Journal of Clinical and Investigative Dermatology
Melasma and Common Pigmentary Dermatoses in Asian Individuals and an Overview of Their Treatment
Kyoung-Chan Park* and Soon-Hyo Kwon
- Seoul National University College of Medicine, Seoul National University Bundang Hospital, Korea
*Address for Correspondence: Kyoung Chan Park, Department of Dermatology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, 300 Gumi-dong, Bundang-gu, Seongnam-si, Gyeonggi-do 463-707, Korea, Tel: + 82-31-787-7311; Fax: + 82-31-787-4058; E-mail: gcpark@snu.ac.kr
Citation: Kwon SH, Park KC. Melasma and Common Pigmentary Dermatoses in Asian Individuals and an Overview of Their Treatment. J Clin Investigat Dermatol. 2014;2(1): 8.
Copyright © 2014 Park et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Investigative Dermatology | ISSN 2373-1044 | Volume: 2, Issue: 1
Submission: 19 November 2013 | Accepted: 23 January 2014 | Published: 27 January 2014
Reviewed & Approved by: Dr. Shasa Hu, Assistant Professor in the Department of Dermatology and Cutaneous Surgery at University of Miami, USA.
Abstract
Asian patients with Fitzpatrick skin types III-V have been highlighted in publications describing pigmentary dermatoses. Melasma is particularly common in Asia, while nevus of Ota, acquiredbilateral nevus of Ota-like macules (ABNOM), and Mongolian spots are also frequently seen. In Asian individuals, postinflammatory hyperpigmentation (PIH) frequently occurs after the treatment, especially laser and light therapies. Thus, prevention and management of PIH are extremely important concerns. This review discusses the pigmentary dermatoses commonly encountered in Asia, including melasma, ABNOM, nevi of Ota and Ito, and Mongolian spots, and the various treatment options that are either currently available or under investigation in vitro.Keywords
Acquired bilateral nevus of Ota-like macules; Asian individuals; Melasma; Mongolian spot; Nevus of Ota; Pigmentary dermatosisIntroduction
Pigmentary skin disorders are of great concerns among Asian patients. This could be attributed to an increased interest on their skin conditions observed in Asian women. The exponential growth in the market of cosmetic procedures in Asia has exacerbated this trend. As a rapid increase in the populations is expected in Asian countries, pigmentary skin disorders in Asian individuals and their treatment will receive more attention over the next several decades.Melasma
Melasma is an acquired hypermelanosis characterized by symmetrical, irregular light-to-dark-brown macules and patches on sun-exposed area, especially on the face. It is common among Asian and Hispanic women during their third and fourth decades of life [1]. A genetic predisposition, chronic exposure to ultraviolet (UV) radiation, and female sex hormones are typically considered to play main roles in its pathogenesis [2-5]. Histopathological findings include epidermal hyperpigmentation accompanied by an increased number of melanocytes, overexpression of melanogenic enzymes, and overlying dermal changes [6].Topical treatment agents
Niacinamide (vitamin B3) and melanosome transfer inhibitors: A reduction in melanosome transfer from melanocytes to keratinocytes results in hypopigmentation by blocking the dispersion of pigment to the keratinocytes. A serine protease inhibitor has been reported to modulate the activation of the protease-activated receptor 2, resulting in the accumulation of melanosomes within melanocytes in vitro [41,42]. Lectins and neoglycoproteins have also been shown to reduce melanosome transfer in vitro [43]. Hakozaki et al. (2002) demonstrated that niacinamide suppresses melanosome transfer in vitro, and in a split-face trial, showed that 5% niacinamide cream significantly reduced hyperpigmentation and lightened basal skin color in eight weeks [44] (p<0.05).
Other compounds: Topical application of linolenic acid, linoleic acid, oleic acid, and phospholipase D2 resulted in hypopigmentation of the skin of guinea pigs after UV irradiation via the stimulation of tyrosinase ubiquitination and proteasomal degradation [45-48].
Several compounds that modify tyrosinase structures at glycosylation sites have been found to induce hypopigmentation in vitro, including glucosamine, tunicamycin, and calcium D-pantetheine-S-sulfonate [49,50].
Laser and light therapies
Intense-pulsed light therapy: Intense-pulsed light (IPL) therapy emits a broad spectrum of wavelengths with a cutoff shorter than the filter, and provides selective photothermolysis [51]. Li et al. (2008) evaluated the efficacy and safety of IPL treatment in 89 Chinese patients with melasma. After four treatment sessions with threeweek intervals, significant reductions in the mean Melasma Area and Severity Index (MASI) score, from 15.2 to 5.2 (p<0.05), and in the melanin index, from 140.8 to 119 (p<0.05) were found [52]. In this study, transient erythema and edema were the most common adverse events, and three patients experienced PIH.
Although IPL is a good therapeutic option for melasma with promising results reported, melasma-like pigmentation following IPL treatment usually occurs, which is even more intensely pigmented than the melasma it treats. Laser energy induces hyperactive melanocytes through inflammation, increases prostaglandin and cytokine production in keratinocytes and fibroblasts, and disrupts the basement membrane. As a result, a mixture of PIH and aggravated melasma lesions forms [53,54]. Since subtle melasma is clinically invisible to the naked eye but is detected by UV photography in 28.3% of Asian patients, IPL treatment must be performed with caution [55].
Fractional 1,550-nm non-ablative laser therapy: Fractional photothermolysis creates numerous microthermal zones (MTZ) of thermal injury in the skin, while leaving the areas between them unaffected. Transepidermal elimination of the MTZ could effectively remove dermal melanophages [56]. The unaffected areas may cause a more rapid recovery and theoretically, lower the risk of subsequent inflammation and PIH.
In a small clinical trial involving four-to-six sessions of fractional non-ablative laser treatment with one-to-two-week intervals, six out of 10 patients with Fitzpatrick skin types III-V achieved 75-100% clearance of the lesion, with PIH occurring in one patient [57]. In contrast, a split-face study comparing fractional non-ablative laser treatment with TCC, found a significant worsening of pigmentation measured by a Mexameter® (p<0.05) and a higher incidence of PIH (31%) in the laser-treated group [58]. However, in a similar eightweek trial performed by the same investigators, the study groups treated with either fractional non-ablative laser or TCC showed significant improvements in the investigator’s global assessment scores, and there was no statistical difference existed between the two groups [59].
Although fractional non-ablative laser is the only laser device approved by the FDA for melasma, the results vary and the high risk of PIH should be considered, especially in Asian patients. To lower the risk of the occurrence of PIH, treatment with lower fluences, variable pulses, and pretreatment with HQ for up to six weeks are recommended, particularly in patients who have a history of PIH [60].
Q-switched neodymium-doped yttrium aluminum garnet laser treatment : Exposure of skin to nanosecond-domain laser pulses affects the melanosomes through selective photothermolysis. However, laser treatment for melasma has been unsatisfactory because of the resulting inflammation and PIH. Since high-fluence laser irradiation increased the risk of adverse events, the concept of using collimated, low-fluence, 1,064-nm QSNYL treatment for melasma has been suggested. This “laser-toning” technique is popular in East Asian countries, and has become one of the first-line therapies for melasma. While its mechanism of action is unclear, several studies have found that ‘laser toning’ removes the melanosomes, but not the melanocytes. Furthermore, it damages the dendrites of the melanocytes without killing the cells, thereby functionally down-regulating the melanocytes in a process called “subcellular selective photothermolysis” [61,62]. Recently, reductions in the expression of proteins associated with melanogenesis, including TRP-1, tyrosinase-related protein-2, nerve growth factor, α-melanocyte-stimulating hormone, and tyrosinase, were also demonstrated after ‘laser toning’ [63].
In an eight-week trial, 58.8% of the patients who received ‘laser toning’ weekly, administered at 1.6-2.5 J/cm2, demonstrated an improvement of 50-75% in investigator’s global assessment scores [64]. In this study, transient pain, erythema, and edema were commonly reported, while partially hypopigmented macules and diffuse hyperpigmentation rarely occurred. Wattanakrai et al. (2010) undertook a split-face trial to compare ‘laser toning’ with 2% HQ treatment [65]. They found that the side that received ‘laser toning’ weekly, administered at 3.0-3.8 J/cm2 for five sessions, achieved marked improvements in the lightness index (L*) score (92.5%) assessed by a colorimeter, and in the modified MASI score (75.9%), compared with 19.7% and 24%, respectively, for the side administered 2% HQ. The investigators also reported that mottled hypopigmentation developed in three patients and melasma lesions recurred in all patients during follow-up.
Pulsed-dye laser treatment: Pulsed-dye laser (PDL) treatment is the gold standard therapy for vascular lesions. Evidence is accumulating that shows increased vascularization in melasma lesions, which may play a role in the recurrence of the disease [66-68]. An increase in the expression of vascular endothelial growth factor (VEGF) in keratinocytes has led to the suggestion that they may act in vessles, because functioning VEGF receptors were demonstrated in melanocytes in vitro [66,69]. Elevations in the levels of expression of c-kit, stem cell factor (SCF), and inducible nitric oxide synthase have also been observed, which could affect vascularization [70, 71].
In a split-face trial, Passeron et al. (2011) compared TCC plus PDL with TCC alone in patients with Fitzpatrick skin types II-IV [72]. At the end of treatment, the MASI scores were significantly lowered in both groups (p<0.05). However, while the improvement was sustained at the two-month follow-up assessment in the group that received combination treatment, it was not sustained in the group that received TCC alone.
Copper bromide laser treatment : Copper bromide lasers emit two wavelengths of light either separately or simultaneously: the 511-nm green beam for the treatment of pigmented lesions, and the 578-nm yellow beam for the treatment of vascular lesions. In a recent pilot study, 10 Korean patients were treated with copper bromide laser at two-week intervals for eight weeks to evaluate its efficacy and safety [73]. At the onemonth post-treatment follow-up, the mean MASI score decreased modestly from 12.3 to 9.5. L* and the erythema index (a*), measured using a Chromameter®, showed significant improvements (p<0.05). Histopathologically, reductions in the expression of melan-A, CD34, ET-1, and VEGF were observed.
Systemic tranexamic acid
Though the exact pathogenesis remains poorly understood, melasma involves alterations in different dermal components as well as increases in epidermal pigmentation. It includes disruptions and thinning of the basement membrane, prominent solar elastosis, increases in vascularization, elevations in the expression of VEGF, c-kit, and SCF, and increases in the number of mast cells [54,66,70,74]. TXA inhibits plasmin, a key molecule in angiogenesis that converts extracellular matrix-bound VEGF into its free forms [75]. TXA has also been reported to suppress neovascularization induced by basic fibroblast growth factor [76]. Therefore, TXA could reverse melasmarelated dermal changes.
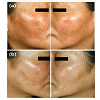
In a recent clinical trial that evaluated the efficacy of systemic TXA in the treatment of melasma, we demonstrated a decrease in the lesional melanin index and a* (erythema index) after 250 mg TXA was administered orally to 25 female study participants three-times daily for eight weeks (Figure 3) [77]. Histological analysis showed significant reductions in epidermal pigmentation, vessel numbers, and mast cell counts. In another trial conducted by Wu et al. (2012), 64.8% of the patients who were administered 250 mg TXA orally twice daily for six months showed “excellent” or “good” outcomes six months after the treatment had ceased [78]. In this study, gastrointestinal discomfort (5.4%) and hypomenorrhea (8.1%) were commonly reported, but no severe adverse events occurred.
Acquired Bilateral Nevus of Ota-Like Macules
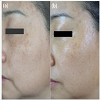
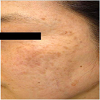
ABNOM, or Hori nevus, first described by Hori et al. (1984), is characterized by multiple bilateral speckled blue-brown or slate gray macules on the malar area or, less commonly, on the forehead, upper eyelids, and nose, with no ocular or mucosal involvement (Figure 4) [79]. It is usually found in middle-aged Asian women, with a reported incidence of 0.8% in a population-based study [80]. Histological findings include irregularly shaped, dendritic melanocytes dispersed in the papillary and mid-dermis, and particularly in the subpapillary dermis. The pathogenesis of ABNOM remains poorly understood, but it is known that ectopic dermal melanocytes resulting from incorrect migration during embryological development are activated in response to UV exposure, excessive levels of sex hormones, chronic inflammation, or other undiscovered factors [79, 81-84].Nevi of Ota and Ito
Nevi of Ota and Ito, and Mongolian spots are three variants of dermal melanocytosis, which can be distinguished by their clinical manifestations [89]. Nevus of Ota, first described by Ota in 1939, presents as a blue-black, brown, or gray patch on the face within the unilateral trigeminal nerve distribution at birth or during adolescence. Histologic findings are similar to those for ABNOM, except that the melanocytes in nevus of Ota are distributed diffusely throughout the papillary and reticular dermis [85].Mongolian Spots
Mongolian spots present as congenital blue-grayish macules, which are usually located in the sacral area of infants. Sometimes, they appear on the extremities or trunk and are called ectopic Mongolian spots. They can be seen in most Mongolian individuals during the neonatal period, then spontaneously regress. However, some Mongolian spots persist into adulthood, which is estimated to occur in 2.8-4.1% of Japanese patients aged 18-26 years [96,97]. Ectopic Mongolian spots are more likely to persist than typical Mongolian spots [98], and it is unlikely to spontaneously regress when a patient is older than 11 years [96,98]. Several studies have demonstrated good responses of persistent Mongolian spots to QS laser devices [99-102].Acknowledgements
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health & Welfare, Republic of Korea (Grant No: A100179).References
- Newcomer VD, Lindberg MC, Sternberg TH (1961) A melanosis of the face ("chloasma"). Arch Dermatol 83: 284-299.
- Pathak MA, Riley FC, Fitzpatrick TB (1962) Melanogenesis in human skin following exposure to long-wave ultraviolet and visible light. J Invest Dermatol 39: 435-443.
- Grimes PE (1995) Melasma. Etiologic and therapeutic considerations. Arch Dermatol 131: 1453-1457.
- Ortonne JP, Arellano I, Berneburg M, Cestari T, Chan H, et al. (2009) A global survey of the role of ultraviolet radiation and hormonal influences in the development of melasma. J Eur Acad Dermatol Venereol 23: 1254-1262.
- Resnik S (1967) Melasma induced by oral contraceptive drugs. JAMA 199: 601-605.
- Kang WH, Yoon KH, Lee ES, Kim J, Lee KB, et al. (2002) Melasma: histopathological characteristics in 56 Korean patients. Br J Dermatol 146: 228-237.
- Sanchez NP, Pathak MA, Sato S, Fitzpatrick TB, Sanchez JL, et al. (1981) Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study. J Am Acad Dermatol 4: 698-710.
- Ball Arefiev KL, Hantash BM (2012) Advances in the treatment of melasma: a review of the recent literature. Dermatol Surg 38: 971-984.
- Bolognia JL, Sodi SA, Osber MP, Pawelek JM (1995) Enhancement of the depigmenting effect of hydroquinone by cystamine and buthionine sulfoximine. Br J Dermatol 133: 349-357.
- Ennes SBP, Paschoalick RC, De Avelar Alchorne MM (2000) A double-blind comparative placebo-controlled study of the efficacy and tolerability of 4% hydroquinone as a depigmenting agent in melasma. J Dermatol Treat 11: 173-179.
- Briganti S, Camera E, Picardo M (2003) Chemical and instrumental approaches to treat hyperpigmentation. Pigment Cell Res 16: 101-110.
- Westerhof W, Kooyers TJ (2005) Hydroquinone and its analogues in dermatology - a potential health risk. J Cosmet Dermatol 4: 55-59.
- Nordlund JJ, Grimes PE, Ortonne JP (2006) The safety of hydroquinone. J Eur Acad Dermatol Venereol 20: 781-787.
- Gupta AK, Gover MD, Nouri K, Taylor S (2006) The treatment of melasma: a review of clinical trials. J Am Acad Dermatol 55: 1048-1065.
- Rendon M, Berneburg M, Arellano I, Picardo M (2006) Treatment of melasma. J Am Acad Dermatol 54: S272-281.
- Kang HY, Valerio L, Bahadoran P, Ortonne JP (2009) The role of topical retinoids in the treatment of pigmentary disorders: an evidence-based review. Am J Clin Dermatol 10: 251-260.
- Lee IW, Lee SC, Kim DS, Kim HJ, Park KC (2001) Effects of dexamethasone on endothelin-1 (ET-1) production by keratinocytes. Ann Dermatol 13: 148-152.
- Kim DS, Kim HJ, Choi KH, Chung JH, Kim KH, et al. (2001) UVB-induced GM-CSF production is suppressed by dexamethasone in HaCaT cells. Photodermatol Photoimmunol Photomed 17: 121-125.
- Ferreira Cestari T, Hassun K, Sittart A, de Lourdes Viegas M (2007) A comparison of triple combination cream and hydroquinone 4% cream for the treatment of moderate to severe facial melasma. J Cosmet Dermatol 6: 36-39.
- Chan R, Park KC, Lee MH, Lee ES, Chang SE, et al. (2008) A randomized controlled trial of the efficacy and safety of a fixed triple combination (fluocinolone acetonide 0.01%, hydroquinone 4%, tretinoin 0.05%) compared with hydroquinone 4% cream in Asian patients with moderate to severe melasma. Br J Dermatol 159: 697-703.
- Grimes PE, Bhawan J, Guevara IL, Colon LE, Johnson LA, et al. (2010) Continuous therapy followed by a maintenance therapy regimen with a triple combination cream for melasma. J Am Acad Dermatol 62: 962-967.
- Sugai T (1992) Clinical effects of arbutin in patients with chloasma. Skin Res 34: 522-529.
- Chakraborty AK, Funasaka Y, Komoto M, Ichihashi M (1998) Effect of arbutin on melanogenic proteins in human melanocytes. Pigment Cell Res 11: 206-212.
- Ertam I, Mutlu B, Unal I, Alper S, Kivcak B, et al. (2008) Efficiency of ellagic acid and arbutin in melasma: a randomized, prospective, open-label study. J Dermatol 35: 570-574.
- Battaini G, Monzani E, Casella L, Santagostini L, Pagliarin R (2000) Inhibition of the catecholase activity of biomimetic dinuclear copper complexes by kojic acid. J Biol Inorg Chem 5: 262-268.
- Moon KY, Ahn KS, Lee J, Kim YS (2001) Kojic acid, a potential inhibitor of NF-kappaB activation in transfectant human HaCaT and SCC-13 cells. Arch Pharm Res 24: 307-311.
- Nazzaro-Porro M, Passi S (1978) Identification of tyrosinase inhibitors in cultures of Pityrosporum. J Invest Dermatol 71: 205-208.
- Balina LM, Graupe K (1991) The treatment of melasma. 20% azelaic acid versus 4% hydroquinone cream. Int J Dermatol 30: 893-895.
- Kim DS, Kim SY, Park SH, Choi YG, Kwon SB, et al. (2005) Inhibitory effects of 4-n-butylresorcinol on tyrosinase activity and melanin synthesis. Biol Pharm Bull 28: 2216-2219.
- Huh SY, Shin JW, Na JI, Huh CH, Youn SW, et al. (2010) Efficacy and safety of liposome-encapsulated 4-n-butylresorcinol 0.1% cream for the treatment of melasma: a randomized controlled split-face trial. J Dermatol 37: 311-315.
- Park KC, Huh SY, Choi HR, Kim DS (2010) Biology of melanogenesis and the search for hypopigmenting agents. Dermatologica Sinica 28: 53-58.
- Ros JR, Rodriguez-Lopez JN, Garcia-Canovas F (1993) Effect of L-ascorbic acid on the monophenolase activity of tyrosinase. Biochem J 295 ( Pt 1): 309-312.
- Gukasyan GS (2002) Study of the kinetics of oxidation of monophenols by tyrosinase. The effect of reducers. Biochemistry (Mosc) 67: 277-280.
- Huh CH, Seo KI, Park JY, Lim JG, Eun HC, et al. (2003) A randomized, double-blind, placebo-controlled trial of vitamin C iontophoresis in melasma. Dermatology 206: 316-320.
- Ichihashi M, Funasaka Y, Ohashi A, Chacraborty A, Ahmed NU, et al. (1999) The inhibitory effect of DL-alpha-tocopheryl ferulate in lecithin on melanogenesis. Anticancer Res 19: 3769-3774.
- Yamamura T, Onishi J, Nishiyama T (2002) Antimelanogenic activity of hydrocoumarins in cultured normal human melanocytes by stimulating intracellular glutathione synthesis. Arch Dermatol Res 294: 349-354.
- Saliou C, Kitazawa M, McLaughlin L, Yang JP, Lodge JK, et al. (1999) Antioxidants modulate acute solar ultraviolet radiation-induced NF-kappa-B activation in a human keratinocyte cell line. Free Radic Biol Med 26: 174-183.
- Kasraee B (2002) Depigmentation of brown Guinea pig skin by topical application of methimazole. J Invest Dermatol 118: 205-207.
- Kasraee B (2002) Peroxidase-mediated mechanisms are involved in the melanocytotoxic and melanogenesis-inhibiting effects of chemical agents. Dermatology 205: 329-339.
- Robb EL, Page MM, Wiens BE, Stuart JA (2008) Molecular mechanisms of oxidative stress resistance induced by resveratrol: Specific and progressive induction of MnSOD. Biochem Biophys Res Commun 367: 406-412.
- Seiberg M, Paine C, Sharlow E, Andrade-Gordon P, Costanzo M, et al. (2000) Inhibition of melanosome transfer results in skin lightening. J Invest Dermatol 115: 162-167.
- Seiberg M, Paine C, Sharlow E, Andrade-Gordon P, Costanzo M, et al. (2000) The protease-activated receptor 2 regulates pigmentation via keratinocyte-melanocyte interactions. Exp Cell Res 254: 25-32.
- Minwalla L, Zhao Y, Cornelius J, Babcock GF, Wickett RR, et al. (2001) Inhibition of melanosome transfer from melanocytes to keratinocytes by lectins and neoglycoproteins in an in vitro model system. Pigment Cell Res 14: 185-194.
- Hakozaki T, Minwalla L, Zhuang J, Chhoa M, Matsubara A, et al. (2002) The effect of niacinamide on reducing cutaneous pigmentation and suppression of melanosome transfer. Br J Dermatol 147: 20-31.
- Ando H, Funasaka Y, Oka M, Ohashi A, Furumura M, et al. (1999) Possible involvement of proteolytic degradation of tyrosinase in the regulatory effect of fatty acids on melanogenesis. J Lipid Res 40: 1312-1316.
- Ando H, Ryu A, Hashimoto A, Oka M, Ichihashi M (1998) Linoleic acid and alpha-linolenic acid lightens ultraviolet-induced hyperpigmentation of the skin. Arch Dermatol Res 290: 375-381.
- Ando H, Wen ZM, Kim HY, Valencia JC, Costin GE, et al. (2006) Intracellular composition of fatty acid affects the processing and function of tyrosinase through the ubiquitin-proteasome pathway. Biochem J 394: 43-50.
- Ando H, Watabe H, Valencia JC, Yasumoto K, Furumura M, et al. (2004) Fatty acids regulate pigmentation via proteasomal degradation of tyrosinase: a new aspect of ubiquitin-proteasome function. J Biol Chem 279: 15427-15433.
- Mishima Y, Imokawa G (1983) Selective aberration and pigment loss in melanosomes of malignant melanoma cells in vitro by glycosylation inhibitors: premelanosomes as glycoprotein. J Invest Dermatol 81: 106-114.
- Franchi J, Coutadeur MC, Marteau C, Mersel M, Kupferberg A (2000) Depigmenting effects of calcium D-pantetheine-S-sulfonate on human melanocytes. Pigment Cell Res 13: 165-171.
- Moreno Arias GA, Ferrando J (2001) Intense pulsed light for melanocytic lesions. Dermatol Surg 27: 397-400.
- Li YH, Chen JZ, Wei HC, Wu Y, Liu M, et al. (2008) Efficacy and safety of intense pulsed light in treatment of melasma in Chinese patients. Dermatol Surg 34: 693-700.
- Chan NP, Ho SG, Shek SY, Yeung CK, Chan HH (2010) A case series of facial depigmentation associated with low fluence Q-switched 1,064 nm Nd:YAG laser for skin rejuvenation and melasma. Lasers Surg Med 42: 712-719.
- Torres-Alvarez B, Mesa-Garza IG, Castanedo-Cazares JP, Fuentes-Ahumada C, Oros-Ovalle C, et al. (2011) Histochemical and immunohistochemical study in melasma: evidence of damage in the basal membrane. Am J Dermatopathol 33: 291-295.
- Negishi K, Kushikata N, Tezuka Y, Takeuchi K, Miyamoto E, et al. (2004) Study of the incidence and nature of "very subtle epidermal melasma" in relation to intense pulsed light treatment. Dermatol Surg 30: 881-886.
- Sheth VM, Pandya AG (2011) Melasma: a comprehensive update: part II. J Am Acad Dermatol 65: 699-714.
- Rokhsar CK, Fitzpatrick RE (2005) The treatment of melasma with fractional photothermolysis: a pilot study. Dermatol Surg 31: 1645-1650.
- Wind BS, Kroon MW, Meesters AA, Beek JF, van der Veen JP, et al. (2010) Non-ablative 1,550 nm fractional laser therapy versus triple topical therapy for the treatment of melasma: a randomized controlled split-face study. Lasers Surg Med 42: 607-612.
- Kroon MW, Wind BS, Beek JF, van der Veen JP, Nieuweboer-Krobotova L, et al. (2011) Nonablative 1550-nm fractional laser therapy versus triple topical therapy for the treatment of melasma: a randomized controlled pilot study. J Am Acad Dermatol 64: 516-523.
- Rahman Z, Alam M, Dover JS (2006) Fractional Laser treatment for pigmentation and texture improvement. Skin Therapy Lett 11: 7-11.
- Mun JY, Jeong SY, Kim JH, Han SS, Kim IH (2011) A low fluence Q-switched Nd:YAG laser modifies the 3D structure of melanocyte and ultrastructure of melanosome by subcellular-selective photothermolysis. J Electron Microsc (Tokyo) 60: 11-18.
- Kim JH, Kim H, Park HC, Kim IH (2010) Subcellular selective photothermolysis of melanosomes in adult zebrafish skin following 1064-nm Q-switched Nd:YAG laser irradiation. J Invest Dermatol 130: 2333-2335.
- Kim JE, Chang SE, Yeo UC, Haw S, Kim IH (2013) Histopathological study of the treatment of melasma lesions using a low-fluence Q-switched 1064-nm neodymium:yttrium-aluminium-garnet laser. Clin Exp Dermatol 38: 167-71.
- Jeong SY, Chang SE, Bak H (2008) New melasma treatment by collimated low fluence Q-switched Nd:YAG laser. Korean J Dermatol 46: 1163-1170.
- Wattanakrai P, Mornchan R, Eimpunth S (2010) Low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser for the treatment of facial melasma in Asians. Dermatol Surg 36: 76-87.
- Kim EH, Kim YC, Lee ES, Kang HY (2007) The vascular characteristics of melasma. J Dermatol Sci 46: 111-116.
- Kang HY, Bahadoran P, Suzuki I, Zugaj D, Khemis A, et al. (2010) In vivo reflectance confocal microscopy detects pigmentary changes in melasma at a cellular level resolution. Exp Dermatol 19: e228-233.
- Passeron T (2013) Long-lasting effect of vascular targeted therapy of melasma. J Am Acad Dermatol 69: e141-142.
- Kim EJ, Park HY, Yaar M, Gilchrest BA (2005) Modulation of vascular endothelial growth factor receptors in melanocytes. Exp Dermatol 14: 625-633.
- Kang HY, Hwang JS, Lee JY, Ahn JH, Kim JY, et al. (2006) The dermal stem cell factor and c-kit are overexpressed in melasma. Br J Dermatol 154: 1094-1099.
- Jo HY, Kim CK, Suh IB, Ryu SW, Ha KS, et al. (2009) Co-localization of inducible nitric oxide synthase and phosphorylated Akt in the lesional skins of patients with melasma. J Dermatol 36: 10-16.
- Passeron T, Fontas E, Kang HY, Bahadoran P, Lacour JP, et al. (2011) Melasma treatment with pulsed-dye laser and triple combination cream: a prospective, randomized, single-blind, split-face study. Arch Dermatol 147: 1106-1108.
- Lee HI, Lim YY, Kim BJ, Kim MN, Min HJ, et al. (2010) Clinicopathologic efficacy of copper bromide plus/yellow laser (578 nm with 511 nm) for treatment of melasma in Asian patients. Dermatol Surg 36: 885-893.
- Hernandez-Barrera R, Torres-Alvarez B, Castanedo-Cazares JP, Oros-Ovalle C, Moncada B (2008) Solar elastosis and presence of mast cells as key features in the pathogenesis of melasma. Clin Exp Dermatol 33: 305-308.
- Ferrara N (2010) Binding to the extracellular matrix and proteolytic processing: two key mechanisms regulating vascular endothelial growth factor action. Mol Biol Cell 21: 687-690.
- Bastaki M, Nelli EE, Dell'Era P, Rusnati M, Molinari-Tosatti MP, et al. (1997) Basic fibroblast growth factor-induced angiogenic phenotype in mouse endothelium. A study of aortic and microvascular endothelial cell lines. Arterioscler Thromb Vasc Biol 17: 454-464.
- Na JI, Choi SY, Yang SH, Choi HR, Kang HY, et al. (2013) Effect of tranexamic acid on melasma: a clinical trial with histological evaluation. J Eur Acad Dermatol Venereol 27: 1035-1039.
- Wu S, Shi H, Wu H, Yan S, Guo J, et al. (2012) Treatment of melasma with oral administration of tranexamic acid. Aesthetic Plast Surg 36: 964-970.
- Hori Y, Kawashima M, Oohara K, Kukita A (1984) Acquired, bilateral nevus of Ota-like macules. J Am Acad Dermatol 10: 961-964.
- Sun CC, Lu YC, Lee EF, Nakagawa H (1987) Naevus fusco-caeruleus zygomaticus. Br J Dermatol 117: 545-553.
- Mizushima J, Nogita T, Higaki Y, Horikoshi T, Kawashima M (1998) Dormant melanocytes in the dermis: do dermal melanocytes of acquired dermal melanocytosis exist from birth? Br J Dermatol 139: 349-350.
- Rubin AI, Laborde SV, Stiller MJ (2001) Acquired dermal melanocytosis: appearance during pregnancy. J Am Acad Dermatol 45: 609-613.
- Murakami F, Baba T, Mizoguchi M (2000) Ultraviolet-induced generalized acquired dermal melanocytosis with numerous melanophages. Br J Dermatol 142: 184-186.
- Murakami F, Soma Y, Mizoguchi M (2005) Acquired symmetrical dermal melanocytosis (naevus of Hori) developing after aggravated atopic dermatitis. Br J Dermatol 152: 903-908.
- Park JM, Tsao H, Tsao S (2009) Acquired bilateral nevus of Ota-like macules (Hori nevus): etiologic and therapeutic considerations. J Am Acad Dermatol 61: 88-93.
- Kunachak S, Leelaudomlipi P (2000) Q-switched Nd:YAG laser treatment for acquired bilateral nevus of ota-like maculae: a long-term follow-up. Lasers Surg Med 26: 376-379.
- Polnikorn N, Tanrattanakorn S, Goldberg DJ (2000) Treatment of Hori's nevus with the Q-switched Nd:YAG laser. Dermatol Surg 26: 477-480.
- Suh DH, Han KH, Chung JH (2001) Clinical use of the Q-switched Nd:YAG laser for the treatment of acquired bilateral nevus of Ota-like macules (ABNOMs) in Koreans. J Dermatolog Treat 12: 163-166.
- Stanford DG, Georgouras KE (1996) Dermal melanocytosis: a clinical spectrum. Australas J Dermatol 37: 19-25.
- Mishima Y, Mevorah B (1961) Nevus Ota and nevus Ito in American Negroes. J Invest Dermatol 36: 133-154.
- Mataix J, Lopez N, Haro R, Gonzalez E, Angulo J, et al. (2007) Late-onset Ito's nevus: an uncommon acquired dermal melanocytosis. J Cutan Pathol 34: 640-643.
- Geronemus RG (1992) Q-switched ruby laser therapy of nevus of Ota. Arch Dermatol 128: 1618-1622.
- Moreno-Arias GA, Camps-Fresneda A (2001) Treatment of nevus of Ota with the Q-switched alexandrite laser. Lasers Surg Med 28: 451-455.
- Chan HH, Ying SY, Ho WS, Kono T, King WW (2000) An in vivo trial comparing the clinical efficacy and complications of Q-switched 755 nm alexandrite and Q-switched 1064 nm Nd:YAG lasers in the treatment of nevus of Ota. Dermatol Surg 26: 919-922.
- Choi CW, Kim HJ, Lee HJ, Kim YH, Kim WS (2013) Treatment of nevus of Ota using low fluence Q-switched Nd:YAG laser. Int J Dermatol.
- Hidano A (1971) Persistent Mongolian spot in the adult. Arch Dermatol 103: 680-681.
- Kikuchi I, Inoue S (1980) Natural history of the Mongolian spot. J Dermatol 7: 449-450.
- Kikuchi I (1980) Mongolian spots remaining in schoolchildren a statistical survey in Central Okinawa. J Dermatol 7: 213-216.
- Kagami S, Asahina A, Watanabe R, Mimura Y, Shirai A, et al. (2007) Treatment of 153 Japanese patients with Q-switched alexandrite laser. Lasers Med Sci 22: 159-163.
- Kagami S, Asahina A, Watanabe R, Mimura Y, Shirai A, et al. (2008) Laser treatment of 26 Japanese patients with Mongolian spots. Dermatol Surg 34: 1689-1694.
- Shirakawa M, Ozawa T, Ohasi N, Ishii M, Harada T (2010) Comparison of regional efficacy and complications in the treatment of aberrant Mongolian spots with the Q-switched ruby laser. J Cosmet Laser Ther 12: 138-142.
- Kagami S, Asahina A, Uwajima Y, Miyamoto A, Yamada D, et al. (2012) Treatment of persistent Mongolian spots with Q-switched alexandrite laser. Lasers Med Sci 27: 1229-1232.