Journal of Andrology & Gynaecology
Download PDF
Research Article
*Address for Correspondence: Darius A. Paduch, M.D, Ph.D., Department of Urology, Weill Cornell Medical College, 520 E 70th St Starr 900, New York, NY 10065, USA, Tel: 212-746-5455; E-mail: dap2013@med.cornell.edu
Citation: Lee DJ, Dabaja AA, Kapoor V, Paduch DA. Association of the Force of Ejaculation and Orgasm Satisfaction using Novel Assessment Yools: Prospective Trial in Healthy Men. J Androl Gynaecol. 2014;2(3): 4.
Copyright © 2014 Lee DJ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN 2332-3442 | Volume: 2, Issue: 3
Submission: 01 September 2014 | Accepted: 25 September 2014 | Published: 27 September 2014
Association of the Force of Ejaculation and Orgasm Satisfaction using Novel Assessment Tools: Prospective Trial in Healthy Men
Daniel J. Lee1, Ali A. Dabaja1,2, Victor Kapoor2, Darius A. Paduch1*
- 1Department of Urology, Weill Cornell Medical College, New York, NY, USA
- 2Department of Urology, Henry Ford Health System, Detroit, MI, USA
*Address for Correspondence: Darius A. Paduch, M.D, Ph.D., Department of Urology, Weill Cornell Medical College, 520 E 70th St Starr 900, New York, NY 10065, USA, Tel: 212-746-5455; E-mail: dap2013@med.cornell.edu
Citation: Lee DJ, Dabaja AA, Kapoor V, Paduch DA. Association of the Force of Ejaculation and Orgasm Satisfaction using Novel Assessment Yools: Prospective Trial in Healthy Men. J Androl Gynaecol. 2014;2(3): 4.
Copyright © 2014 Lee DJ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Andrology & Gynaecology | ISSN 2332-3442 | Volume: 2, Issue: 3
Submission: 01 September 2014 | Accepted: 25 September 2014 | Published: 27 September 2014
Abstract
Background: Orgasmic and ejaculatory disorders affect hundreds of thousands of men worldwide, but remain poorly understood and studied. No validated and reproducible tools are available to assess orgasmic satisfaction. In addition, little is known about the relationships between orgasmic quality and ejaculatory force. We therefore performed a prospective trial to characterize orgasmic satisfaction and ejaculatory force.Methods: Fifty healthy subjects with no evidence of orgasmic, erectile, and ejaculatory dysfunction participated in the study. A 10-point self-assessment scale was used to rate the quality of the orgasm (median orgasm satisfaction score). The force of ejaculation used a 4-point scale based off of the distance traveled while lying supine: 0 for no ejaculate, 1 overflow, 2 below the umbilicus, and 3 above the umbilicus.
Results: Overall, the median age was 37 years (range 18-65). Twenty-seven (54%) had a median grade 3 force of ejaculation, while 16 (32%) had a grade 2, and 7 (14%) had a grade 1 force of ejaculation. Sixty-two percent (31/50) were a complete match on all three graded ejaculation samples, with 98% (49/50) were a complete match or differed by only one point. The median orgasm satisfaction score was 8 (IQR 6-9). Those who had a median grade 3 ejaculatory force had significantly higher scores of orgasm satisfaction than grade 2 or grade 1 (p=0.03).
Conclusion: Ejaculatory and orgasmic dysfunctions are prevalent but poorly characterized aspects of sexual dysfunction. Ejaculatory force was found to be associated with orgasmic satisfaction in a cohort of healthy participants. A scale for ejaculatory force was created and found to be easily utilized and reliable that can potentially be used for future studies. The development of better evaluation tools can help improve the treatment of ejaculatory and orgasmic disorders.
Keywords
Ejaculatory dysfunction; Orgasmic dysfunction; AssessmentIntroduction
Male sexual function depends on the complex interaction of multiple dimensions of human sexuality: arousal, sexual desire, orgasm, erectile function, and ejaculation. Sexual dysfunction is often multi- dimensional that occurs as a spectrum of disorders involving any or a combination of these factors [1]. Sexual dysfunction is a common problem in males with 35% of men aged 40 to 70 years experiencing moderate to complete erectile dysfunction [2], and in an analysis of more than 3000 individuals, 31% of men reported some sexual dysfunction [3].Major advances have been made in understanding the neurovascular mechanisms of sexual response and function in men [4,5], with the development of several drugs for the treatment of erectile dysfunction [6]. Ejaculatory dysfunction, which includes a spectrum of disorders such as premature ejaculation, delayed ejaculation, an ejaculation, painful ejaculation, retrograde ejaculation, and diminished volume or force of ejaculation, is an important public health problem that is often comorbid with erectile dysfunction and orgasmic dysfunction [7]. Premature ejaculation can be a frequent source of distress and sexual dissatisfaction [8,9]; one study of 1,463 females found that poor ejaculatory control contributed up to 23% of their relationship terminations [10]. It is estimated that 10-20% of men will have delayed ejaculation or an ejaculation [11,12], with 20-40% of men experiencing ejaculatory dysfunction at some point in their lives [13].
Although ejaculatory dysfunction is prevalent, it has not been wellcharacterized or evaluated. Delayed ejaculation and an ejaculation do not have separate classifications in the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) or billing ICD-9 codes, making the study of their effects in the population difficult. There are currently no standardized assessments of ejaculatory function, and little is known about the relationship between ejaculatory force and orgasm satisfaction. This study sought to evaluate the association between ejaculatory force and orgasm satisfaction using a standardized assessment.
Material and Methods
Patient populationAfter institutional board approval, 50 healthy men between the ages of 18 and 65 were recruited for the study. Participants were recruited through advertisements in New York, New Jersey, and Connecticut from 2008 to 2009. All patients were paid $200 to cover time and travel expenses. Inclusion criteria included normal self- reported erectile function, ejaculatory function, and orgasmic function, not taking prescribed or over-the-counter medication, ability to ejaculate in the supine position, normal voiding function, no psychiatric disorders, and ability to sign consent. Exclusion criteria included any sexual dysfunction, inability to ejaculate through masturbation, delayed puberty, and any currently used medications.
Measures
Participants completed questionnaires of orgasmic, erectile, and ejaculatory function (see Appendix A). Background information included age, their ages of puberty, first intercourse, and first masturbation, as well as median times to ejaculation during intercourse and masturbation. Participants completed the International Prostate Symptom Score (IPSS) and the International Index of Erectile Function (IIEF) questionnaire.
Participants were asked to masturbate 3 times at home while supine, with at least 2 days in between each trial, and record the force of ejaculation and satisfaction of orgasm. The force of ejaculation was graded on a four-point scale: 0-no ejaculation (grade 0), 1-overflow (grade 1), 2-below the umbilicus (grade 2), 3-above the umbilicus (grade 3) (see Figure 1). Orgasm satisfaction was graded on a tenpoint scale: 0-no sensation and 10-most satisfied. The median scores of the 3 measurements for the force of ejaculation and satisfaction of orgasm were then used for statistical comparisons. The median orgasm satisfaction scores were then analyzed as a categorical value, with scores 0 to 6 being lower satisfaction, 7 to 8 moderate satisfaction, and 9 to 10 high satisfaction. Participants also scored their satisfaction with their current or most recent sexual relationship on a 5-point scale, 1-dissatisfaction, 3-neutral, 5-extreme satisfaction.
Results
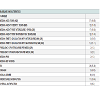
Clinical characteristicsOverall, the median age was 37 years (range 18-65), with a median IPSS score of 2 (IQR 1-3, see Table 1). The median erectile function IIEF score was 29 (IQR 25-30), median orgasmic IIEF score was 10 (IQR 9-10), median sexual desire score was 9 (IQR 8-10), median intercourse satisfaction score was 11 (IQR 10-14), and median overall satisfaction score was 8 (IQR 8-9). The median age of puberty was 12 years (IQR 11-13), median age of first masturbation was 12 (11-14), and median age of first sexual intercourse was 17 (IQR 15-19). The median time to ejaculation during masturbation was 5 minutes (IQR 3.5-11), and 10 minutes (IQR 5-15) during sexual intercourse. The median frequency of masturbation was 3 times per week (IQR 2-5), and median frequency of intercourse was 2 times per week (IQR 1-3).
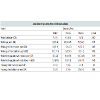
Overall, twenty-seven (54%) had a median grade 3 force of ejaculation, while 16 (32%) had a grade 2 force of ejaculation, and 7 (14%) had a grade 1 force of ejaculation. Sixty-two percent (31 / 50) were a complete match on all three graded ejaculation samples, with 98% (49 / 50) were a complete match or differed by only one point. The median orgasm satisfaction score was 8 (IQR 6-9). Fifteen (30%) had a high median satisfaction score, 21 (42%) had a moderate satisfaction score, and 14 (28%) had a lower satisfaction score.
Those who had a median grade 3 ejaculatory force had significantly higher scores of orgasm satisfaction than grade 2 or grade 1 (see Table 2, p=0.03). There were no significant associations between ejaculatory force with age, age at first intercourse or first masturbation, time to ejaculation, satisfaction with relationship, or frequency of masturbation or intercourse (all p>0.05). There were no associations between clinical variables and the relative satisfaction with orgasm.
Discussion
Ejaculatory and orgasm dysfunction are prevalent conditions and public health issues [3,7]; however, there is a paucity of literature and standardized assessments to evaluate those disorders. The present study indicates a reliable and reusable tool that can assess the force of ejaculation. The 4-point scale is a fixed anatomic scale that can be easily remembered by participants and can be utilized for future clinical trials to evaluate ejaculatory dysfunction, as well as assessing the relative success of different pharmacologic treatment or behavioral modifications.Arousal, orgasm, and ejaculatory function are highly integrated and coordinated processes, and disorders in these categories often coexist. In a study of 12,130 patients with erectile dysfunction, Paduch et al. found that 57.8% and 64.4% of the men reported ejaculatory and orgasmic dysfunction, respectively, and that increasing erectile dysfunction severity was associated with increased rates of ejaculatory and orgasmic dysfunction. In this current study, the level of satisfaction with orgasm was associated with the degree of ejaculatory force in this cohort of healthy men. This finding provides a baseline for future studies to measure the impact of ejaculatory or orgasmic dysfunction on the quality of life, and for further prospective clinical trials to evaluate the treatment of orgasmic or ejaculatory dysfunction.
In healthy men, arousal and/or physical stimulation will cause parasympathetic discharge and nitric oxide release causing cavernosal artery smooth muscle relaxation and increased venous outflow resistance [2]. Recent investigations have highlighted the importance of spinal central pattern generators (CPG) that modulate sensory and proprioceptic signals, including signals from the dorsal nerve of the penis, to initiate ejaculation by sympathetic discharge through the pudendal nerve to visceral organs such as the vas deferens, prostate, and seminal vesicles, smooth muscles of the bladder neck, and to the striated bulbospongiosus and ischiocavernosus muscles. This study highlights the spinal coordination at the CPGs, as the force of ejaculation was found to be highly precise and reproducible when measured multiple times in similar external conditions. Our tools to evaluate ejaculatory force or function may be used in future studies to further evaluate the response of CPGs.
Although this study was performed in healthy males with no stated sexual dysfunction, we noted that there was some heterogeneity in the level of orgasmic satisfaction, which highlights the prevalence of orgasmic and ejaculatory dysfunction in the general population. This also emphasizes the need for further trials, especially with the increased use of medications such as selective serotonin receptor inhibitors, antipsychotics, tricyclic antidepressants that can affect sexual function [7,13].
Several limitations of this study should be considered. The study was prospective in design, but utilized subjective measures of orgasm. We attempted to limit the potential bias by having each participant masturbate in similar environments each time and immediately record the level of satisfaction with orgasm on a ten point scale. Another potential limitation is a possible recall bias; as patients were asked to recall their relative time to ejaculation during intercourse and masturbation. Although we attempted to limit these issues, future studies are needed to confirm the findings of this study and further evaluate the impact of ejaculatory and orgasmic dysfunction in a prospective fashion.
Conclusion
Ejaculatory and orgasmic dysfunctions are prevalent but poorly characterized aspects of sexual dysfunction. Ejaculatory force was found to be associated with orgasmic satisfaction in a cohort of healthy participants. No tools exist to evaluate ejaculatory function or force, so a scale for ejaculatory force was created and found to be easily utilized and reliable that can potentially be used for future studies. The development of better evaluation tools can help improve the treatment of ejaculatory and orgasmic disorders.References
- Derogatis LR, Melisaratos N (1979) The DSFI: a multidimensional measure of sexual functioning. J Sex Marital Ther 5: 244-281.
- Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB (1994) Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol 151: 54-61.
- Laumann EO, Paik A, Rosen RC (1999) Sexual dysfunction in the United States: prevalence and predictors. JAMA 281: 537-544.
- Burnett AL (1995) Role of nitric oxide in the physiology of erection. Biol Reprod 52: 485-489.
- Rajfer J, Aronson WJ, Bush PA, Dorey FJ, Ignarro LJ (1992) Nitric oxide as a mediator of relaxation of the corpus cavernosum in response to nonadrenergic, noncholinergic neurotransmission. N Engl J Med 326: 90-94.
- Boolell M, Gepi-Attee S, Gingell JC, Allen MJ (1996) Sildenafil, a novel effective oral therapy for male erectile dysfunction. Br J Urol 78: 257-261.
- Paduch DA, Bolyakov A, Beardsworth A, Watts SD (2012) Factors associated with ejaculatory and orgasmic dysfunction in men with erectile dysfunction: analysis of clinical trials involving the phosphodiesterase type 5 inhibitor tadalafil. BJU Int 109: 1060-1067.
- Patrick DL1, Althof SE, Pryor JL, Rosen R, Rowland DL, et al. (2005) Premature ejaculation: an observational study of men and their partners. J Sex Med 2: 358-367.
- Rowland D1, Perelman M, Althof S, Barada J, McCullough A, et al. (2004) Self-reported premature ejaculation and aspects of sexual functioning and satisfaction. J Sex Med 1: 225-232.
- Burri A, Giuliano F, McMahon C, Porst H. (2014) Female Partner’s Perception of Premature Ejaculation and Its Impact on Relationship Breakups, Relationship Quality, and Sexual Satisfaction. J Sex Med 11: 2243-2255.
- Nathan SG (1986) The epidemiology of the DSM-III psychosexual dysfunctions. J Sex Marital Ther 12: 267-281.
- Delavierre D ( 2008) [Diagnosis of male anorgasmia]. Prog Urol 18: F8-10.
- Rosen RC, Lane RM, Menza M (1999) Effects of SSRIs on sexual function: a critical review. J Clin Psychopharmacol 19: 67-85.