26-31]. In contrast, a plethora of research has focussed on those registered to medicinal cannabis dispensaries (for example [32,33]), or with particular health conditions (for example [34-36], and have lacked comparisons between non-users or recreational users. Each of the available population surveys were conducted across North America, although two were specific to particular regions (Ontario [29] and California [30]). Across surveys, approximately 10% or less of the participants reported medicinal cannabis use although medicinal use was more prevalent among males, whites and Hispanics, and over the age of 35 years. Medicinal cannabis use was typically reported to be daily and administered by smoking joints, bowls or pipes. Unfortunately, none of these representative studies focussed on opinions relating to regulatory models or separates those who use cannabis solely for medical purposes and not also recreational purposes.
Given the limitations in knowledge and perceptions of medicinal cannabis use among the Australian population, the aim of this study was to provide the most detailed investigation of medicinal and non-medicinal cannabis use in Australia. Using this information will help increase understanding of the differences between non-users and current medicinal and non-medicinal cannabis users regarding perceptions of risk and views on policy changes and highlight issues likely to impact on medical practice in the new regulatory environment.
Methods
Participants and procedureEthics approval for this study was obtained from the University of New South Wales Human Research Ethics Committee. Between March and May of 2016 a paid advertisement for the survey was placed on the Facebook advertisement platform and appeared on the newsfeed of Facebook users aged 18 years or over who had a listed location within Australia and invited them to complete a survey on ‘drug use’. The advertisement had a click through rate of 1.4% (indicating effectiveness by industry standards of a score above 1% [37]) and reached 416,319 individuals. Clicking on this advertisement took the respondent to a provided link for the online survey where they received information on the survey and then provided consent to continue. The legitimacy of this recruitment technique in the addictions field has been described previously [38].
A total of 3388 adults responded positively to the advertisement and began the survey. A total of five obvious hoax responses and an additional 72 individuals were removed during data cleaning as they contained conflicting information indicating careless or artificial responding. Of the remaining 3311, 47.7% (n = 1578) provided complete data and were thus included into this study.
Survey
The survey was published online using the free ‘Survey Monkey’ service (https://www.surveymonkey.com/). The content was largely adapted from Swift and colleagues to cover the Australian publics’ knowledge, perception and patterns of cannabis use for medicinal and non-medicinal purposes in the context of possible policy change [25].
For the purposes of this study, relevant questions assessed six areas:
1) Demographics (sex, age, living situation (state and metropolitan, rural or remote) and employment status (full-time or part-time));
2) General wellbeing and health (qualitative assessment of any health conditions affecting day-to-day life and whether or not the condition was ongoing);
3) Any cannabis (ever use, age of onset, past month frequency of any use in days, quantity of use per day of use in cones, joints or grams, experienced and preferred routes of administration);
4) Medicinal cannabis use (qualitative assessment of health conditions, check-list on ever use, reasons for use, experienced and preferred routes of administration, effect on health conditions (11 point Likert scale rating improvement), past month frequency of use in days and quantity used per day of use, history of use (less than one year, 1-5 years, 6-10 years, more than 10 years));
5) Knowledge of medicinal cannabis (qualitative assessment of the participant’s knowledge of medicinal cannabis laws and the extent of their support for these laws (11 point Likert scale), qualitative assessment of the health conditions the participant feels are effectively treated by cannabis, how they obtained this knowledge (personal experience, friend recommendation, personal research, health professional, other recommendation) and the extent that they believe the scientific evidence supporting the use of medicinal cannabis for spasticity, cancer, chemotherapy, nausea, problems sleeping, and low mood (all 11 point Likert scales)).
6) The sixth area assessed perceptions of medical cannabis and included the participants’ support for policy (11 point Likert scales on legalisation and access for personal use for recreational purposes and qualitative assessment of any final thoughts); thoughts on access (who should have access (no restriction, doctor prescription, clinical trial participants, all adults, those with a particular health condition, government regulated special access, or other), approval of weekly use for medicinal and recreational purposes and degree of preference for the requirement of Therapeutic Goods Administration approval (all ten-point Likert), qualitative assessment of who would be responsible for growing the cannabis, preferred form (smoked, oil, tablet, oral spray, baked product, liquid, other) and source (myself, friend, private company, public company, other)); harms related to legalising access (qualitative assessment of what harms there may be, harms relating to production and regulation by the government, harms relating to daily use for medical and non-medical use, side-effects from medicinal use, and opinions on regulation) and research (extent of support for further clinical trials (ten-point Likert) and qualitative assessment of support or opposition for further clinical trials).
Participants were categorised as a non-user (NU), recreationalonly user (RU), medicinal-only user (MU), or combined user (recreational and medicinal; CU) through analysis of questions assessing ever use, days of use for medicinal and recreational purposes, and a purpose built checklist (I have only ever used cannabis for non-medicinal purposes, I use for non-medicinal purposes although have previously used for medicinal purposes, I usually use for nonmedicinal purposes but I also sometimes use for medicinal purposes, I usually use for medicinal purposes but I also sometimes use for non-medicinal purposes, I use for medicinal purposes although I have previously used for non-medicinal purposes, I have only ever used for medicinal purposes). The full survey and was expected to take approximately 20 minutes to complete.
Data analysis
Qualitative data from open ended responses was coded and organized by two independent researchers into categories using open coding thematic analysis and reported as themes. Discrepancies were discussed until objective consensus was reached. Reported health conditions were categorised according to the International Classification of Diseases, 10th revision (ICD-10) [39].
Differences in categorical demographic information were analysed by χ2 using IBM SPSS Statistics, Release Version 22, with the rest of statistical analysis undertaken using Stata 13.1 (Statacorp). Significance was defined as P < 0.05. Due to clustering of responses at polar ends of the Likert scale questions, these were converted to binary responses for analysis although mean and interquartile range (IQR) is reported. Additionally, as gender and age groups were unbalanced across non-users and groups by cannabis use motivation, we conducted logistic regression analyses predicting responses according to cannabis use status only (crude OR), and status controlling for age and gender (adjusted OR). In cases where linearity was violated, age was adjusted according to box-tidwell output and where this adjustment could not be made, age was entered as a categorical variable (See Table Notes). Odds ratio and 95% confidence interval results are reported according to the ruleof-4 approach [40]. Marginal estimated means (MEM) from adjusted models are also reported (age and gender held constant).
Results
No significant demographic differences were found between those who completed or did not complete the survey with the exception of age. Those under 26 years were significantly more likely to not complete the survey (χ2 (5) = 57.21, P < 0.001; +7.4 Adj. standardised residual).Demographics
Demographic details of the 1578 participants who completed the survey are presented in Table 1. Also provided in this Table 1 is Australian population data as published by the Australian Bureau of Statistics (ABS) from June 2015 and employment status as at July 2016 [41,42]. Region was surveyed using the Rural, Remote and Metropolitan Areas (RRMA) classification, however; in the absence of complete Australian data by region using this classification, approximate comparisons were made using the Australian Statistical Geography Standard (ASGS) collected by the ABS as at July, 2016 [43]. Overall the survey respondents were comparable to the Australia population with the exception of over representing those aged younger than 26 years, underrepresenting those over 65 years and over representing those in remote locations. Gender was not evenly distributed by age group, as males were overrepresented under the age of 36 years (χ2 (5) = 127.41, P < 0.001; adj. res +7.4, +5.7) and females overrepresented from age 36 to 64 years (adj. res +3.4, +4.9, +6.1).General well-being and health
Upon open ended questioning regarding any health conditions, participants most commonly reported a pain condition or felt symptoms of pain. Males tended to report musculoskeletal issues, while females tended to report arthritis and mood disorders. Regarding the reporting of any health condition, compared to nonusers (MEM 51.6%), recreational users were less likely to report a health condition (adjusted OR 0.465 [0.318 - 0.679] MEM 33.1%) while combined (adjusted OR 1.75 [1.21 - 2.53] MEM 65.1%) and medicinal-only users (adjusted OR 3.58 [1.82 - 7.06] MEM 79.3%) were significantly more likely (all P < 0.001). Males were less likely than females to report any health condition (OR 0.64 [0.52 - 0.80] P < 0.001) and the likelihood of reporting any health condition increased with participant age (OR 1.53 [1.43 - 1.64] P < 0.001). Medicinal and combined cannabis users were asked whether their reported health condition was diagnosed and if they were seeing a doctor for the condition, with medicinal users three times more likely to confirm this was the case (MEM 92.5% and 76.9% compared to 80.3% and 50.1%; adjusted OR 3.01 [1.18 - 7.67] and 3.32 [1.81 - 6.09]).
Cannabis use
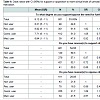
The majority of the sample reported some form of cannabis use (87.39%) and this was most likely to be combined use (both medicinal and recreational; 51.20%) or recreational use (31.99%) with just 5.20% of participants reporting medicinal-only use. As shown in Table 2 motivations for cannabis use differed by gender and age. Non-users were significantly more likely than average to be female and older. Both recreational users and combined users were more likely to be younger while combined users tended to also be male. In contrast, medicinal only users were more likely to be older.Differences in patterns of cannabis use by cannabis use motivation are shown in Table 3. As compared to recreational users, combined users were younger at their average age of use onset, although both groups were likely to initiate use in their teenage years. In contrast, medicinal users were more likely to initiate use in their early twenties. Compared to recreational users, medicinal and combined users were more likely to have ever used regularly, although combined users were also more likely than medicinal users to have used regularly. Similarly, combined users were more likely to report daily recreational use in the past 28 days compared to recreational users. Moreover, combined users were more likely to use more than one gram on a typical day of use as compared to recreational users, and were more likely to have tried more than three separate routes of cannabis administration. In contrast, when asked about any past month cannabis use, medicinal users were the most likely to have used daily.Patterns of medicinal cannabis use
As detailed in Table 4, medicinal users were significantly more likely than combined users to report daily medicinal use in the past 28 days although used a similar quantity of grams per day of use and reported using cannabis for a comparable length of time. Approximately two thirds of those reporting any medicinal cannabis use reported that their symptoms were much improved following use.Upon open ended questioning, the most commonly reported reason for medicinal cannabis was for pain relief followed by mental health concerns (including anxiety and depression). Cannabis was also commonly used to provide assistance with sleeping and appetite. There did not appear to be any trend in reasons for use between combined and medicinal-only users with the exception that combined users tended to be more likely to use cannabis for anxiety. When asked to report any associated difficulty with use, participants reported physical side effects (drowsiness, hunger, weight gain, respiratory concerns, nausea, unpleasant feelings) and psychological effects (anxiety, paranoia, loss of motivation, poor memory, hallucinations and depression) most commonly, followed by sociological issues (work/driving interference, stigma, financial concerns) and other issues (strain and dose inconsistencies, withdrawal, dependence and drug interactions).
Knowledge and perceptions of medicinal cannabis use
The total sample most commonly reported gaining their knowledge on medicinal cannabis from personal research. This was particularly the case for combined and medicinal-only users compared to non-users (MEM 59.9% and 64.7% compared to 49.0%; adjusted OR 1.55 [1.12 - 2.15] and 1.90 [1.12 - 3.24]). Non-users were more likely to use news sources as information (MEM 59.4%) compared to recreational (MEM 44.7%, OR 0.55 [0.39 - 0.78]), combined (MEM 28.6%, OR 0.27 [0.20 - 0.39]) and medicinal-only users (MEM 20.8%, OR 0.18 [0.10 - 0.33]). While few participants sourced information from health professionals, medicinal-only users were most likely to do so (MEM 28.9% compared to 18.1% of nonusers, 11.9% recreational users, and 16.7% combined users).
When asked about knowledge of the current state of medical cannabis in Australia, a minority of participants were aware that they could be prescribed cannabinoid pharmaceuticals for multiple sclerosis related spasticity in Australia (MEM 18.8% of non-users, 23.0% of recreational users, 23.3% of combined users, and 16.2% of medicinal-only users). However, most had heard of new cannabis laws, particularly medicinal users compared to non-users (MEM 87.7% compared to 75.7%, OR 2.29 [1.10 - 4.80]). The majority completely supported these new laws, particularly those reporting recreational use as compared to non-users (MEM 80.4% compared to 66.9%, OR 2.03 [1.37 - 3.01]). When prompted using open ended questioning to describe what they believed these new laws were, very few participants were able to accurately describe that the change in legislation which came at the time of survey allowed for cannabis to be grown for medicinal and research purposes. In contrast, many incorrectly believed that this change was relating to legalising medicinal cannabis under various restrictions (such as under prescription, or only for those with specific serious illnesses such as cancer, epilepsy and pain). Other participants described the legalisation of cannabis trials and/ or commercial or private growing without further detail. Finally, a minority believed that use of cannabis for all medicinal purposes was made legal.
When asked about how firm they believed the scientific evidence was for a number of provided conditions, medicinal users were consistently more likely than recreational and non-users to believe the evidence was firm (Table 5). In the cases of muscle spasticity, chemotherapy-related side effects, sleeping problems and low mood, medicinal-only users were more likely to believe the evidence was firm compared to combined users. As compared to non-users, recreational users were more likely to believe the evidence was firm was regarding the treatment of sleeping problems and nausea.On open ended questioning, the participants most commonly reported that cannabis was known to treat pain, seizures and cancer. Combined and medicinal-only users tended to be more likely to cite mental health conditions (particularly anxiety and depression) and insomnia, while recreational cannabis users were similar to non-users with the exception of an increased likelihood of citing appetite, insomnia and glaucoma. Notably, an important minority of participants, especially combined and medicinal users, reported that cannabis could treat multiple conditions (responding “too many to list”, “numerous” or “many”).
There were significant differences in preferred preparations by cannabis use motivation. Compared to non-users, cannabis users were most likely to prefer smoked cannabis that is no different to non-medical cannabis (MEM 43.4% of combined users, 22.9% medicinal-only users, and 27.6% of recreational users compared to 8.2% of non-users; OR 8.5 [4.7 - 15.5], OR 3.31 [1.48 - 7.44] and OR 4.2 [2.3 - 7.8], respectively). In contrast, tablets were preferred by non-cannabis users compared to other groups (MEM 29.6% compared to 5.2% of combined users, 9.7% medicinal-only users, and 18.9% of recreational users; OR 0.130 [0.084 - 0.202], OR 0.255 [0.123 - 0.529], OR 0.56 [0.38 - 0.82], respectively). Support for a liquid form of cannabis (similar to cough syrup), tinctures, oral sprays, and vaporizers were low and not different between groups.
When asked to rate support for clinical trials of medicinal cannabis, support was higher among recreational and combined cannabis users compared to non-users although significantly low among medicinal users compared to recreational users (Table 6). Those reporting reasons for their support of further trials (54.56%; n = 861) most commonly reported an interest in gaining more knowledge or a desire that the effectiveness of medicinal use be better demonstrated. Those reporting reasons for opposition of further trials (26.05%; n = 411) most commonly detailed that there was already sufficient research and further research would be redundant or that more research was not preferable to immediate legalisation. Reasons for opposition were more likely to be given by combined and medicinal users compared to non-users and recreational users.
Discussion
This study presents the results from the largest and most in-depth survey of Australian’s opinions, beliefs and use of medicinal cannabis. The first important finding was the scarcity of individuals reporting medicinal-only use (5.20%) as compared to those also reporting recreational use (‘combined users’; 51.20%). In line with previous research, we identified that only approximately one in ten who reported medicinal cannabis use does not report additional recreational cannabis use [31]. This difference in cannabis use motivation was a significant factor in predicting patterns of cannabis use and perceptions of medicinal cannabis use. First, combined users were more likely to use cannabis regularly and reported more frequent recreational use at greater quantities, in addition to supporting the regular use of cannabis-even compared to those who only used cannabis for recreational purposes. In contrast, those using for medicinal-only purposes were the most likely to report daily cannabis use. Second, those reporting any recreational use were more likely to be younger than those reporting medicinal use only and more likely to begin using cannabis before they were 18 years old. In addition, those reporting combined use were more likely to be male than other groups. These patterns of use indicate that combined users, who make up the vast majority of medicinal users, represent a distinct subpopulation separate from both recreational-only and medicinal-only users and who have more frequent recreational use than recreational-only users. This is an important finding as previous population surveys regarding medicinal cannabis use typically collapse combined users with medicinal only users [26-31]. Moreover, while the majority of Australians support medicinal cannabis use, they do not support recreational cannabis use [6].Participants were most commonly treating pain conditions with cannabis followed by mental health conditions (including anxiety, depression and other non-mood disorders) and then insomnia. Combined users were particularly likely to use cannabis to treat anxiety. These conditions have been identified as targets for medicinal cannabis use in previous Australian research, however; treating mental health conditions with cannabis does not seem to be as prevalent in the US or Canada [25-31]. While there are mechanisms by which cannabis may alleviate low mood at least in the short term, this finding is particularly concerning given established links between early onset and long term cannabis use and worsened mental health [44-46]. Moreover, combined users were less likely to have had their health conditions diagnosed by a health professional indicating that cannabis may be used as an alternative to medical assessment and treatment. As such, it may be of some benefit to encourage contact with the medical system through future regulatory models.
The majority of the sample reported gaining knowledge on medicinal cannabis use from personal research and experience, with few reporting having spoken with a health professional. The findings revealed a serious lack of knowledge of the evidence base for medicinal cannabis and recent legislative changes. First, when asked to describe the current state of medicinal cannabis use in Australia, the vast majority were unable to accurately describe the recent changes to legislation allowing for the cultivation of cannabis for medicinal or scientific purposes. Second, the full sample consistently believed that there is firm evidence for cannabis as a treatment for pain, spasticity, cancer, side effects of chemotherapy, sleeping problems, low mood, and nausea. In contrast, the evidence is not thought to be firm for any of these conditions, particularly for sleeping problems and low mood [47,48]. Third, when the sample was asked to provide conditions for which cannabis was thought to treat, many respondents replied that the list was too long and numerous to be provided. Finally, a minority of respondents opposed clinical trials of medicinal cannabis use, including almost half of medicinal-only users. When asked their reasons for this opposition, participants frequently cited that conducting further research would be redundant as the evidence for the effectiveness of medicinal cannabis is already clear. As such there is an obvious need to increase efforts to educate the public, and particularly those already using cannabis for medicinal purposes, as to the current state and poor quality of the current evidence base [48].
Under the current regulatory model in Australia, general practitioners will become the gatekeepers of medicinal cannabis prescription. This survey indicates that those seeking medicinal cannabis from their general practitioner may present with:
1) Health conditions that do not have currently strong evidence base for treatment with cannabis;
2) A long history of cannabis use which may require screening for underlying health conditions and related problems;
3) A firm belief on the benefits of medicinal cannabis established through personal research which may need to be addressed with reference to the importance of research quality; and
4) A disengagement from the medical system which may place an initial strain on clinical rapport. Each of these factors is likely to be challenging in a clinical setting and strategies and guidelines for general practitioners to improve engagement with these patients are yet to be developed.
In contrast, the much smaller group of patients without a history of recreational cannabis use may be more easily integrated into the current regulatory system, given their increased engagement with medical professionals and preference for non-inhalation routes of administration which are similar to typical pharmaceutical medications.
In summary, the results from this non-representative but large survey provides an increased understanding regarding the differences between non-users and current medicinal and non-medicinal cannabis users in the perceptions of risk and views on the medicinal use of cannabis in Australia. Notably, the use of cannabis only for medicinal purposes was rare in this sample and they consistently supported the use of cannabis for medicinal purposes, citing its effectiveness in treating pain and mental health conditions in particular, but also reporting a belief in effectiveness for treating a great number of other health conditions. Participant knowledge was inconsistent with the current evidence base and likely to come from personal research and experience as opposed to consultation with health professionals. This pattern of results indicates a general resistance to scientific and medical literature which may lead to a reduced rapport in clinical settings. The need for national clinical guidelines is paramount given the stark contrast between the current state of low to moderate evidence for medicinal cannabis and the overwhelming enthusiasm by the public in general and particularly by current cannabis users.
References
- D'Souza DC, Ranganathan M (2015) Medical marijuana: Is the cart before the horse? JAMA 313: 2431-2432.
- Grant I, Atkinson JH, Gouaux B, Wilsey B (2012) Medical marijuana: clearing away the smoke. Open Neurol J 6: 18-25.
- Martin JH, Bonomo Y (2016) Medicinal cannabis in Australia: the missing links. Med J Aust 205: 425.
- Matthew-Simmons F, Sunderland M, Ritter A (2013) Exploring the existence of drug policy 'ideologies' in Australia. Drugs 20: 258-267.
- Williams J, van Ours JC, Grossman M (2011) Why do some people want to legalize cannabis use? National Bureau of Economic Research, Cambridge, USA.
- Australian Institute of Health and Welfare (2014) National Drug Strategy Household Survey Report: 2013 Drug statistics series no. 28, Cat. no. PHE 183, AIHW, Canberra, Australia.
- Room R (2014) Legalizing a market for cannabis for pleasure: Colorado, Washington, Uruguay and beyond. Addiction 109: 345-351.
- Government NSW (2016) Terminal Illness Cannabis Scheme.
- Hadland SE, Knight JR, Harris SK (2015) Medical marijuana: review of the science and implications for developmental-behavioral pediatric practice. J Dev Behav Pediatr 36: 115-123.
- Hill KP (2015) Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA 313: 2474-2483.
- Copeland J, Clement N (2014) The use of cannabis for medical purposes. National Cannabis Prevention and Information Centre, Sydney, Australia.
- Parmar JR, Forrest BD, Freeman RA (2016) Medical marijuana patient counseling points for health care professionals based on trends in the medical uses, efficacy, and adverse effects of cannabis-based pharmaceutical drugs. Res Social Adm Pharm 12: 638-654.
- Rosenberg K (2015) Medical cannabis effective for chronic pain, other indications. Am J Nurs 115: 53.
- Sznitman SR, Bretteville-Jensen AL (2015) Public opinion and medical cannabis policies: examining the role of underlying beliefs and national medical cannabis policies. Harm Reduct J 12: 46.
- Gurley RJ, Aranow R, Katz M (1998) Medicinal marijuana: a comprehensive review. J Psychoactive Drugs 30: 137-147.
- Joy JE, Watson SJ, Benson JA (1999) Marijuana and medicine: assessing the science base. National Academy Press, Washington, DC, USA.
- Mathre ML (1997) Cannabis in medical practice: a legal, historical and pharmacological overview of the therapeutic use of marijuana. McFarland & Company, Inc., publishers, Jefferson, North Carolina.
- Hill KP (2014) Medical marijuana: more questions than answers. J Psychiatr Pract 20: 389-391.
- The National Academies of Sciences, Engineering, and Medicine (2017) The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. The National Academies Press, Washington, DC, USA.
- Ablin J, Ste-Marie PA, Schafer M, Hauser W, Fitzcharles MA (2016) Medical use of cannabis products: Lessons to be learned from Israel and Canada. Schmerz 30: 3-13.
- Bestrashniy J, Winters KC (2015) Variability in medical marijuana laws in the United States. Psychol Addict Behav 29: 639-642.
- Lucas PG (2008) Regulating compassion: an overview of Canada's federal medical cannabis policy and practice. Harm Reduct J 5: 5.
- Belackova V, Ritter A, Shanahan M, Chalmers J, Hughes C, et al. (2015) Medicinal cannabis in Australia - framing the regulatory options. Drug Policy Modelling Program, National Drug and Alcohol Research Centre, Syndey, Australia.
- Chapman SA, Spetz J, Lin J, Chan K, Schmidt LA (2016) Capturing heterogeneity in medical marijuana policies: a taxonomy of regulatory regimes across the United States. Subst Use Misuse 51: 1174-1184.
- Swift W, Gates P, Dillon P (2005) Survey of Australians using cannabis for medical purposes. Harm Reduct J 2: 18.
- Boyd CJ, Veliz PT, McCabe SE (2015) Adolescents' use of medical marijuana: a secondary analysis of monitoring the future data. J Adolesc Health 57: 241-244.
- Davenport SS, Caulkins JP (2016) Evolution of the United States marijuana market in the decade of liberalization before full legalization. J Drug Issues 46: 411-427.
- Lin LA, Ilgen MA, Jannausch M, Bohnert KM (2016) Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addict Behav 61: 99-103.
- Ogborne AC, Smart RG, Adlaf EM (2000) Self-reported medical use of marijuana: a survey of the general population. CMAJ 162: 1685-1686.
- Ryan-Ibarra S, Induni M, Ewing D (2015) Prevalence of medical marijuana use in California, 2012. Drug Alcohol Rev 34: 141-146.
- Schauer GL, King BA, Bunnell RE, Promoff G, McAfee TA (2016) Toking, vaping, and eating for health or fun: marijuana use patterns in adults, U.S., 2014. Am J Prev Med 50: 1-8.
- Colorado Department of Public Health and Environment (2016) Medical Marijuana Registry Program Statistics. Colorado Department of Public Health and Environment.
- Sabet K, Grossman E (2014) Why do people use medical marijuana? the medical conditions of users in seven U.S. states. J Glob Drug Policy Pract 8: 1-26.
- Clark AJ, Ware MA, Yazer E, Murray TJ, Lynch ME (2004) Patterns of cannabis use among patients with multiple sclerosis. Neurology 62: 2098-2100.
- Furler MD, Einarson TR, Millson M, Walmsley S, Bendayan R (2004) Medicinal and recreational marijuana use by patients infected with HIV. AIDS Patient Care STDS 18: 215-228.
- Waissengrin B, Urban D, Leshem Y, Garty M, Wolf I (2015) Patterns of use of medical cannabis among Israeli cancer patients: a single institution experience. J Pain Symptom Manage 49: 223-230.
- McDermott A (2014) What is the average CTR on Facebook ads?
- Thornton LK, Harris K, Baker AL, Johnson M, Kay-Lambkin FJ (2016) Recruiting for addiction research via Facebook. Drug Alcohol Rev 35: 494-502.
- World Health Organisation (2016) International statistical classification of diseases and related health problems, 10th Revision (ICD-10).
- Cole TJ (2015) Setting number of decimal places for reporting risk ratios: rule of four. BMJ 350: h1845.
- Australian Bureau of Statistics (2017) Labour force, Australia.
- Australian Bureau of Statistics (2016) Population by age and sex, regions of Australia.
- Australian Bureau of Statistics (2016) Australian Statistical Geography Standard (ASGS): Volume 1 - Main structure and greater capital city statistical areas.
- Witkin JM, Tzavara ET, Nomikos GG (2005) A role for cannabinoid CB1 receptors in mood and anxiety disorders. Behav Pharmacol 16: 315-331.
- Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, et al. (2014) The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med 44: 797-810.
- Yurasek AM, Hadley W (2016) Commentary: Adolescent marijuana use and mental health amidst a changing legal climate. J Pediatr Psychol 41: 287-289.
- Gates PJ, Albertella L, Copeland J (2014) The effects of cannabinoid administration on sleep: a systematic review of human studies. Sleep Med Rev 18: 477-487.
- Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, et al. (2015) Cannabinoids for medical use: a systematic review and meta-analysis. JAMA 313: 2456-2473.