Journal of Clinical and Investigative Dermatology
Download PDF
Case Report
*Address for Correspondence: Kelly K. Park, Division of Dermatology, Loyola University Medical Center, Building 54, Room 1012160 S, First Avenue, Maywood, IL 60153, USA, Tel: 708-216-6533; Fax: 877-991-4957; E-mail: kyunghwamd@gmail.com
Citation: Park KK, Hagstrom E, Berrios R, Tung RC. A Novel Purse-String Suture and Dehydrated Human Amnion/Chorion Membrane Allograft Closure Technique for the Repair of Defects Following Mohs Micrographic and Excisional Surgery. J Clin Investigat Dermatol. 2016;4(1): 3.
Copyright © 2016 Park KK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Investigative Dermatology | ISSN: 2373-1044 | Volume: 4, Issue: 1
Submission: 25 March, 2016| Accepted: 29 March, 2016 | Published: 02 April, 2016
The unique characteristics, needs, and preferences of the elderly undergoing Mohs micrographic (MMS) and excisional surgery can be barriers to subsequent repair and reconstruction, particularly when presented with large surgical defects and burdensome wound care.
A Novel Purse-String Suture and Dehydrated Human Amnion/Chorion Membrane Allograft Closure Technique for the Repair of Defects Following Mohs Micrographic and Excisional Surgery
Kelly K. Park1*, Erika Hagstrom2, Ricardo Berrios3 and Rebecca C. Tung1
- 1Division of Dermatology, Loyola University Medical Center, Building 54, Room 101 2160 S, First Avenue, Maywood, IL 60153, USA
- 2Department of Medicine, Loyola University Medical Center, Maywood, Illinois, USA
- 3Brandon Dermatology, Brandon, Florida, USA
*Address for Correspondence: Kelly K. Park, Division of Dermatology, Loyola University Medical Center, Building 54, Room 1012160 S, First Avenue, Maywood, IL 60153, USA, Tel: 708-216-6533; Fax: 877-991-4957; E-mail: kyunghwamd@gmail.com
Citation: Park KK, Hagstrom E, Berrios R, Tung RC. A Novel Purse-String Suture and Dehydrated Human Amnion/Chorion Membrane Allograft Closure Technique for the Repair of Defects Following Mohs Micrographic and Excisional Surgery. J Clin Investigat Dermatol. 2016;4(1): 3.
Copyright © 2016 Park KK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical & Investigative Dermatology | ISSN: 2373-1044 | Volume: 4, Issue: 1
Submission: 25 March, 2016| Accepted: 29 March, 2016 | Published: 02 April, 2016
Keywords
Mohsmicrographic surgery; Purse string; Repair; Dehydrated human amniotic/chorionic membrane allograft (dHACM); Pulsed dye laser (PDL)The unique characteristics, needs, and preferences of the elderly undergoing Mohs micrographic (MMS) and excisional surgery can be barriers to subsequent repair and reconstruction, particularly when presented with large surgical defects and burdensome wound care.
Four elderly patients with multiple comorbidities, polypharmacy, and social issues requested surgical management of sizeable, symptomatic skin cancers: basal cell carcinomas (BCC), squamous cell carcinoma (SCC), and melanoma. All patients desired closure methods that would avoid extensive reconstruction and minimize wound care responsibilities. In this retrospective case series, we investigated outcomes, cosmesis, and ease of wound care following reconstruction with combination of purse-string suture and single application dehydrated human amnion/chorion membrane allograft (dHACM) closure technique for the repair of MMS and excisional surgery defects in a medically fragile patient population.
Case 1
An 84-year-old male with chronic lymphocytic leukemia on bendamustine and history of laryngeal SCC presented with a bleeding infiltrative BCC of the left temporal scalp. Four MMS stages were required to clear the tumor margins, yielding and an 18 cm2 defect. Partial closure of the tips reduced the defect size to 7.2 cm2.A central purse-string further minimized defect to 2.0 cm2. A dHACM (EpiFix®, MiMedx Group, Inc., Marietta, GA) was applied to the site. At three weeks, one treatment with low-level pulsed dye laser (PDL, Vbeam®, Syneron Candela, Wayland, MA) was performed. Complete healing was noted at five weeks.
Case 2
An 85-year-old female with history of metastatic nasal BCC on antiplatelet therapy presented with a painful nodular and infiltrative BCC on the occipital scalp. Three MMS stages were necessary to clear the tumor, leaving a defect measuring 15.0 cm2. The wound edges were cinched using the purse string technique to a size of 4.4 cm2. This was covered with dHACM. After three weeks, the patient began a series of four weekly low-level PDL treatments. Complete reepithelialization was noted at six weeks.Case 3
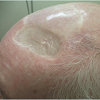
A 101-year-old caregiver-dependent male with extensive cardiac history on fish oil and aspirin presented with a painful SCC on the right dorsal hand. Two MMS stages were necessary to clear tumor, leaving a defect of 10.5 cm2 (Figure 1). Purse-string technique was used to decrease the final defect to 3.74 cm2. A dHACM was placed in the wound bed. Three weeks afterwards, four weekly low-level PDL treatments were performed. Complete healing was seen six weeks (Figure 2).Case 4
An 80-year-old male with a history of quiescent metastatic melanoma with significant cardiac history on garlic, vitamin E, and omega-3 fatty acids opted for wide local excision down to the fascia for a growing recurrent melanoma of the scalp (Breslow depth 1.85 mm). The final defect measured 7.28 cm2 (Figure 3). The dermis was cinched with a purse string suture to a size of 3.4 cm2 and dHACM was placed centrally. At three weeks, two low-level PDL treatments were performed a week apart. Near complete reepithelialization was seen at six weeks and complete healing at nine weeks (Figure 4).Technique
Following tumor extirpation, patients had sizable defects that were unsuitable for primary closure. In all cases, a subcuticular pursestring suture using absorbable suture material was placed to partially close the defect.Absorbable suture was passed as a running stitch in and out along the dermal edge of the circular wound in such a way that the two ends could be drawn tightly and secured with a knot, effectively reducing wound areas by 53.3-72.2% in each case.
To the resulting smaller central defect, a trimmed allograft was placed and moistened with normal saline used to promote adherence, assist with hemostasis, reduce pain and accelerate epithelialization.
A sterile pressure dressing was applied and left intact between wound care visits. Surgical sites were assessed at 1-2 week intervals to determine cosmetic outcomes, scar satisfaction, healing time, and adverse events. Low-intensity 595 nm PDL (settings ranged from 5-7 mm spot size, 7-7.5 joules, and 6 m sec pulse duration) was performed after three weeks to enhance healing and maximize cosmesis.
Discussion
All defects rapidly healed without complications and patients were pleased with their outcomes. Rationale for employing both surgical and allograft methods of reconstruction stemmed from the goal to facilitate wound healing.Cohen et al. observed that cuticular purse-string suture alone can partially or fully close defects and decrease defect size by an average of 60% [1]. This repair method is fast, distributes wound tension, provides hemostasis, and minimizes healing duration whilemaintaining function and providing excellent scar outcomes [1]. A randomized trial demonstrated via patient report that purse-string closures healed faster than secondary intention (5.62 weeks vs. 7.43 weeks) [2]. It is a reliable closure method for patients on anticoagulant and antiplatelet agents and reasonable alternative to flap or graftclosure [1].
When compared to secondary intention healing after MMS or excisional surgery, a bi-layered tissue-engineered, foreskin-derived biological dressing produced more pliable and less vascular scars that were more cosmetically acceptable [3]. Similarly, dHACM has been shown to facilitate overall healing in wounds refractory to aggressivemanagement and reduces healing times [4]. These allografts attenuate wound inflammation, have antibacterial activity, and posses scar andpain reduction properties [3]. These characteristics are thought to be due to its composition of basement membrane layers, cytokines, intrinsic factor, and secretion of angiogenic factors [3].
Prior successful use of dHACM in combination with low intensity PDL was also reported in an immunosuppressed patient who underwent MMS for SCC complicated by infection [5]. The adjuvant use of PDL as low-level laser therapy was utilized in this report and series for its antimicrobial and potential wound healing properties [3].
Conclusion
The use of combination purse-string suture and dHACM closure technique for reconstruction of surgical defects following micrographic or excisional surgery led to high patient satisfaction, excellent cosmetic outcomes, acceptable healing times, and lowwound care burden. This closure method may be a consideration for the repair of cutaneous surgical defects in select medically challenged patient populations.Acknowledgements
We would like to thank the MiMedx Group, Inc. for their in-kind donation of Epifix® product.References
- Cohen PR, Martinelli PT, Schulze KE, Nelson BR (2007) The cuticular purse string suture: a modified purse string suture for the partial closure of round postoperative wounds. Int J Dermatol 46: 746-753.
- Joo J, Custis T, Armstrong AW, King TH, Omlin K, et al. (2015) Purse-string suture vs second intention healing: results of a randomized, blind clinical trial. JAMA Dermatol 151: 265-270.
- 3. Gohari S, Gambla C, Healey M, Spaulding G, Gordon KB, et al. (2002) Evaluation of tissue-engineered skin (human skin substitute) and secondary intention healing in the treatment of full thickness wounds after Mohs micrographic or excisional surgery. Dermatol Surg 28: 1107-1114.
- Sheikh ES, Sheikh ES, Fetterolf DE (2014) Use of dehydrated human amniotic membrane allografts to promote healing in patients with refractory non healing wounds. Int Wound J 11: 711-717.
- Fancher W, Desai S, Peterson A, Tung R (2015) Aggressive squamous cell carcinoma within a burn scar complicated by M. fortuitum infection: combination treatment with antibiotic therapy, mohs surgery, amnion-chorion graft, and low-intensity pulsed dye laser. Dermatol Surg 41: 1079-82.