Journal of Surgery
Download PDF
Case Report
Foreign Body Removal in Indian Patient after 18 Years of Ingestion
AlBahrani Z1*, Busbaih Z2, Busbaih J3 and BusbaihA4
- Department of Surgery, University of King Faisal, KSA
- Department of Surgery, Prince Soud bin Jalawi Hospital, KSA
- Department of Medicine, King Fahad Hofuf Hospital, KSA
- Department of dentistry primary health care, KSA
*Address for Correspondence: AlBahrani, Department of Surgery, University of King Faisal, AlAhsa, KSA, Tel: +966-54-099-9882; Fax: +966 13 8442244; E-Mail: zyn990@gmail.com
Citation: AlBahrani Z, Busbaih Z, Busbaih J, Busbaih A. Foreign Body Removal in Indian Patient after 18 Years of Ingestion. J Surgery. 2018;6(1): 2.
Copyright: © 2018 AlBahrani Z, et al. This is an open access articledistributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Surgery | ISSN: 2332-4139 | Volume: 6, Issue: 1
Submission: 14, February 2018| Accepted: 26, March 2018 | Published: 30, March 2018
Abstract
Exploratory laparotomy is considered as the conventional management procedure for acute abdominal issues. It can cause paralytic ileus and may lead to abdominal wall dehiscence. Few cases of lump ingestion have been reported in scientific literature. Here we report removal of a foreign body (an electric lamp) from patient abdomen who developed perforated Viscous following exploratory laparotomy. The patient was admitted with abdominal pain and constipation and later diagnosed with Foreign Body (FB) ingestion by computed tomography C.T. scan of the abdomen and pelvis. The patient underwent FB sigmoid removal and closure was done.
Keywords
Foreign body; Laparoscopy; Exploratory laparotomy; Electric lamp; Perforation; Acute Abdomen; Indian
Introduction
Exploratory laparotomy is a traditional procedure involving incision through abdominal wall to gain access into the abdominal cavity. The use of laparotomy for foreign body extraction resulted in a statically significant survival benefit Compared with laparoscopy alone for foreign body removal can reduce recovery period but it is not appropriate in all times. Prolonged ileus due to laparotomy has been reported in 7.5 % Wound dehiscence 2.9% was unlikely with our case with low risk index [1,2]. Recovery time typically takes approximately 6 weeks, however walking during this period recommended to reduce chest infection and blood clots formation. Prophylaxis against VTE is routinely advised by Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) for more than 1 week. We report a case with lamp ingestion from childhood and extracted after 18 years when he developed complications.
Case Report
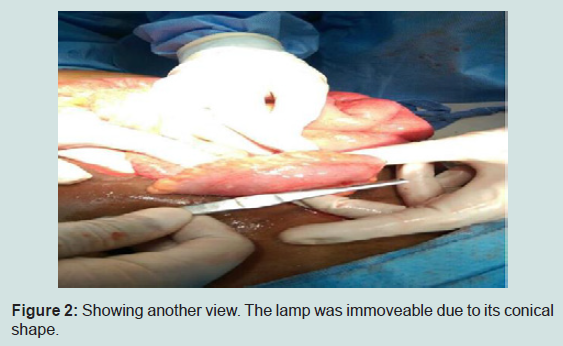
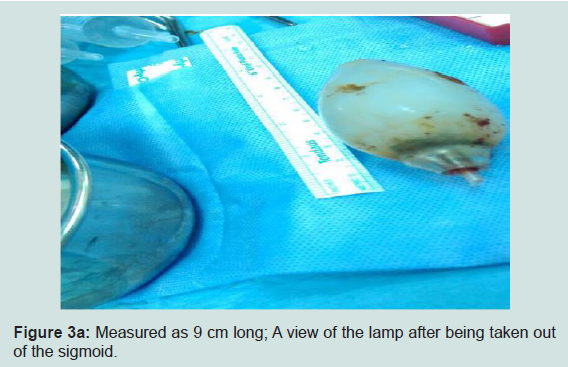
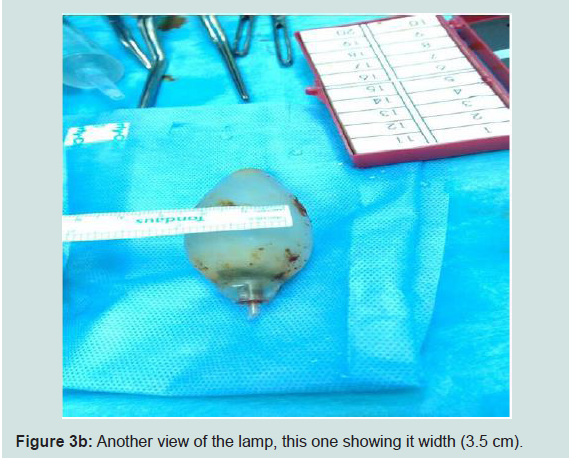
28 years old Indian male was admitted with worsening abdominalpain for 5 days that was progressively increasing in intensity and severity without any vomiting. Last day before admission, patient develop constipation and generalized abdominal pain, Obstipation and distention. He was diagnosed with acute perforated viscous due to foreign body at sigmoid showed by CT scan. Patient described a history of his lamp ingestion when he was child, aged 10 years, playing challenge with other 2 kids, one of the kids, he informed, was died immediately as result of the foreign body stuck in esophagus leads to suffocation. He didn’t consult anyone because he was afraid from his father and he didn’t get any symptoms at that time. The case was discussed with surgery team and decision was taken to do explaratory laparotomy. Patient scheduled for procedure, FB removal and primary anastomosis was done. Patient’s supine, G.A induced, usual preparation and dripping, Midline incision done, opening of rectal sheeth, there was fluid collection and pus with ½ cm perforation at the sigmoid area where the foreign body was found (Figures 1 and 2). Extraction of FB (lamp) was done. This was a conical shaped glass lamp without its metal base; only glass which is can stay in stomach without being affected by gastric contents. We understand that there is a place where foreign body will stuck at some points in the bowel like; pylorus, duodenum and ileocecal junction valve. Another point which is in the sacral prominence area. During intraoperatively it was measured 9x3.5 cm in size, the diameter 3.5 cm; that means it truly passing lamp since he developed symptoms when it start moving from stomach to sigmoid area. (Figures 3a and 3b), remained immovable through bowel for a long period of time. And because 1.5 cm sharp point that’s get stuck in the sacral prominancy from scientific point of view and that is why it makes perforation in that area, sigmoid area. The perforation was cleaned and the area was flushed with normal saline. GI closed with staplers, sutured closure of rectal sheeth, the wound has been closed in layers. The surgical procedure lasted for 75 minutes. Patient discharged after 7 days post-surgery with good condition with direction to follow-up with OPD 2 weeks later, He recovered well.
Discussion
Exploratory Laparotomy is the classical procedure used in the management of acute perforated viscous and for foreign body removal. As a rule, it has also been used to determine the nature of an illness, stage of a disease process and to determine the cause of blockage of intestine. It is generally well-tolerated procedure and its main risks include infection, incisional hernia and bleeding from surgical site. Adhesive intestinal obstruction, a less common complication, is reported in 3% of all laparotomies [3]. However, it is also associated with Enterocutaneous fistula [4]. In patient with perforated viscous, Intra-abdominal collection or abscess is an important complication. Drainage is the main stay to treat this abscess. However, laparoscopy contribute to bleeding 10 % [5], and also low risk of infection 1.1% [6]. The literature reveals many reported instances of intra abdominal foreign body removal managed by laparoscopy, as well as one report described [7,8]. The World Society of Emergency Medicine (WSES) recommends if the area of perforation cannot be localized laparoscopically, the surgeon should begin with a laparotomy before proceeding further. In some other studies 1 to 14 % patient will need surgery in the presence of complications [9]. Hence our patient had generalized purulent peritonitis, given the feasibility of organ failure we interfered with exploratory laparotomy. Foreign body ingestion is not uncommon in Indians (58.33%) with male predominance 78.94%) belonged to low socioeconomic status as well as our patient came from rural area with poor health service [10]. It is reported that patients with retained foreign body for 10 years who were observed, had increased rate of morbidity 50%. The median overall mortality rate was 10 % [11]. Our patient had significant acute abdomen, presented with perforation not SBO and an initial endoscopic examination could not be performed. However, in light of radiological and clinical findings, peritonitis was suspected confirmed by CT scan so surgical intervention was started. After 2 weeks of treatment, the patient improved, and the perforation resolved.
Conclusion
Patient with retained lamp in abdomen ultimately will present in very serious complications with high rates of morbidity and mortality. Despite this being a rare situation and the case saved with surgery, advice to bring education for foreign body ingestion in health relatedissues, prevention remains the key to the problem.
References
- Kirchhoff P, Clavien PA, Hahnloserg D (2010) Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg 4: 5.
- Kenig J, Richter P, Żurawska S, Lasek A, Zbierska K (2012) Risk factors for wound dehiscence after laparotomy - clinical control trial. Pol Przegl Chir 84: 565-573.
- Duron JJ, Silva NJ, du Montcel ST, Berger A, Muscari F, et al. (2006) Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg 244: 750-757.
- Galie KL, Whitlow CB (2006) Postoperative enterocutaneous fistula: when to reoperate and how to succeed. Clin Colon Rectal Surg 19: 237-246.
- Kaushik R(2010) Bleeding complications in laparoscopic cholecystectomy: Incidence, mechanisms, prevention and management. J Minim Access Surg 6: 59-65.
- Gupta R, Sample C, Bamehriz F, Birch DW (2006) Infectious complications following laparoscopic appendectomy. Can J Surg 49: 397-400.
- Chin EH, Hazzan D, Herron DM, Salky B (2007) Laparoscopic retrieval of intraabdominal foreign bodies. Surg Endosc 21: 1457.
- Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, et al. (2016) Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 48: 489-496.
- Chia DK, Wijaya R, Wong A, Su-Ming T (2015) Laparoscopic management of complicated foreign body ingestion: a case series. Int Surg 100: 849-853.
- Gupta Y, Gourh G, Mundra RK (2015) Retrospective study of upper digestive tract foreign bodies in central India. Int Surg JISJ 2: 539-543.
- Gonzalez-Ojeda A, Rodriguez-Alcantar DA, Arenas-Marquez H, Sanchez Perez-Verdia E, Chavez-Perez R, et al. (1999) Retained foreign bodies following intra-abdominal surgery. Hepatogastroenterology 46: 808-812.