Journal of Integrative Medicine & Therapy
Download PDF
Research Article
*Address for Correspondence: Guan-Cheng Sun, Institute of Qigong and Integrative Medicine, 10127 Main Place Suite B, Bothell, WA 98011, Tel: (206) 290-6072; E-mail: gsun@bastyr.edu
Citation: Sun GC, Ding X, Zhou XH, Putiri A, Bradley R. Effects of Yi Ren Medical Qigong on Body Weight in People with Type 2 Diabetes Mellitus: A Secondary Analysis of a Randomized Controlled Pilot Study. J Integrative Med Ther. 2014;1(1): 5.
Copyright © 2014 Sun GC, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Integrative Medicine & Therapy| ISSN 2378-1343 | Volume: 1, Issue: 1
Submission: 02 January 2014 | Accepted: 19 February 2014 | Published: 24 February 2014
Reviewed & Approved by: Dr. Adam Perlman, Executive Director, Duke Integrative Medicine, Durham
Effects of YRMQ on estimates of HOMA-IR
Effects of Yi Ren Medical Qigong on Body Weight in People with Type 2 Diabetes Mellitus: A Secondary Analysis of a Randomized Controlled Pilot Study
Guan-Cheng Sun1,2*, Xiaobo Ding3, Xiao-Hua Zhou3, Amy Putiri1 and Ryan Bradley4
- 1Institute of Qigong and Integrative Medicine, Bothell, Washington
- 2Bastyr University Research Institute, Kenmore, Washington
- 3University of Washington, Department of Biostatistics, School of Public Health and Community Medicine, and HSR&D VA Pudget Sound Health Care SystemSeattle, Washington
- 4Bastyr University Research Institute, San Diego, California
*Address for Correspondence: Guan-Cheng Sun, Institute of Qigong and Integrative Medicine, 10127 Main Place Suite B, Bothell, WA 98011, Tel: (206) 290-6072; E-mail: gsun@bastyr.edu
Citation: Sun GC, Ding X, Zhou XH, Putiri A, Bradley R. Effects of Yi Ren Medical Qigong on Body Weight in People with Type 2 Diabetes Mellitus: A Secondary Analysis of a Randomized Controlled Pilot Study. J Integrative Med Ther. 2014;1(1): 5.
Copyright © 2014 Sun GC, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Integrative Medicine & Therapy| ISSN 2378-1343 | Volume: 1, Issue: 1
Submission: 02 January 2014 | Accepted: 19 February 2014 | Published: 24 February 2014
Reviewed & Approved by: Dr. Adam Perlman, Executive Director, Duke Integrative Medicine, Durham
Abstract
Objectives: The objective of this study was to determine whether Yi Ren Medical Qigong (YRMQ) has a positive impact on body weight in people with type 2 diabetes mellitus (T2DM).Design: A secondary analysis was conducted with data collected during a completed randomized, controlled clinical trial study.Settings/location: Bastyr University Research Institute (Kenmore, WA)
Subjects: Participants (n=32), mean age of 56.3 ± 8.1(SD) years, with diagnosed type 2 diabetes and HbA1C > 7.5%, fasting blood glucose > 7 mmol/l (126 mg/dl).
Interventions: Patients were randomized into a standard care plus YRMQ group, or standard care plus progressive resistance training (PRT group), or standard care alone (control group).
Outcome measures: Outcome measures included body weight, body mass index (BMI), fasting glucose, and homeostasis assessment index estimates of insulin resistance (HOMA-IR).
Results: Both the YRMQ and PRT groups had a significant trend of decrease in body weight and BMI when compared to the control group. For the body weight, the p-values of the rank sum tests for control-PRT, control-YRMQ and PRT-YRMQ are 0.02, 0.10 and 0.55, respectively. For BMI, the p-values of the rank sum tests for control-PRT, control-YRMQ and PRT-YRMQ are 0.01, 0.04 and 0.73, respectively. The Qigong group also showed trends for improvement in insulin resistance while PRT did not, despite the significant body weight loss in the PRT group.
Conclusion: Yi Ren Medical Qigong was associated with trends in weight loss and improvement of insulin resistance in people with type 2 diabetes mellitus.
Introduction
Type 2 diabetes mellitus (T2DM) is the most common form of diabetes, affecting over 90% of the people with diabetes. T2DM is marked by abnormally high levels of blood glucose, as a result of the bodies’ inability to use blood glucose because of relative insulin deficiency or sustained insulin resistance. There is no cure for T2DM in today’s medical science, and the typical clinical course is for patients to respond to pharmacotherapy initially by normalizing their fasting glucose levels, and then to undergo gradual deterioration in glycemic control despite optimal medical management using a variety of drugs [1].In the view of Traditional Chinese Medicine (TCM), T2DM is named as “Xiao Ke Zheng”, which refers to excessive drinking and urination” [2]. Its pathogenesis is considered to be the accumulation of “Heat” (Yang) and the consumption of “Yin,” where the Lung, Spleen and Kidney are all directly affected. Treatment focuses on giving comprehensive, individual, and integrated recommendations for the whole body [3]. TCM therapy is usually used as adjuvants in combination with anti-diabetic drugs. However, there is still insufficient evidence to draw definitive conclusions about the efficacy of TCM for diabetes [4].
Qigong (pronounced “chee gung”) is an important part of TCM, and has been reported to prevent and cure disease, and to improve chronic health conditions by self-practice or by receiving qi from a Qigong therapist [5]. In Qigong the term “qi” (or “chi”) means “vital energy of the body” and “gong” means the skill and achievement cultivated through regular and disciplined practice. Although in TCM qigong is considered “energetic medicine”, the practice of qigong combines breathing, movement and meditation, and therefore is often classified by Western providers under the category of “mind/body medicine”. Qigong refers to the mind-body operational skills and techniques that integrate the adjustments (regulations) of mind, body and breathing into Oneness” [6]. Regardless of its classification, previous studies suggest that Qigong may be a beneficial adjunct treatment for individuals with T2DM [2,7-10].There were consistent and statistically significant positive associations between participation in Qigong and blood glucose, triglycerides and total cholesterol [11]. Recently, systematic reviews have found support for a role of Qigong in the management of T2MD [2,10]. However, important to this evaluation, no studies performed thus far have reported evidence of any beneficial effect of Qigong on weight [11]. In order to evaluate whether Qigong has beneficial effects on people with T2DM, we conducted a three-armed, 12-week randomized, controlled clinical trial to compare the biological and psychological responses of Qigong with progressive resistance training (PRT) or standard care in patients with T2DM. Our primary results on blood glucose control [5] and perceived stress [4] have been previously reported. In this study, our specific objective was to perform a secondary analysis of our completed RCT in order to understand potentially beneficial mechanisms of Qigong on body weight and insulin resistance in people with T2DM.
Research Design and Methods
Design and subjectsThis study used a three-armed, randomized, controlled clinical trial design. All research protocols were approved by the Institutional Review Board (IRB) at Bastyr University and subjects provided Informed Consent. To be eligible, participants had to be between 18 and 65 years of age and diagnosed with type 2 diabetes from their primary care physician, and the participants met the inclusion criteria consisting of an HbA1c level greater than 7.5% and a fasting blood glucose greater than 7 mmol/dL (126 mg/dL). The research team randomly assigned age- and sex-matched participants (N = 32, 13 men and 19 women) to one of three groups for a 12-weekintervention period. None of the participants were taking insulin; however, all were taking oral diabetes medication [5,12].
Intervention
All participants were asked to maintain their current activity levels including medications, diet and exercise during the study. Group 1 (n=11) received the Yi Ren Medical Qigong (YRMQ) intervention; group 2 (n=11) received the progressive resistance training (PRT) intervention, as an active comparator; and group 3 (n=10) served as the standard care control group. All interventions lasted 12 weeks and included weekly supervised YRMQ and PRT sessions as well as at-home practice. The intervention consisted of weekly YRMQ or PRT sessions in groups (60 min/wk) that certified instructors led. In addition, the research team asked participants in both active treatment groups to practice at home twice a week for 30 minutes per session [5,12].
Measures
Blood glucose and body weight were obtained at baseline, week 4, week 8 and at the end of week 12. HbA1c, insulin, Perceived Stress Scale (PSS) and Beck Depression Inventory (BDI) were measured before and after the intervention as described in our previous report [12]. Blood testing required a 12-hour fast (no food or drink, except water and medications); approximately 20ml of blood was obtained via a venipuncture in the arm with the individual in an upright position and after at least 5 minutes in a resting state. We measured height and weight after an overnight fast with the participant dressed in light clothing and without shoes. Homeostasis assessment index estimates of insulin resistance (HOMA-IR) was calculated using fasting glucose and fasting insulin according to published methods [13].
Statistical analysis
Data were analyzed using MATLAB (version 7.3, MathWorks, Inc., Natick, MA, USA). Demographic characteristics for each treatment group were described as medians, means and standard deviations for continuous variables, and frequency counts and percentages for categorical variables. To compare the effect of YRMQ and PRT on the major outcome variables to the control group, it is required that any outcome variable has the same distribution among the three groups at the baseline. Thenon-parametric one-way analysis of variance, the Kruskal-Wallis test, was used to check whether an outcome variable had the same distribution among the three groups at baseline. The same approach was used to the test for differences in the outcome variables before and after treatment to find out whether each treatment had the same effect for the outcome variable. The Wilcoxon rank-sum test was employed to determine any differences between any two of YRMQ, PRT and standard care. Considering the feasibility of recruiting and retaining study participants, the sample size for this pilot study is small. If a test is not significant, it may be due to the insufficient statistical power by the small sample size. However, if a test is significant, it has the same interpretation regardless of the sample size. We considered p-values < 0.05 as statistically significant. The original randomization allocation from our primary analyses was maintained in all secondary analyses reported here.
Results
Attrition and complianceTable 1 summarizes demographic characteristics of study participants. Thirteen men and 19 women had a mean age of 56.3 ± 8.1 yr and mean Body Mass Index (BMI) of 31.8 ± 6.0 kg/m2 with Caucasian 59% and non-Caucasian 41%.The mean HbA1c was 8.2 ± 1.1, 8.2 ± 1.2 and 8.1 ± 1.1 in YRMQ, PRT and standard care control groups, respectively. A total of 9 participants dropped out from the study including 2 from standard care control group, 5 from PRT group, and 2 from YRMQ group, corresponding to dropout frequencies of 20%, 45%, and 18%, respectively. Our pilot data demonstrate that it is feasible to implement YRMQ as an adjunct complementary therapy to conventional standard care for treating T2DM. In this study, the completion rate was relatively high at Qigong group (82%) compared with PRT group (55%) and standard care control group (80%). There was no any adverse event related to the intervention.
The body weights at baseline (mean ± SD) were 180.1 ± 44.3, 201.8 ± 30.5 and 194.5 ± 34.9 in YRMQ, PRT and standard care control groups, respectively (p=0.71). The changes of body weight during the intervention in the three groups are plotted in Figure 1A. The body weights in the control group increased in all except two patients; while in the PRT group the body weights of 4 patients decreased, 1 patient remained unchanged and 1 patient experienced weight increase. We observed an interesting phenomenon in the YRMQ group: there was a tendency for patients with high baseline body weights to experience weight reductions and patients with lower baseline body weights to experience weight increases. This indicates that YRMQ may lead to reduction of body weights in more obese individuals. Figure 1B shows that a strong trend towards significant increase over time for the body weight in the control group, but slightly decrease in the YRMQ and PRT groups. The Kruskal-Wallis test comparing the median of changes in the three groups suggests that the three groups are significantly different (p=0.055). Note that the p-value for testing the zero median of the changes in body weights in the untreated conventional standard care group is 0.055, showing that a strong trend towards increased body weight over time during the 12 weeks intervention period. On the other hand, the p-values of the rank sum tests for control-PRT, control-YRMQ and PRT-YRMQ are 0.02, 0.10 and 0.55, respectively. This indicates that YRMQ and PRT have beneficial effect in body weight loss compared to the standard care, although there is no difference in change in weight between YRMQ and PRT.
Changes in BMI
Baseline BMI values are reported in Table 1. The BMI at baseline (mean ± SD) was 32.4 ± 8.3, 32.7 ± 4.7 and 30.1 ± 4.1 in YRMQ, PRT, and standard care control groups, respectively (p=0.71). The changes of BMI during the intervention in the three groups are plotted in Figure 2A. BMI values in the control group increased in all except one patient; while the BMI values in the PRT group decreased in all except one patient. We observed an interesting phenomenon in the YRMQ group: there was a tendency for patients with high baseline BMI values to experience BMI reductions and patients with lower baseline BMI values to experience BMI increases. This indicates that YRMQ may lead to reduction of BMI in more obese individuals. Figure 2B shows that a strong trend towards significant increase over time for the body weight in the control group, but slightly decrease in the YRMQ and PRT groups. The Kruskal-Wallis test comparing the median of changes in the three groups suggests that the three groups are significantly different (p=0.021). Note that the p-value for testing the zero-median of the changes in BMI values in the untreated conventional standard care group is 0.070, showing that a strong trend towards significant increase over time for BMI during the 12 weeks intervention period. On the other hand, the p-values of the rank sum tests for control-PRT, control-YRMQ and PRT-YRMQ are 0.01, 0.04 and 0.73, respectively. This indicates that YRMQ and PRT have beneficial effect in BMI compared to the standard care, although there is no difference in change in weight between YRMQ and PRT.
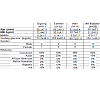
Effects of YRMQ on estimates of HOMA-IR
Adequate baseline and follow-up data was available to calculate HOMA-IR for 8, 6 and 9 subjects in the untreated standard care control group, PRT and YRMQ groups respectively. The HOMAIR values at baseline and week-12 of every patient are plotted in Figure 3A. The means and standard deviations of differences of the HOMA-IR values before and after treatment are shown in Figure 3B. For baseline HOMA-IR, the p-value of the Kruskal-Wallis test is 0.86, revealing that the distributions of HOMA-IR values in the three groups have identical median. The rank sum tests comparing control-PRT, control-YRMQ and PRT-YRMQ were shown as P=0.76, 0.08 and 0.09, respectively. These results suggested that YRMQ group showed a strong trend towards significant differences over time for HOMA-IR values comparing with standard care and PRT.
Discussion
The results on the beneficial effects of YRMQ in diabetes are consistent with the studies of Miller et al. [9] and Liu et al. [8] of Qigong in patients with impaired glucose tolerance not on diabetes medication. In our study, we recruited a different population: all participants were diagnosed with diabetes and many participants were on oral diabetes medication but not on insulin treatment. Interestingly, we found that both YRMQ and PRT demonstrated its beneficial effects on weight loss as shown in Figure 1A and 1B, Figures 2A and 2B, but HOMA-IR index score increased 28% in PRT group and decreased 1.3% in YRMQ group in this population as shown in Figure 3A and 3B. We also report a potentially interested observation in the YRMQ group: where those participants with high BMI values at baseline had BMI reductions experienced decreased insulin resistance and participants with low BMI values experienced BMI increase with decreased insulin resistance as well. The PRT group demonstrated significant body weight loss and BMI decrease as shown in Figure 1B and Figure 2B, but their insulin resistance increased as shown in Figure 3B, leading us to hypothesize that the YRMQ group’s results indicate a different mechanism at work than we observed in the PRT group.This low-cost intervention of Yi Ren Medical Qiong as an adjunct part of a program of treatment may play an important role in T2DM management.Traditional Chinese medicine (TCM) categorizes T2DM as “Xiao Ke Zheng”. According to the TCM, the pathogenesis of T2DM is considered to be the accumulation of “Heat” (Yang) and the consumption of “Yin,” where the Lung, Spleen and Kidney are all directly affected. Basis of our clinical observation on study participants, we agree that the pathogenesis of T2DM is associated und the direct connections with lungs and spleen. From our clinical observation with internal qi diagnostics, we found that the causes of T2DM are associated with imbalanced autonomic nervous system, weakened pancreas, lower energy of kidneys and excess energy of the hyper liver, particularly the disharmony relationship between the liver and pancreas. According to the five-element theory, we observed the phenomenon of the Liver-Wood overpowers the Pancreas-Earth and weakens the Kidneys-Water. This internal qi/subtle energy based diagnosis and observation may provide new perspective for TCM therapies for treating T2DM.
The present research is limited in several ways. First, although this analysis was performed using data collected from a well-controlled clinical trial, changes in body weight/BMI were not our pre-specified outcome from this trial, therefore our observations deserve replication in another trial designed to detect clinically significant changes in weight. Our study is limited due to our small sample size and relatively high loss to follow-up. As mentioned, we were not originally powered to detect changes in body weight, which may explain the marginal p-values associated with mean weight changes; similarly this likely explains why, despite a trend in improved HOMA-IR, this change did not reach statistical significance. Our study is also limited in intent to treat analysis, due to exclusion of participants. The research team excluded three from analysis (one from the PRT group and two from the YRMQ group) as a result of changes in their medications [12]. Finally, our results are also limited in that HOMA-IR is a validated estimate of insulin resistance, but it is not a gold-standard measure. Despite these limitations the results presented are consistent with previously reported results on glucose improvements, and provide excellent preliminary data from which to design a larger randomized trial applying gold-standard assessments of body weight, and powered for clinically significant changes in body weight.
This study investigated the short-term benefits of the YRMQ intervention with a small size of participants. It would be worthwhile in future studies with larger subject numbers to investigate whether the benefit is sustained in the long term with participants who continue to practice YRMQ at home. Despite these limitations, the findings of this study provide evidence that YRMQ is feasible and effective in assisting in the management of T2DM with or without reducing body weight. Further studies examining long-term benefits of YRMQ, including a potential association between improvement in weight loss and insulin resistance, may provide additional information that may assist patients with T2DM and clinicians in providing optimal comprehensive diabetes care.
Conclusion
The findings of the recent analysis of the YRMQ intervention were associated with trends in weight loss (p=0.1), and BMI reduction (p=0.04) and improvement of insulin resistance (p=0.075) in people with T2DM. The effect of YRMQ on insulin resistance may work different mechanisms from PRT.Acknowledgement
This study is funded in part by the T32 training grant (T32 AT000815-06) from the National Center for Complementary and Alternative Medicine with the National Institutes of Health, the Seattle Foundation, VA Seattle Washington and the Institute of Qigong & Internal Alternative Medicine. We greatly appreciate HSR&D Center of Excellence, VA Puget Sound Health Care System, and the Department of Biostatistics, University of Washington for their support. Dr. Zhou’s work was supported in part by U.S. Department of Veterans Affairs, Veterans Affairs Health Administration, HSR&D grants (RCS 05-196). Dr. Bradley’s time was supported during the conduct of the original trial by grant number 1KL2RR025015-01 from the National Center for Research Resources (NCRR). Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the author(s) and not of the funding sources. We are especially grateful for the kind and valuable cooperation of the volunteers who made this study possible. We thank the Bastyr University Research Institute staff for their help. Our thanks to Jennifer Lovejoy, PhD, for her review, advice and editing in the preparation of this manuscript.References
- Robertson RP, Harmon J, Tran PO, Poitout V (2004) Beta-cell glucose toxicity, lipotoxicity, and chronic oxidative stress in type 2 diabetes. Diabetes 53: S119-S124.
- Chen KW, Liu T, Zhang H, Lin Z (2009) An analytical review of the Chinese literature on Qigong therapy for diabetes mellitus. Am J Chin Med 37: 439-457.
- Liu X, Feng C (2005) Recent advances in TCM treatment of diabetic gangrene. J Tradit Chin Med 25: 70-77.
- Xie W, Zhao Y, Zhang Y (2011)Traditional ChineseMedicines in Treatment of Patients with Type 2 diabetes mellitus. Evid Based Complement Alternat Med 2011: 726723.
- Sun GC (2010) Effects of Qigong on glucose control in type 2 diabetes: a randomized controlled pilot study. Diabetes care 33: e8.
- Liu T, Chen KW (2010) Chinese Medical Qigong. Singing Dragon.
- Tsujiuchi T, Kumano H, Yoshiuchi K, He D, Tsujiuchi Y, (2002) et al. The effect of Qi-gong relaxation exercise on the control of type 2 diabetes mellitus: a randomized controlled trial. Diacare 25: 241-242.
- Liu X, Miller YD, Burton NW, Brown WJ (2010) A preliminary study of the effects of Tai Chi and Qigong medical exercise on indicators of metabolic syndrome, glycaemic control, health-related quality of life, and psychological health in adults with elevated blood glucose. Br J Sports Med 44: 704-709.
- Liu X, Miller YD, Burton NW, Chang JH, Brown WJ (2011) Qi-Gong Mind-Body therapy and Diabetes Control- A Randomized Controlled Trial. Am J Prev Med 41: 152-158.
- Lee MS, Chen KW, Choi TY, Ernst E (2009) Qigong for type 2 diabetes care: a systematic review. Complement Ther Med 17: 236-242.
- Xin L, Miller YD, Brown WJ (2007) A qualitative review of the role of qigong in the management of diabetes. J Altern Complement Med 13: 427-433.
- Putiri AL, Lovejoy JC, Gillham S, Sasagawa M, Bradley R, et al. (2012) Psychological effects of Yi Ren Medical Qigong and progressive resistance training in adults with type 2 diabetes mellitus: a randomized controlled pilot study. Altern Ther Health Med 18: 30-34.
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, et al. (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28: 412-419.